Thoracic outlet syndrome
Template:DiseaseDisorder infobox
For patient information click here
Editor(s)-In-Chief: Robert G. Schwartz, M.D. [1], Piedmont Physical Medicine and Rehabilitation, P.A.; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Thoracic outlet syndrome (TOS) consists of a group of distinct disorders that affect the nerves in the brachial plexus (nerves that pass into the arms from the neck) and various nerves and blood vessels between the base of the neck and axilla (armpit). While traditionally thought of as a sensory-motor neurovascular disorder that is due to a mechanical or compressive source clinical evidence also exits that suggests the sympathetic portion of the nervous system is frequently involved. This is at least one explanation for the poor outcomes seen with a surgical treatment approach.
Epidemiology
TOS is more common in women. The onset of symptoms usually occurs between 20 and 50 years of age.
Causes
For the most part, these disorders are thought to be produced by compression of the components of the brachial plexus (the large cluster of nerves that pass from the neck to the arm), the subclavian artery, the subclavian vein or are sympathetically mediated. These subtypes are referred to as neurogenic TOS, arterial TOS, and venous TOS, respectively. The compression may be positional (caused by movement of the clavicle (collarbone) and shoulder girdle on arm movement) or static (caused by abnormalities or enlargement of the various muscles surrounding the arteries, veins and brachial plexus).
The neurogenic form of TOS accounts for 95 to 98% of all cases of TOS. The sympathetic nervous system is felt to be the most common neurogenic source.
It is known from pathological studies of cadavers, and from surgical studies of patients with TOS, that there are numerous anomalies of the scalene muscles and the other muscles that surround the arteries, veins and brachial plexus. TOS may result from these anomalies of the scalene muscles or from enlargement (hypertrophy) of the scalene muscles. One common cause of hypertrophy is trauma, as may occur in motor vehicle accidents.
The two groups of people most likely to develop TOS are those suffering neck injuries in motor vehicle accidents and those who use computers in non-ergonomic postures for extended periods of time. Young overhead athletes (such as swimmers, volleyball players and baseball pitchers) and musicians may also develop thoracic outlet syndrome, but significantly less frequently than the two large groups above.
Classification
Old Classification
The following taxonomy of TOS is used in ICD-9-CM and other sources:
- Scalenus anticus syndrome (compression on brachial plexus and/or subclavian artery caused by muscle growth) - diagnosed by using Adson's sign with patient's head turned outward
- Cervical rib syndrome (compression on brachial plexus and/or subclavian artery caused by bone growth) - diagnosed by using Adson's sign with patient's head turned inward
- Costoclavicular syndrome (narrowing between the clavicle and the first rib) -- diagnosed with costoclavicular maneuver[1]
New Classification
- Neurogenic TOS has a characteristic sign, called the Gilliatt-Sumner hand, in which there is severe wasting in the fleshy base of the thumb. There may be numbness along the underside of the hand and forearm, or dull aching pain in the neck, shoulder, and armpit. When the sympathetic nervous system is involved, there may be skin temperature and skin color changes. Findings are most predominant in the medial aspect of the arm, all the way down to the fifth finger.
- Vascular TOS features pallor, a weak or absent pulse in the affected arm, which also may be cool to the touch and appear paler than the unaffected arm. Symptoms may include numbness, tingling, aching, and heaviness.
- Non-specific TOS most prominently features a dull, aching pain in the neck, shoulder, and armpit that gets worse with activity. Non-specific TOS is frequently triggered by a traumatic event such as a car accident or a work related injury. It also occurs in athletes, including weight lifters, swimmers, tennis players, and baseball pitchers.
Symptoms
- Arterial thoracic outlet syndrome can present with pallor, coldness, pain, and paresthesias of the fingers due to severe ischemia.
- Venous form (aka Paget-Schroetter syndrome, Effort thrombosis and thoracic inlet syndrome) presents with arm swelling and pain.
Diagnosis of Thoracic Outlet Syndrome should be Distinguished from
- Acute coronary syndrome
- Brachial plexitis
- Carpal tunnel syndrome
- Cervical disc disorders (e.g., cervical spondylitis)
- Complex regional pain syndrome
- Reflex Sympathetic Dystrophy
- Fibromyalgia
- Mediastinal venous obstruction (e.g., Pancoast tumor)
- Multiple sclerosis
- Postural palsy
- Raynaud's disease
- Rotator cuff injuries
- Spinal cord injuries
- Spinal cord neoplasms
- Superficial thrombophlebitis
- Trauma
- Tumors of the syrinx
- Ulnar nerve compression at the elbow
- Vasculitis
- Vasospastic disorder
Diagnosis
- Adson's sign and the costoclavicular maneuver are notoriously inaccurate, and may be a small part of a comprehensive history and physical examination of a patient with TOS. There is currently no single clinical sign that makes the diagnosis of TOS with certainty.
