Sandbox cah 17
| Sandbox cah 17 | |
| OMIM | 202110 |
|---|---|
| DiseasesDB | 1841 |
| MeSH | D000312 |
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Congenital adrenal hyperplasia due to 17α-hydroxylase deficiency is an uncommon form of congenital adrenal hyperplasia resulting from a defect in the gene for the enzyme CYP17A1, which mediates several key transformations in the synthesis of both cortisol and sex steroids. Because CYP17A1 mediates several reactions and different defective alleles can result in different combinations of impaired activity, people affected by this type of CAH can display a wide variety of problems and effects. Some versions of this disease cause ambiguous genitalia in genetic males, failure of the ovaries to function at puberty in genetic females, and/or hypertension due to excessive mineralocorticoid production.
Pathophysiology
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive diseases resulting from defects in steps of the synthesis of cortisol from cholesterol by the adrenal glands. All of the forms of CAH involve excessive or defective production of sex steroids and can pervert or impair development of primary or secondary sex characteristics in affected infants, children, and adults. Many also involve excessive or defective production of mineralocorticoids, which can cause hypertension or salt wasting, respectively.
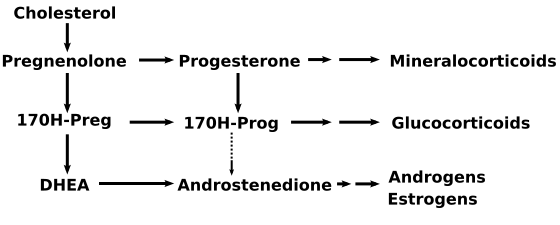
The enzyme itself is attached to the smooth endoplasmic reticulum of the steroid-producing cells of the adrenal cortex and gonads. CYP17A1 functions as both a 17α-hydroxylase and a 17,20-lyase. The dual activities mediate three key transformations in cortisol and sex steroid synthesis:
- As 17α-hydroxylase it mediates pregnenolone → 17-hydroxypregnenolone
- and progesterone → 17-hydroxyprogesterone.
- As 17,20-lyase it mediates 17-hydroxypregnenolone → DHEA.
- An expected second 17,20-lyase reaction (17-hydroxyprogesterone → androstenedione) is mediated so inefficiently in humans as to be of no known significance.
The hydroxylase reactions are part of the synthetic pathway to cortisol as well as sex steroids, but the lyase reaction is only necessary for sex steroid synthesis. Different alleles of the CYP17A1 gene result in enzyme molecules with a range of impaired or reduced function that produces a range of clinical problems.
The dual enzyme activities were for many decades assumed to represent two entirely different genes and enzymes. Thus, medical textbooks and nosologies until quite recently described two different diseases: 17α-hydroxylase deficient CAH, and a distinct and even rarer defect of sex steroid synthesis termed 17,20-lyase deficiency (which is not a form of CAH). In the last decade it has become clearer that the two diseases are different forms of defects of the same gene. However, the clinical features of the two types of impairment are distinct enough that they are described separately in the following sections.
Genetics
17α-hydroxylase deficient CAH
The gene for the cytochrome CYP17A1 enzyme resides on chromosome 10q24.3. Mutations of this gene result in altered activities of the enzyme and the various forms of congenital adrenal hyperplasia and sex steroid deficiency due to its impairment. As are most enzyme deficiencies, these disorders are inherited in an autosomal recessive manner with a reported incidence of about 1 in 50,000 births. The OMIM number for diseases arising from mutations of this gene is 202110.
17,20-lyase deficiency
A very small number of people have reportedly had an abnormal allele that resulted primarily in a reduction of 17,20-lyase activity, rather than both the hydroxylase and lyase activities as described above. In these people the defect had the effect of an isolated impairment of sex steroid synthesis, with no significant effects on mineralocorticoid or glucocorticoid production, and no adrenal hyperplasia, mineralocorticoid overproduction, or hypertension.
The sex steroid deficiency produces effects similar to 17α-hydroxylase deficiency. Severely affected genetic females (XX) are born with normal internal and external genitalia and there are no clues to abnormality until adolescence, when both the androgenic and estrogenic signs (e.g., breasts and pubic hair) of puberty fail to occur. Gonadotropins are high and the uterus infantile in size. The ovaries may contain enlarged follicular cysts, and ovulation may not occur even after replacement of estrogen.
