Histrelin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alberto Plate [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Histrelin is a endocrine-metabolic agent and gonadotropin releasing hormone agonist that is FDA approved for the treatment of children with central precocious puberty (CPP). Common adverse reactions include implant site reactions, gynecomastia, hot sweats, amenorrhea, erectile dysfunction and fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
There is limited information regarding Histrelin FDA-Labeled Indications and Dosage (Adult) in the drug label.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Histrelin in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Histrelin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Recommended Dose
- The recommended dose of Histrelin is one implant every 12 months. Each implant contains 50 mg histrelin acetate. The implant is inserted subcutaneously in the inner aspect of the upper arm and provides continuous release of histrelin (65 mcg/day) for 12 months of hormonal therapy. Histrelin should be removed after 12 months of therapy (the implant has been designed to allow for a few additional weeks of histrelin acetate release, in order to allow flexibility of medical appointments). At the time an implant is removed, another implant may be inserted to continue therapy. Discontinuation of Histrelin should be considered at the discretion of the physician and at the appropriate time point for the onset of puberty (approximately 11 years for females and 12 years for males).
Recommended Procedure for Implant Insertion and Removal
- This procedure section is intended to provide guidance for the insertion and removal of Histrelin. The actual procedure used, however, is at the discretion of the qualified healthcare provider performing the procedure.
- Insertion of a new implant can proceed using the following Suggested Insertion Procedure. If a previous Histrelin implant must first be removed, please see the Suggested Removal Procedure instructions below.
Suggested Insertion Procedure
- The supplies necessary to insert the implant, including the Insertion Tool and local anesthetic, are provided in a separate Implantation Kit that is shipped along with the implant. Please note that the implant should be kept refrigerated (2-8°C) in its sealed vial, pouch, and carton, until needed for the procedure. Once removed from refrigeration, the vial containing the implant (still in its unopened pouch and carton) may remain at room temperature for up to 7 days, if necessary, before being used. If not used in that time, the packaged implant may again be properly refrigerated until the expiration date on the carton.
NOTE: The Implantation Kit is to be stored at room temperature and should not be refrigerated. Insertion of the Histrelin implant is a surgical procedure. Sterile gloves and aseptic technique must be used to minimize any chance of infection.
Setting up the Sterile Field
- Using proper aseptic technique, the sterilized components of the Implantation Kit needed for the insertion procedure, including the Insertion Tool, are to be carefully dispensed from their packaging onto the Sterile Field drape (non-fenestrated) provided. Note That The Kit Box And All Packaging Are Not Sterile And Should Be Kept Off Of The Sterile Field Drape. Do Not Place The Vial Of Local Anesthetic Or The Vial Containing The Implant Onto The Drape as the exterior surface of these vials is not sterile.
- The implant vial should not be opened until just before the time of insertion. Open the vial by removing the metal band and carefully pour the sterile contents (implant and sterile saline) onto the Sterile Field drape. The implant can then be handled with sterile gloves or with the sterile mosquito clamp provided. AVOID bending or pinching the implant.
Preparing the Patient and the Insertion Site
- The patient should be on his/her back, ideally with the arm least used (e.g., left arm for a right-handed person) positioned, either bent or extended, so that the physician has ready access to the inner aspect of the upper arm. Propping the arm with pillows may help the patient more easily hold the position. The suggested optimum site for subcutaneous insertion is approximately half-way between the shoulder and the elbow, in line with the crease between the biceps and triceps muscles.
- Antiseptic: Swab the insertion area with topical antiseptic, then overlay with the fenestrated Sterile Field drape provided, so that the opening is over the insertion site (for clarity of illustration, the following images do not show the drape).

- Anesthetic: The method of anesthesia utilized (i.e., local, conscious sedation, general) is at the discretion of the healthcare provider.
- If local anesthesia is selected: a vial of sterile local anesthetic (note that the exterior of the vial is not sterile) has been provided along with a sterile hypodermic needle for injection. After determining the absence of known allergies to the anesthetic agent, inject anesthetic into the subcutaneous tissue, starting at the planned incision site, then infiltrating along the intended subcutaneous insertion path, up to the length of the implant (a little more than one inch). Local anesthesia may also be supplemented by the use of distraction techniques.