- Cervical radiography
- Chest radiography is helpful to evaluate:
- Presence of cervical or first rib
- Clavicle deformity
- Pulmonary disease
- Pancoast tumor
- Color flow duplex scanning
- Nerve conduction studies, electromyography, or imaging studies are recommended to confirm or rule out a diagnosis of TOS.
- Nerve conduction evaluation via root stimulation and F wave is the best direct approach to evaluation of neurologic TOS.
- Electromyography (EMG) is unreliable and does not provide objective evidence of TOS, however it is frequently used to rule out other disorders such as C8 radiculopathy.
- Cervical myelogram
- CT scan
- MRI [2]
- Arteriography, while only rarely used to evaluate thoracic outlet syndrome, may be used if a surgery is being planned to correct an arterial TOS.[3]
- Arteriography indications:
- Evidence of peripheral emboli in the upper extremity
- Suspected subclavian stenosis or aneurysm (e.g., bruit or abnormal supraclavicular pulsation)
- Blood pressure differential greater than 20 mmHg
- Obliteration of radial pulse during EAST
- Venography
- Venography indications:
- Persistent or intermittent edema of the hand or arm
- Peripheral unilateral cyanosis
- Prominent venous pattern over the arm, shoulder, or chest
- Thermography indications:
- Vasomotor or sudomotor instability
- Weather sensitivity
- Cold limb in a shawl or C8 distribution
- Thermography may be one of the most sensitive tests to objectify the presence of thoracic outlet syndrome, especially if it is felt to be sympathetic in origin
Diagnostic Findings
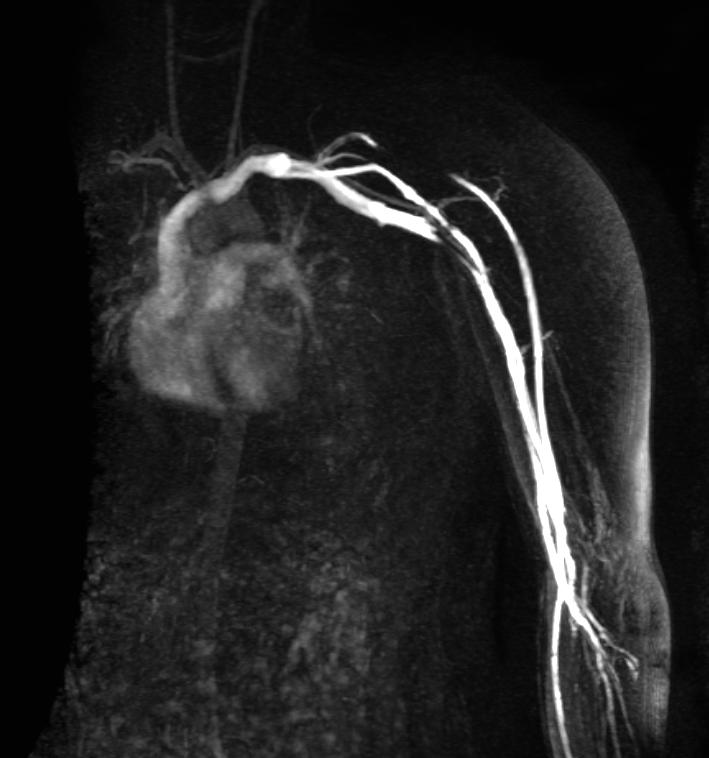
MRV demonstrates severe focal stenosis of the left subclavian vein only when the patient's arm is overhead.
-
MIP
-
3D MRV
-
MIP
-
3D MRV
Treatment
Often, continued and active postural changes along with physiotherapy, massage therapy, chiropractic or osteopathic manipulation, will suffice. The recovery process however is long term, and a few days of poor posture can often set one back. Various anesthetic injections, such as cervical plexus block and stellate ganglion block can provide significant relief.
About 10 to 15% of patients undergo surgical decompression following an appropriate trial of conservative therapy, most often specific physical therapy directed towards the treatment of thoracic outlet syndrome, and usually lasting between 6 and 12 months. Surgical treatment may include removal of anomalous muscles, removal of the native anterior and/or middle scalene muscles, removal of the first rib or, if present, a cervical rib, or neurolysis (removal of fibrous tissue from the brachial plexus).
