Pramlintide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: SEVERE HYPOGLYCEMIA
See full prescribing information for complete Boxed Warning.
* SYMLIN use with insulin increases the risk of severe hypoglycemia, particularly in patients with type 1 diabetes. When severe hypoglycemia occurs, it is seen within 3 hours following a SYMLIN injection. Serious injuries may occur if severe hypoglycemia occurs while operating a motor vehicle, heavy machinery, or while engaging in other high-risk activities. Appropriate patient selection, careful patient instruction, and insulin dose reduction are critical elements for reducing this risk.
|
Overview
Pramlintide is an antidiabetic that is FDA approved for the treatment of patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose] control despite optimal insulin therapy. There is a Black Box Warning for this drug as shown here. Common adverse reactions include abdominal pain, anorexia, nausea, vomiting, hypersensitivity reaction, dizziness, headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- SYMLIN is indicated as an adjunctive treatment in patients with type 1 or type 2 diabetes who use mealtime insulin therapy and who have failed to achieve desired glucose control despite optimal insulin therapy.
- Pramlintide acetate is supplied as a sterile injection in the following dosage forms:
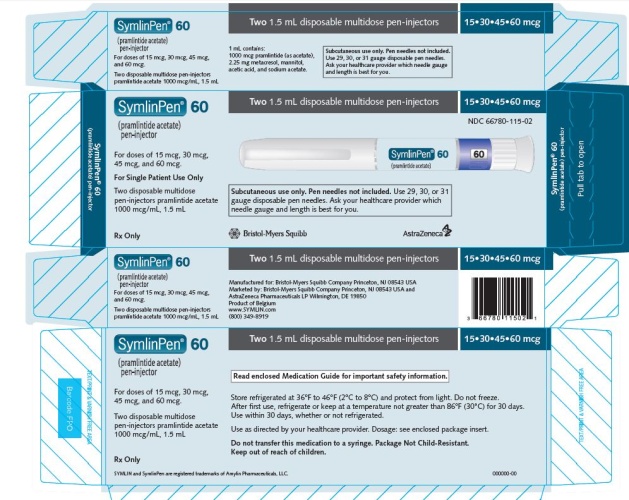
- 1.5 mL disposable multidose pramlintide acetatePen ® 60 pen-injector containing 1000 mcg/mL pramlintide (as acetate).
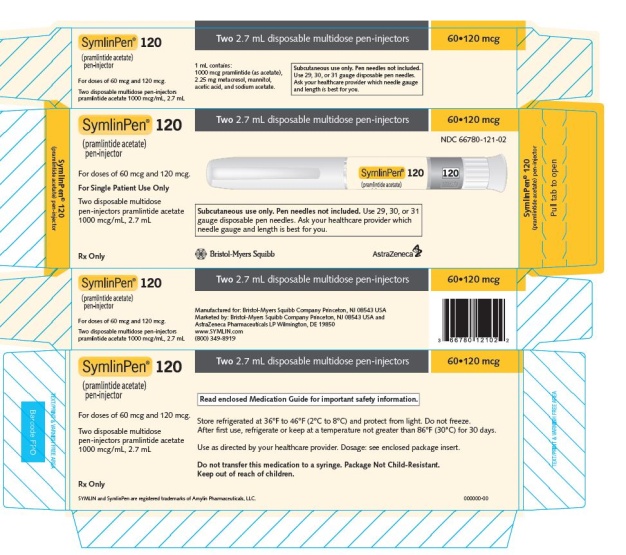
- 2.7 mL disposable multidose pramlintide acetatePen ® 120 pen-injector containing 1000 mcg/mL pramlintide (as acetate).
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pramlintide in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pramlintide in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Pramlintide in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pramlintide in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pramlintide in pediatric patients.
Contraindications
- pramlintide acetate is contraindicated in patients with any of the following: serious hypersensitivity reaction to pramlintide acetate or to any of its product components.
- Hypoglycemia unawareness.
- Confirmed gastroparesis.
Warnings
|
WARNING: SEVERE HYPOGLYCEMIA
See full prescribing information for complete Boxed Warning.