- The following sections describe the suggested procedure for insertion of the implant using the Insertion Tool provided. The method of insertion used, however, is at the discretion of the healthcare provider performing the procedure.
Loading the Insertion Tool
- The sterile Insertion Tool is comprised of a fixed handle attached to a retractable, bevel-tipped cannula, into the chamber of which the implant is to be placed for subcutaneous insertion. The cannula can be extended and retracted. The fully extended cannula contains a fixed piston upon which the implant, once inserted, rests. During the final step of the insertion procedure, the cannula will be retracted into the handle using the slide mechanism (green button), thereby exposing and leaving the implant to remain in the subcutaneous tissue.
- When first grasping the sterile Insertion Tool, confirm that the cannula is fully extended. Verify this by inspecting the position of the green retraction button. The button should be locked in position all the way forward, towards the cannula, farthest from the handle.

- The implant can be picked up using sterile gloves or with the sterile mosquito clamp provided. Avoid bending or pinching the implant. Note that the implant may come out of its vial slightly curved and/or partially flattened after refrigerated storage. To help make the implant more symmetrical prior to loading into the Tool, you can roll the implant a few times (while wearing a sterile glove) between the fingers and thumb.
- Insert the implant into the cannula of the Insertion Tool manually or using the mosquito clamp. When inserting the implant into the cannula, DO NOT FORCE the implant. If resistance is felt, the implant should be removed and manually manipulated or rolled as needed, and re-inserted into the cannula.

- When fully inserted, the implant rests inside the cannula so that just the tip of the implant is visible at the beveled end of the cannula.
Making the Incision
- Using the sterile scalpel provided, make an incision transverse to the long axis of the arm, and of a size adequate to allow the bore of the cannula to be inserted into the subcutaneous tissue. Be sure that the incision is positioned so that there is sufficient length of upper arm available to fit the implant easily within the intended insertion space.

Inserting the Implant
- It is suggested that insertion may be easier if a “pocket” for the implant is first created by blunt dissection through the incision, subcutaneously along the path of the anesthetic, using the cannula of the loaded Insertion Tool, or using a sterile hemostatic clamp or equivalent surgical tool.
- Be sure to VISIBLY RAISE THE SKIN (known as tenting) at all times during the pocket-making and insertion procedures to ensure correct subcutaneous placement (“just under the skin”) of the implant. Note that the cannula of the Insertion Tool, or whatever tool is being used to create the pocket, SHOULD NOT ENTER MUSCLE TISSUE. Deep insertion of the implant will not affect the performance of Histrelin but may cause difficulty in the later removal of the implant.
- If using the cannula of the loaded Insertion Tool to create the pocket, carefully insert the tip of the cannula into the incision and advance through the subcutaneous tissue, while visibly raising the skin along the length of the cannula up to, but no farther than, the inscribed black line on the cannula. DO NOT DEPRESS THE GREEN RETRACTION BUTTON ON THE TOOL WHILE INSERTING OR ADVANCING THE TOOL INTO THE INCISION.
- Pull the Tool back, almost to the beveled tip of the cannula, and advance the Tool forward again, so that the cannula re-enters the pocket completely, but no farther than the inscribed black line. Be sure to keep the insertion path just immediately subcutaneous.
- If another tool was used to create the pocket, now insert the loaded cannula of the Insertion Tool containing the implant through the incision, up to the inscribed black line.

- Hold the Insertion Tool in place with the base against the patient’s arm (if possible) as you carefully move your thumb to the green retraction button. Depress the button to release the locking mechanism, then slide the button back toward the handle until it stops, all the while holding the body of the Insertion Tool in place.