In general;
- Treatment of arterial thoracic outlet syndrome is surgical intervention. Treatment is required to treat or prevent acute thromboembolic events.
- Treatment of venous thoracic outlet syndrome depends primarily on the presence and extent of associated venous thrombosis and may include anticoagulation, thrombolysis, or surgical decompression.
Noninvasive
- Stretching
The goal of self stretching is to relieve compression in the thoracic cavity, reduce blood vessel and nerve impingement, and realign the bones, muscles, ligaments, and tendons causing the problem.- Moving shoulders forward (hunching) then back to neutral, followed by extending them back (arching) then back to neutral, followed by lifting shoulders then back to neutral.
- Tilting and extending neck opposite to the side of injury while keeping the injured arm down or wrapped around the back.
- Nerve Gliding
This syndrome causes a compression of a large cluster of nerves, resulting in the impairment of nerves throughout the arm. By performing nerve gliding exercises one can stretch and mobilize the nerve fibers. Chronic and intermittent nerve compression has been studied in animal models, and has a well-described pathophysiology, as described by Susan Mackinnon, MD, currently at Washington University in St. Louis. Nerve gliding exercises have been studied by several authorities, including David Butler in Australia.- Extend your injured arm with fingers directly outwards to the side. Tilt your head to the otherside, and/or turn your head to the other side. A gentle pulling feeling is generally felt throughout the injured side. Initially, only do this and repeat. Once this exercise has been mastered and no extreme pain is felt, begin stretching your fingers back. Repeat with different variations, tilting your hand up, backwards, or downwards.
- Posture
TOS is rapidly aggravated by poor posture. Active breathing exercises and ergonomic desk setup can both help maintain active posture. Often the muscles in the back become weak due to prolonged (years) hunching. - Ice/Heat
Ice can be used to decrease inflammation of sore or injured muscles. Heat can also aid in relieving sore muscles by improving circulation to them. While the whole arm generally feels painful, some relief can be seen when ice/heat is applied to the thoracic region (collar bone, armpit, or shoulder blades).
Invasive
- Cortisone
Injected into a joint or muscle, cortisone can help relief and lower inflammation. - Botox injections
Short for Botulinum Toxin A, Botox binds nerve endings and prevents the release of neurotransmitters that activate muscles. A small amount of Botox injected into the tight or spastic muscles found in TOS sufferers often provides months of relief while the muscles is temporarily paralyzed. This noncosmetic treatment is unfortunately not covered by most medical plans and costs upwards of $400. Botox is VERY long-lasting, and its use will probably be based on results of ongoing research. Serious side effects have been reported, and are similarly long-lasting, so improved understanding of the mechanism of a 'scalene block' is vital to determining the benefit and risk of using Botox. - Surgical approaches have also been used.[4]
- Provocative test: The injection of a short-acting anesthetic such as xylocaine into the anterior scalene, subclavius, or pectoralis minor muscles as a provocative test to assist in the diagnosis of thoracic outlet syndrome. This is referred to as a 'scalene block'. If the patient experiences symptomatic relief for approximately 15 minutes following this procedure, surgical decompression is more likely to be successful in leading to the same level of symptomatic relief. However, this is not considered a 'treatment', as the relief is expected to wear off within an hour or two, at a maximum. Active research continues into the accuracy and risks of this provocative test.
Prognosis
The outcome for individuals with TOS varies according to type. The majority of individuals with TOS will improve with exercise and physical therapy. Vascular TOS, and true neurogenic TOS often require surgery to relieve pressure on the affected vessel or nerve.
References
- ↑ Template:FPnotebook
- ↑ Stepansky F, Hecht EM, Rivera R, Hirsh LE, Taouli B, Kaur M, Lee VS. Dynamic MR angiography of upper extremity vascular disease: pictorial review. Radiographics. 2008 Jan-Feb;28(1):e28. Epub 2007 Oct 29. PMID 17967936
- ↑ Thoracic outlet syndrome Mount Sinai Hospital, New York
- ↑ Rochkind S, Shemesh M, Patish H; et al. (2007). "Thoracic outlet syndrome: a multidisciplinary problem with a perspective for microsurgical management without rib resection". Acta Neurochir. Suppl. 100: 145–7. PMID 17985565.
Template:PNS diseases of the nervous system nl:Thoracic outlet syndrome