* SYMLIN use with insulin increases the risk of severe hypoglycemia, particularly in patients with type 1 diabetes. When severe hypoglycemia occurs, it is seen within 3 hours following a SYMLIN injection. Serious injuries may occur if severe hypoglycemia occurs while operating a motor vehicle, heavy machinery, or while engaging in other high-risk activities. Appropriate patient selection, careful patient instruction, and insulin dose reduction are critical elements for reducing this risk.
|
- Patients may experience erythema, edema, or pruritus at the site of injection. These minor reactions usually resolve in a few days to a few weeks. In some instances, these reactions may be related to factors other than pramlintide acetate, such as irritants in a skin cleansing agent or improper injection technique.
Patient Selection
- Proper patient selection is critical to the safe and effective use of pramlintide acetate. Before initiating pramlintide acetate, the patient's HbA1c, recent blood glucose monitoring data, history of insulin-induced hypoglycemia, current insulin regimen, and body weight should be reviewed. Pramlintide acetate therapy should only be considered in patients with type 1 diabetes or patients with type 2 diabetes using mealtime insulin who fulfill the following criteria:
- Have failed to achieve adequate glycemic control despite individualized insulin management.
- Are receiving ongoing care under the guidance of a healthcare professional skilled in the use of insulin and supported by the services of diabetes educator(s).
- Patients meeting any of the following criteria should NOT be considered for SYMLIN therapy:
- Poor compliance with current insulin regimen.
- Poor compliance with prescribed self blood glucose monitoring.
- Have a HbA1c >9%.
- Recurrent severe hypoglycemia requiring assistance during the past 6 months.
- Presence of hypoglycemia unawareness.
- Confirmed diagnosis of gastroparesis.
- Require the use of drugs that stimulate gastrointestinal motility.
- Pediatric patients.
- SYMLIN should be prescribed with caution to persons with visual or dexterity impairment.
Hypoglycemia
- Pramlintide acetate alone does not cause hypoglycemia. However, pramlintide acetate is indicated to be coadministered with mealtime insulin therapy, and in this setting there is an increased risk of severe hypoglycemia, particularly in patients with type 1 diabetes. If severe hypoglycemia associated with pramlintide acetate occurs, it is usually seen within the first 2 to 3 hours following a pramlintide acetate injection. If severe hypoglycemia occurs while operating a motor vehicle, heavy machinery, or while engaging in other high-risk activities, serious injuries or death may occur. Therefore, when introducing pramlintide acetate therapy, appropriate precautions need to be taken to avoid increasing the risk for severe hypoglycemia.
- These precautions include frequent monitoring of pre- and post-meal glucose combined with an initial 50% reduction in doses of mealtime insulin.
- Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as longstanding diabetes; diabetic neuropathy; use of medications such as beta-blockers, clonidine, guanethidine, or reserpine; or intensified glycemic control.
- The addition of any anti-diabetic medication, such as pramlintide acetate, to an existing regimen of one or more anti-diabetic medications (e.g., sulfonylurea), or other medications that can increase the risk of hypoglycemia may necessitate further insulin dose adjustments and particularly close monitoring of blood glucose.
- pramlintide acetatePen should never be shared between patients, even if the needle is changed. Pen-sharing poses a risk for transmission of blood-borne pathogens.
Never Mix pramlintide acetate and Insulin
- Mixing pramlintide acetate and insulin can alter the pharmacokinetics of both products which may result in inadequate glucose control or hypoglycemia. Therefore, pramlintide acetate and insulin must always be administered as separate injections and should never be mixed.
Concomitantly Administered Oral Medications
- Pramlintide acetate slows gastric emptying, which may delay the absorption of concomitantly administered oral medications. Administer the concomitant oral medication at least 1 hour prior to pramlintide acetate injection or 2 hours after pramlintide acetate injection if the rapid onset or threshold concentration of the concomitant medication is a critical determinant of its effectiveness (such as with analgesics, antibiotics, and oral contraceptives).
Medications that Affect Gastrointestinal Motility
- Pramlintide acetate slows gastric emptying. Pramlintide acetate is not recommended for patients taking other medications that alter gastrointestinal motility.