- Retracting the button causes the cannula to withdraw from the incision, leaving the implant in the subcutaneous tissue. DO NOT FURTHER ADVANCE THE CANNULA ONCE THE RETRACTION PROCESS HAS STARTED. Likewise, do not withdraw the Insertion Tool until the button is fully retracted or the implant may be pulled partially out of the incision. Once the retraction is complete, the Tool can be fully withdrawn.
NOTE: It may be helpful during the process of retraction and withdrawal of the cannula to apply pressure to the skin over the implant, to help ensure that the implant remains in the subcutaneous pocket.
- If there is a need to re-start the process at any time during the insertion procedure, withdraw the Insertion Tool, carefully extract the implant from the cannula and reset the retraction button on the Tool to its forward-most position. *Examine the implant before reloading the implant into the Insertion Tool, and start again.
- Placement of the implant should be confirmed by palpation. Note that the tip of a properly-placed implant may not be visible through the incision.
- After implantation, briefly cover the site with a sterile gauze pad and apply pressure to ensure hemostasis.
Closing the Incision
- To close the incision, you can use the absorbable sutures and/or the sterile adhesive surgical strips provided. To improve adhesion of the strips, you can apply benzoin tincture antiseptic (provided) to the skin, and let it dry, before applying the adhesive strips.

- Once closed, cover the incision site with sterile gauze pads and secure the dressing with the bandage provided.
- Please provide the patient’s parent or guardian with a Patient Information Leaflet, which includes information about the implant and instructions on proper care of the insertion site.
Suggested Removal Procedure
- Histrelin should be removed after 12 months of therapy. Most of the supplies necessary to remove the implant, including the local anesthetic and the sterile mosquito clamp, are provided in the Implantation Kit that is shipped along with a new Histrelin implant. Note that the Implantation Kit is to be stored at room temperature and must not be refrigerated. See the Suggested Insertion Procedure above for further instructions.
- Removal of the Histrelin implant is a surgical procedure. Sterile gloves and aseptic technique must be used to minimize any chance of infection.
- Setting up the Sterile Field: Using proper aseptic technique, the sterilized components of the Implantation Kit needed for the implant removal procedure are to be carefully dispensed from their packaging out onto the Sterile Field drape (non-fenestrated) provided. NOTE THAT THE KIT BOX AND ALL PACKAGING ARE NOT STERILE and should be kept off of the Sterile Field drape. DO NOT PLACE THE VIAL OF LOCAL ANESTHETIC ONTO THE DRAPE as the exterior surface of the vial is not sterile.
Preparing the Patient and the Site
- The patient should be on his/her back, with the arm containing the implant positioned, either bent or extended, so that the physician has ready access to the inner aspect of the upper arm. Propping the arm with pillows may help the patient more easily hold the position.
- The implant to be removed should first be located by palpating the inner aspect of the upper arm, near the incision from the prior year.

- Generally, the previous implant is readily palpated. In the event the implant is difficult to locate, ultrasound may be used. If ultrasound fails to locate the implant, other imaging techniques such as CT or MRI may be used to locate it (plain films are not recommended as the implant is not radiopaque).
- Antiseptic : Swab the area above and around the previous implant with topical antiseptic. Overlay the area with the fenestrated Sterile Field drape provided, so that the hole is over the previous insertion site (for clarity of illustration, the following images do not show the drape).

- Anesthetic: The method of anesthesia utilized (i.e., local, conscious sedation, general) is at the discretion of the healthcare provider.
If local anesthesia is selected: a vial of sterile local anesthetic (note that the exterior of the vial is not sterile) has been provided along with a sterile hypodermic needle for injection. After determining the absence of known allergies to the anesthetic agent, inject anesthetic into the subcutaneous tissue at and around the site of the intended incision (the site of the previous implant). Local anesthesia may also be supplemented by the use of distraction techniques.

Making the Incision and Removing the Implant
- Using the sterile scalpel provided, make an incision of a size adequate to allow the implant to be easily removed and, if a new implant will be inserted, large enough for the bore of the cannula of the Insertion Tool provided.