Natural History, Complications, and Prognosis
Complications
Glucocorticoid Effects of 17α-hydroxylase deficient CAH
Although production of cortisol is inefficient enough to raise ACTH, the 50-100-fold elevations of corticosterone have enough weak glucocorticoid activity to prevent glucocorticoid deficiency and adrenal crisis.
Effects of Impaired Sex Steroid Synthesis
Genetic XX females affected by 17α-hydroxylase deficiency are born with normal female internal and external anatomy. At the expected time of puberty, neither the adrenals nor the ovaries can produce sex steroids, so neither breast development nor pubic hair appear. Investigation of delayed puberty yields elevated gonadotropins and normal karyotype, while imaging confirms the presence of ovaries and an infantile uterus. Discovery of hypertension and hypokalemic alkalosis usually suggests the presence of one of the proximal forms of CAH, and the characteristic mineralocorticoid elevations confirm the specific diagnosis.
A few milder forms of this deficiency in genetic females have allowed relatively normal breast development and irregular menstruation. Evidence suggests that only 5% of normal enzyme activity may be enough to allow at least the physical changes of female puberty, if not ovulation and fertility. In these girls, the elevated blood pressure was the primary clinical problem.
17α-Hydroxylase deficiency in genetic males (XY) results in moderate to severe reduction of fetal testosterone production by both adrenals and testes. Undervirilization is variable and sometimes complete. The appearance of the external genitalia ranges from normal female to ambiguous to mildly underdeveloped male. The most commonly described phenotype is a small phallus, perineal hypospadias, small blind pseudovaginal pouch, and intra-abdominal or inguinal testes. Wolffian duct derivatives are hypoplastic or normal, depending on degree of testosterone deficiency. Some of those with partial virilization develop gynecomastia at puberty even though masculinization is reduced. The presence of hypertension in the majority distinguishes them from other forms of partial androgen deficiency or insensitivity. Fertility is impaired in those with more than minimal testoserone deficiency.
Mineralocorticoid Effects
The adrenal cortex is hyperplastic and overstimulated, with no impairment of the mineralocorticoid pathway. Consequently, levels of DOC, corticosterone, and 18-deoxycorticosterone are elevated. Although these precursors of aldosterone are weaker mineralocorticoids, the extreme elevations usually provide enough volume expansion, blood pressure elevation, and potassium depletion to suppress renin and aldosterone production. Some persons with 17α-hydroxylase deficiency develop hypertension in infancy, and nearly 90% do so by late childhood. The low-renin hypertension is often accompanied by hypokalemia due to urinary potassium wasting and metabolic alkalosis. These features of mineralocorticoid excess are the major clinical clue distinguishig the more complete 17α-hydroxylase deficiency from the 17,20-lyase deficiency, which only affects the sex steroids. Treatment with glucocorticoid suppresses ACTH, returns mineralocorticoid production toward normal, and lowers blood pressure.
Treatment
The most difficult management decisions are posed by the more ambiguous genetic (XY) males. Most who are severely undervirilized, looking more female than male, are raised as females with surgical removal of the nonfunctional testes. If raised as males, a brief course of testosterone can be given in infancy to induce growth of the penis. Surgery may be able to repair the hypospadias. The testes should be salvaged by orchiopexy if possible. Testosterone must be replaced in order for puberty to occur and continued throughout adult life.
Pharmacotherapy
Management of 17α-hydroxylase and 17,20-lyase deficiencies
Hypertension and mineralocorticoid excess is treated with glucocorticoid replacement, as in other forms of CAH.
Most genetic females with both forms of the deficiency will need replacement estrogen to induce puberty. Most will also need periodic progestin to regularize menses. Fertility is usually reduced because egg maturation and ovulation is poorly supported by the reduced intra-ovarian steroid production.
Related Chapters
- Congenital adrenal hyperplasia for an overview of CAH, more detailed discussion of management issues related to all forms of CAH, and links to support groups.
- Lipoid congenital adrenal hyperplasia
- Congenital adrenal hyperplasia due to 3β-hydroxysteroid dehydrogenase deficiency
- Congenital adrenal hyperplasia due to 11β-hydroxylase deficiency
- Intersex and ambiguous genitalia
- Adrenal insufficiency