Allergy
- Local allergy.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trial Experience
Adverse Reactions (Excluding Hypoglycemia)
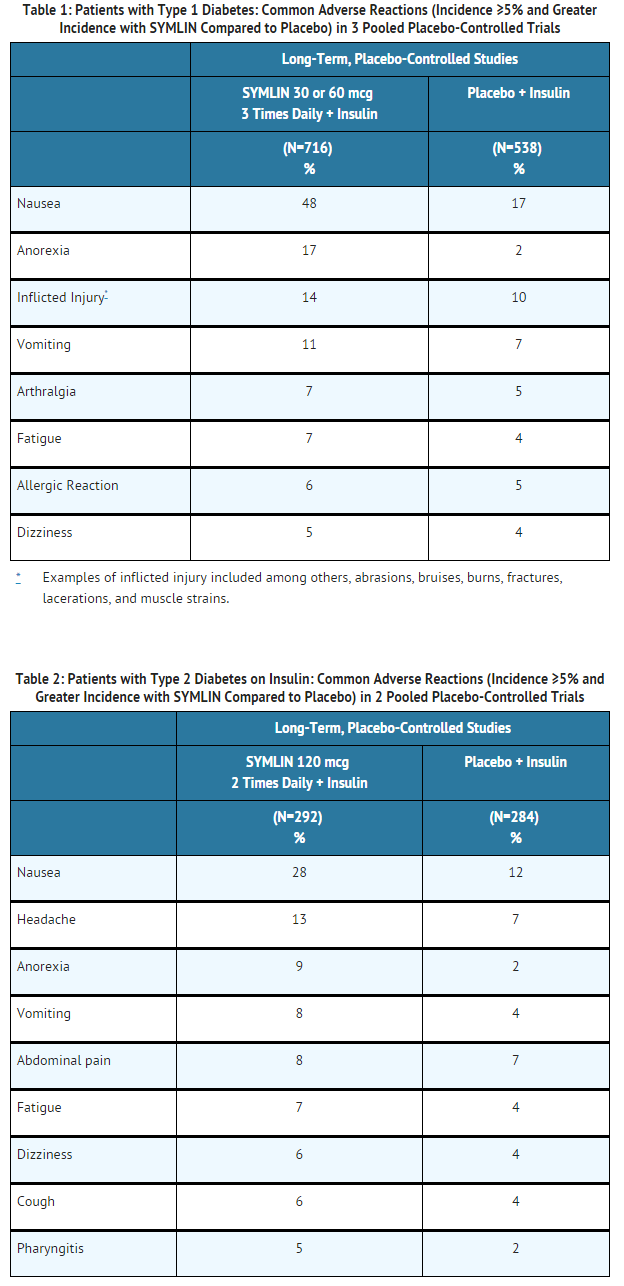
- Adverse reactions (excluding hypoglycemia, which is discussed separately below) commonly associated with pramlintide acetate when coadministered with a fixed dose of insulin in the 26- to 52-week, placebo-controlled trials in patients with type 1 diabetes and patients with type 2 diabetes on mealtime insulin are presented in Table 1 and Table 2, respectively.
- Most adverse reactions were gastrointestinal in nature. The incidence of nausea is higher at the beginning of pramlintide acetate treatment and decreases with time in most patients. Gradual titration of the pramlintide acetate dose minimizes the incidence and severity of nausea.
Severe Hypoglycemia
- Coadministration of pramlintide acetate with mealtime insulin increases the risk of severe hypoglycemia, particularly in patients with type 1 diabetes.
- Two definitions of severe hypoglycemia were used in the pramlintide acetate clinical trials. Patient-ascertained severe hypoglycemia was defined as an episode of hypoglycemia requiring the assistance of another individual (including help administering oral carbohydrate) or requiring the administration of glucagon, intravenous glucose, or other medical intervention.
- Medically-assisted severe hypoglycemia was defined as an episode of hypoglycemia that was classified as a serious event by the investigator or that required glucagon, intravenous glucose, hospitalization, paramedic assistance or an emergency room visit. The incidence of severe hypoglycemia during the pramlintide acetate clinical development program is summarized in Table 3 and Table 4.
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of pramlintide acetate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Injection site reactions
- Pancreatitis
Drug Interactions
Insulin
- The pharmacokinetic parameters of pramlintide are altered when pramlintide acetate is mixed in the same syringe with regular, NPH, and 70/30 premixed formulations of recombinant human insulin. pramlintide acetate and insulin must not be mixed and must be administered as separate injections.
Oral Medications
- Pramlintide acetate has the potential to delay the absorption of concomitantly administered oral medications. When the rapid onset or threshold concentration of a concomitant orally administered medication is a critical determinant of effectiveness (such as with analgesics, antibiotics, and oral contraceptives), the medication should be administered at least 1 hour prior to pramlintide acetate injection or 2 hours after pramlintide acetate injection.