- Generally, the tip of the implant will be visible through the incision, possibly covered by a pseudocapsule of tissue. In order to facilitate the removal of the implant, it may be necessary to palpate the head of the implant through the incision using your smallest finger, especially if the head of the implant is not readily visible. In addition, you may need to push down on the distal end of the implant and “massage it forward” towards the incision.
- Carefully nick the pseudocapsule to reveal the polymer tip of the implant. It may be beneficial to insert the sterile mosquito clamp provided into the hole created in the pseudocapsule and expand by opening the clamp. Widening the opening of the pseudocapsule may ease the extraction of the implant.
- Gently but securely grasp the implant with the sterile mosquito clamp and extract the implant.

- Dispose of the implant in a proper manner, treating it like any other bio-waste.
- Briefly cover the site with a sterile gauze pad and apply pressure to ensure hemostasis.
- If inserting a new implant, see the Suggested Insertion Procedure instructions provided above. Note that you can insert the new implant into the same “pocket” as the removed implant, or make a new incision at a different site in the same arm or in the contralateral arm.
- If a new implant is not to be inserted, proceed to close the incision.
Closing the Incision
- To close the incision, you can use the absorbable sutures and/or the sterile adhesive surgical strips provided. To improve adhesion of the strips, you can apply benzoin tincture antiseptic (provided) to the skin, and let it dry, before applying the adhesive strips.

- Once closed, cover the incision site with sterile gauze pads and secure the dressing with the bandage provided.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Histrelin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Histrelin in pediatric patients.
Contraindications
- Histrelin is contraindicated in patients who are hypersensitive to gonadotropin releasing hormone (GnRH) or GnRH agonist analogs.
- Histrelin is contraindicated in females who are or may become pregnant while receiving the drug. Histrelin may cause fetal harm when administered to pregnant patients. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus. The possibility exists that spontaneous abortion may occur.
Warnings
Initial Agonistic Action
- Histrelin, like other GnRH agonists, initially causes a transient increase in serum concentrations of estradiol in females and testosterone in both sexes during the first week of treatment. Patients may experience worsening of symptoms or onset of new symptoms during this period. However, within 4 weeks of histrelin therapy, suppression of gonadal steroids occurs and manifestations of puberty decrease.
Implant Insertion/Removal Procedure
- Implant insertion is a surgical procedure and it is important that the insertion instructions are followed to avoid potential complications. The insertion and removal of the implant should be done aseptically. Proper surgical technique is critical in minimizing adverse events related to the insertion and the removal of the histrelin implant. On occasion, localizing and/or removal of implant products have been difficult and imaging techniques were used, including ultrasound, CT, or MRI (note: the histrelin implant is not radiopaque). In some cases the implant broke during removal and multiple pieces were recovered. Confirm that the entire implant has been removed. If the implant was not retrieved completely, the remaining pieces should be removed following the instructions in the Suggested Removal Procedure section. Rare events of spontaneous extrusion of the implant have been observed in clinical trials. During Histrelin treatment, patients should be evaluated for evidence of clinical and biochemical suppression of CPP manifestations (see SECTION 5.3, Monitoring and Laboratory tests). Detailed instructions on the insertion and removal procedures of the implant are provided above.
Monitoring and Laboratory Tests
- LH, FSH and estradiol or testosterone should be monitored at 1 month post implantation then every 6 months thereafter. Additionally, height (for calculation of height velocity) and bone age should be assessed every 6-12 months.
Adverse Reactions
Clinical Trials Experience
The most common adverse reactions with Histrelin involved the implant site. Local reactions after implant insertion include bruising, pain, soreness, erythema and swelling. During the early phase of therapy, gonadotropins and sex steroids rise above baseline because of the natural stimulatory effect of the drug. Therefore, an increase in clinical signs and symptoms may be observed
Adverse Reactions in Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
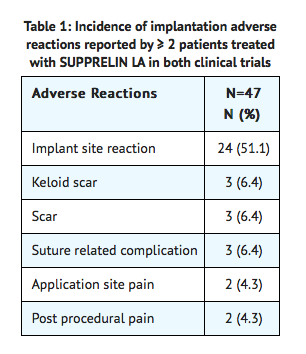
The safety of Histrelin in children with CPP was evaluated in two single-arm clinical trials conducted in a total of 47 patients (44 females and 3 males) over a period of time ranging from 9 to 18 months. The most commonly reported adverse reaction was implant site reaction, which was reported by 24 of 47 (51.1%) patients. Implant site reaction includes discomfort, bruising, soreness, pain, tingling, itching, implant area protrusion and swelling. Two subjects experienced a serious adverse reaction: 1 subject who coincidentally had Stargardt’s Disease experienced amblyopia and 1 subject had a benign pituitary tumor (pituitary adenoma). One subject discontinued the study due to an adverse reaction of infection at the implant site. There were no clinically meaningful findings in standard clinical hematology and chemistry tests and/or in vital signs. The incidence of implantation adverse events reported by more than 2 patients are summarized in Table 1.
The following adverse reactions were reported as possibly related or related in 1 patient each: wound infection, breast tenderness, dysmenorrhea, epistaxis, erythema, feeling cold, gynecomastia, headache, menorrhagia, migraine, mood swings, pituitary tumor benign, pruritus, weight increased, disease progression and influenza-like illness. The adverse reaction metrorrhagia was reported as possibly related or related in 2 patients.
Postmarketing Experience
The following adverse reactions have been identified during post approval use of Histrelin Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- General Disorders and Administration Site Conditions: implant breakage
- Nervous System Disorders: seizures
Drug Interactions
- Overview: No formal drug-drug, drug-food, or drug-herb interaction studies were performed with Histrelin.
- Drug-Laboratory Interactions: Therapy with Histrelin results in suppression of the pituitary-gonadal system. Results of diagnostic tests of pituitary gonadotropic and gonadal functions conducted during and after Histrelin therapy may be affected. Histrelin decreased mean serum insulin-like growth factor-1 (IGF-1) levels by approximately 11% in one study (Study 1). Histrelin increased the serum concentration of dehydroepiandrosterone (D
Use in Specific Populations
Pregnancy
- Histrelin is contraindicated in females who are, or may become, pregnant while receiving the drug. Histrelin can cause fetal harm when administered to a pregnant patient. The possibility exists that spontaneous abortion may occur.
- Animal Data: Major fetal abnormalities were observed in rabbits at 3 times human therapeutic exposure but not in rats after administration of histrelin acetate throughout gestation. There was dose-related increased fetal mortality during organogenesis in both rats given 1, 3, 5 or 15 mcg/kg/day (at less than therapeutic exposures using body surface area comparisons, based on a 65 mcg per day human dose) and in rabbits at 20, 50 or 80 mcg/kg/day (at 3 times human exposure using body surface area comparisons, based on a 65 mcg/day dose in humans).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Histrelin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Histrelin during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Histrelin in women who are nursing.
Pediatric Use
- Safety and effectiveness in pediatric patients below the age of 2 years have not been established. The use of Histrelin in children under 2 years is not recommended.
Geriatic Use
There is no FDA guidance on the use of Histrelin in geriatric settings.
Gender
There is no FDA guidance on the use of Histrelin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Histrelin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Histrelin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Histrelin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Histrelin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Histrelin in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Histrelin Administration in the drug label.
Monitoring
There is limited information regarding Histrelin Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Histrelin and IV administrations.
Overdosage
- There have been no reports of overdose in Histrelin clinical trials. High doses of histrelin acetate injection in animal studies were generally associated only with effects attributed to the expected pharmacology. The method of drug delivery makes accidental or intentional overdosage unlikely.
Pharmacology
| |
Histrelin
| |
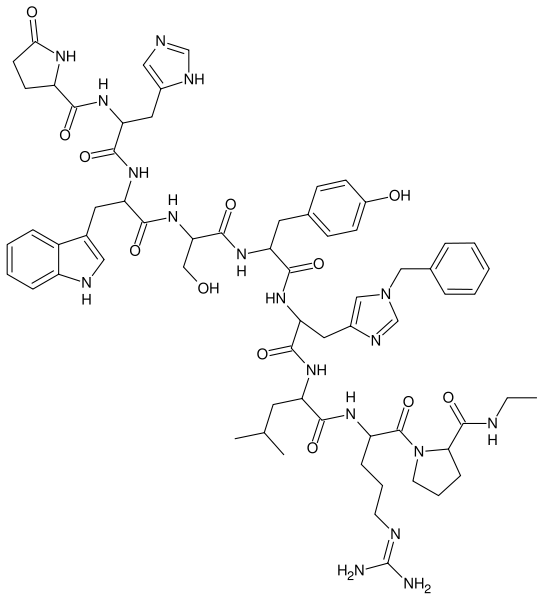
| Systematic (IUPAC) name | |
| 5-oxo-L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-1-benzyl-D-histidyl-L-leucyl-N5-(diaminomethylene)-L-ornithyl-N-ethyl-L-prolinamide | |
| Identifiers | |
| CAS number | |
| ATC code | L02 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 1323.5 g/mol |
| Pharmacokinetic data | |
| Bioavailability | 92% |
| Protein binding | 70% |
| Metabolism | Hepatic |
| Half life | 4.0 hours |
| Excretion | Undetermined |
| Therapeutic considerations | |
| Pregnancy cat. |
X(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Subcutaneous implant |
Mechanism of Action
- Histrelin is a GnRH agonist and an inhibitor of gonadotropin secretion when given continuously. It delivers approximately 65 mcg histrelin acetate per day. Both animal and human studies indicate that following an initial stimulatory phase, chronic, subcutaneous administration of histrelin acetate desensitizes responsiveness of the pituitary gonadotropin which, in turn causes a reduction in ovarian and testicular steroidogenesis.
- In humans, administration of histrelin acetate results in an initial increase in circulating levels of LH and FSH, leading to a transient increase in concentration of gonadal steroids (testosterone and dihydrotestosterone in males, and estrone and estradiol in premenopausal females).
- However, continuous administration of histrelin acetate causes a reversible down-regulation of the GnRH receptors in the pituitary gland and desensitization of the pituitary gonadotropes. These inhibitory effects result in decreased levels of LH and FSH.
Structure
There is limited information regarding Histrelin Structure in the drug label.
Pharmacodynamics
- Long-term treatment with histrelin acetate suppresses the LH response to GnRH causing LH levels to decrease to prepubertal levels within 1 month of treatment. As a result, serum concentrations of sex steroids (estrogen or testosterone) also decrease. Consequently, secondary sexual development ceases to progress in most patients. Additionally, linear growth velocity is slowed which improves the chance of attaining predicted adult height.
Pharmacokinetics
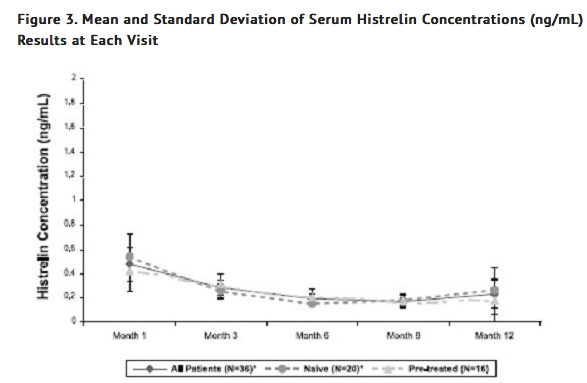
- Pharmacokinetics of histrelin after implantation of Histrelin was evaluated in a total of 47 children with CPP (11 subjects in Study 1 and 36 subjects in Study 2). Patients were examined at 4 weeks after implant insertion and a few times throughout the treatment period. Median serum histrelin concentrations remained above the limit of quantification for the treatment period. Histrelin acetate levels were sustained throughout the study period for most subjects (Figure 3). The median of maximum serum histrelin concentrations over the study period was 0.43 ng/mL, which is expected to maintain gonadotropins at prepubertal levels. There was no apparent pharmacokinetic difference between naïve subjects to a LHRH agonist treatment and subjects who had previous treatment with a LHRH agonist (Figure 3).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies were conducted in rats for 2 years at doses of 5, 25 or150 mcg/kg/day (up to 11 times human exposures using body surface area comparisons, based on a 65 mcg/day dose in humans) and in mice for 18 months at doses of 20, 200, or 2000 mcg/kg/day (at less than therapeutic exposure to 70 times human exposure using body surface area comparisons, based on a 65 mcg/day dose in humans). As seen with other GnRH agonists, histrelin injection administration was associated with an increase in tumors of hormonally responsive tissues. There was a significant increase in pituitary adenomas in rats at mid and high doses (2-11 times human exposure based on body surface area comparisons with a 65 mcg/day human dose). There was an increase in pancreatic islet-cell adenomas in treated female rats and a non-dose-related increase in testicular Leydig-cell tumors (highest incidence in the low-dose group). In mice, there was significant increase in mammary-gland adenocarcinomas in all treated females. In addition, there were increases in stomach papillomas in male rats given high doses, and an increase in histiocytic sarcomas in female mice at the highest dose.
- Mutagenicity studies have not been performed with histrelin acetate. Saline extracts of implants with and without histrelin acetate were negative in a battery of genotoxicity studies. Fertility studies have been conducted in rats and monkeys given subcutaneous daily doses of histrelin acetate up to 180 mcg/kg/day (up to 13 and 30 times human exposure, respectively using body surface area comparisons, based on a 65 mcg/day human dose) for 6 months and full reversibility of fertility suppression was demonstrated. The development and reproductive performance of offspring from parents treated with histrelin acetate has not been investigated.
Clinical Studies
- The efficacy of Histrelin in children with CPP has been evaluated in two single-arm, open label studies. Study 1 was conducted in 11 pretreated female patients, 3.7 to 11.0 years of age. Study 2 was conducted in 36 patients (33 females and 3 males), 4.5 to 11.6 years of age. Sixteen pretreated and 20 treatment-naïve patients were enrolled in Study 2. Baseline patient characteristics were typical of patients with CPP. Efficacy assessments were similar in both studies and included endpoints that measured the suppression of gonadotropins (luteinizing hormone and follicle stimulating hormone) and gonadal sex steroids (estrogen in girls and testosterone in boys, respectively) on treatment. Other assessments were clinical (evidence of stabilization or regression of signs of puberty) or gonadal steroid-dependent (bone age, linear growth). In Study 2, the primary measure of efficacy was LH suppression.
- In Study 2, suppression of LH was induced in all treatment naïve subjects and maintained in all pretreated subjects at Month 1 after implantation and continued through Month 12 (suppression was defined as a peak LH < 4 mIU/mL following stimulation with the GnRH analog leuprolide acetate).
- Secondary efficacy hormone assessments (FSH, estradiol and testosterone) and additional efficacy assessments (bone age advancement, linear growth, clinical progression of puberty) indicated stabilization of disease. Estradiol suppression was present in all 33 girls (100%) through Month 9 and 97% at Month 12. Testosterone suppression was maintained in the three pre-treated males participating in Study 2. The Histrelin effect on efficacy endpoints in the Study 1 was consistent with that observed in Study 2.
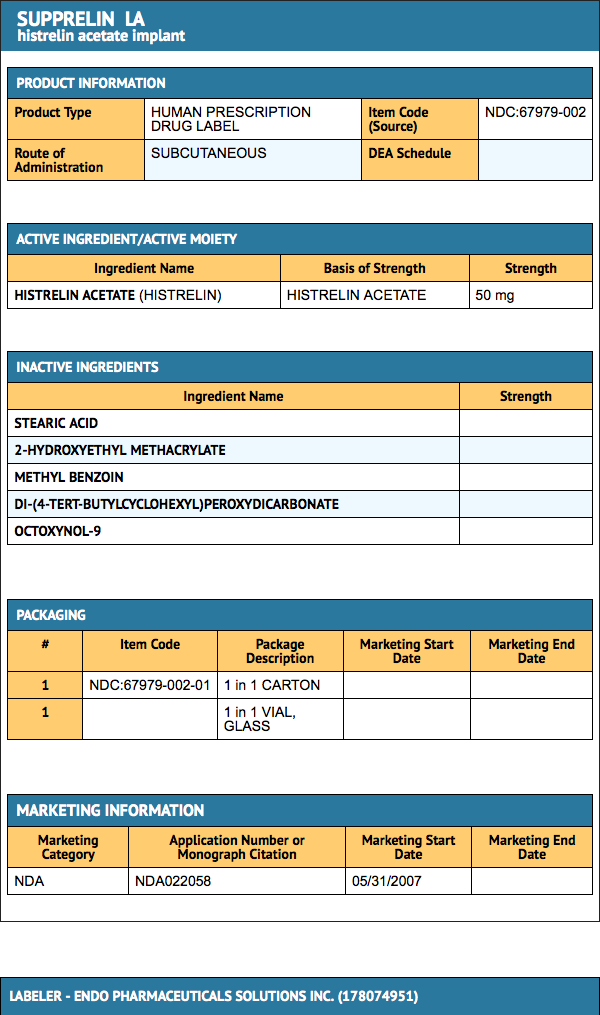
How Supplied
- UPPRELIN LA (NDC 67979-002-01) is supplied in a corrugated shipping carton that contains 2 inner cartons: a small one for the vial containing the Histrelin implant, which is shipped with a cold pack inside a polystyrene cooler that must be refrigerated upon arrival, and a larger one comprising the Implantation Kit, which must not be refrigerated, for use during insertion or removal of Histrelin.
- The Histrelin implant contains 50 mg of histrelin acetate. The Histrelin implant carton contains a cold pack for refrigerated shipment and a small carton containing an amber plastic pouch. Inside the pouch is a glass vial with a Teflon-coated stopper and an aluminum seal, containing the implant in 2 mL of sterile 1.8% sodium chloride solution. (Note: the 3.5 mL vial is not completely filled with saline).
Storage
Histrelin is stable when stored refrigerated, in its sealed vial, pouch, and carton, at 2-8 °C (36-46 °F) until the expiration date provided. Excursion permitted to 25 °C (77 °F) for 7 days. Do not freeze. Protect from light.
Images
Drug Images
{{#ask: Page Name::Histrelin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

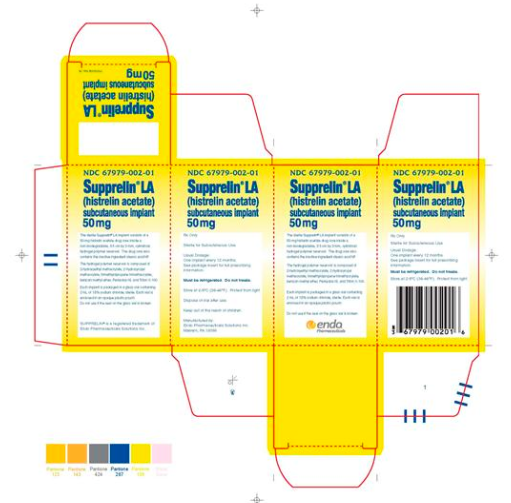
{{#ask: Label Page::Histrelin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Histrelin Patient Counseling Information in the drug label.
Precautions with Alcohol
- Alcohol-Histrelin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Histrelin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
References
Template:Sex hormones Template:Pituitary and hypothalamic hormones and analogues