Drugs Affecting Gastrointestinal Motility
- Due to its effects on gastric emptying, pramlintide acetate should not be considered for patients taking medications that alter gastrointestinal motility (e.g., anticholinergic agents such as atropine) or medications that slow the intestinal absorption of nutrients (e.g., alpha-glucosidase inhibitors). Patients using these medications have not been studied in pramlintide acetate clinical trials.
Drugs Affecting Glucose Metabolism
- The following are examples of medications that may increase the susceptibility to hypoglycemia when administered with pramlintide acetate: oral anti-diabetic products, angiotensin converting enzyme (ACE) inhibitors, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, propoxyphene, salicylates, somatostatin analogs, and sulfonamide antibiotics. Pramlintide acetate and these drugs should be coadministered with caution.
Use in Specific Populations
Pregnancy
- No adequate and well-controlled studies have been conducted in pregnant women. Studies in perfused human placenta indicate that pramlintide acetate has low potential to cross the maternal/fetal placental barrier. Embryofetal toxicity studies with pramlintide acetate have been performed in rats and rabbits.
- Increases in congenital abnormalities (neural tube defect, cleft palate, exencephaly) were observed in fetuses of rats treated during organogenesis with 0.3 and 1.0 mg/kg/day (10 and 47 times the exposure resulting from the human dose of 360 mcg/day based on area under the plasma concentration curve [AUC], respectively). Administration of doses up to 0.3 mg/kg/day pramlintide acetate (9 times the human dose of 360 mcg/day based on AUC) to pregnant rabbits had no adverse effects in embryo fetal development; however, animal reproduction studies are not always predictive of human response. pramlintide acetate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pramlintide in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Pramlintide during labor and delivery.
Nursing Mothers
- It is unknown whether pramlintide acetate is excreted in human milk. Many drugs, including peptides, are excreted in human milk. Therefore, pramlintide acetate should be administered to nursing women only if it is determined by the healthcare professional that the potential benefit outweighs the potential risk to the infant.
Pediatric Use
- Safety and effectiveness of SYMLIN in pediatric patients have not been established.
Geriatic Use
- Pramlintide acetate has been studied in patients ranging in age from 15 to 84 years of age, including 769 patients ≥65 to 75 years of age and 87 patients ≥75 years of age. No consistent differences in the efficacy and safety of pramlintide acetate have been observed in older patients, but greater sensitivity in some older individuals cannot be ruled out.
- As is recommended for all patients, pramlintide acetate and insulin regimens should be carefully managed to minimize the risk of severe hypoglycemia.
Gender
- No consistent differences in the efficacy and safety of pramlintide acetate have been observed between men and women in pramlintide acetate clinical trials (n=2799 for male and n=2085 for female).
Race
- No consistent differences in the efficacy and safety of pramlintide acetate have been observed among patients of differing race/ethnicity in pramlintide acetate clinical trials (n=4257 for Caucasian, n=229 for black, n=337 for Hispanic or Latino, and n=61 for Asian and one or more races) although the smaller sample sizes for non-Caucasians, particularly Asians, limit conclusions.
Renal Impairment
- The dosing requirements for pramlintide acetate are not altered in patients with mild (creatinine clearance [ClCr] 60-89 mL/min), moderate (ClCr 30-59 mL/min) or severe renal impairment (ClCr 15-29 mL/min). pramlintide acetate has not been studied in patients with end-stage renal disease
Hepatic Impairment
- pramlintide acetate use has not been studied in patients with hepatic impairment
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Pramlintide in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Pramlintide in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
- Monitor glucoses frequently and individualize subsequent insulin dose adjustments.
- Monitor blood glucoses frequently, including pre- and post-meals and at bedtime, particularly when initiating pramlintide acetate or increasing the pramlintide acetate dose.
IV Compatibility
There is limited information regarding IV Compatibility of Pramlintide in the drug label.
Overdosage
- Single 10 mg doses of pramlintide acetate (83 times the maximum recommended dose of 120 mcg for patients with type 2 diabetes) were administered to 3 healthy volunteers.
- All 3 individuals reported severe nausea associated with vomiting, diarrhea, vasodilatation, and dizziness. No hypoglycemia was reported. Pramlintide has a short half-life (approximately 48 minutes in healthy individuals). Initiate supportive measures in the case of overdose.
Pharmacology
There is limited information regarding Pramlintide Pharmacology in the drug label.
Mechanism of Action
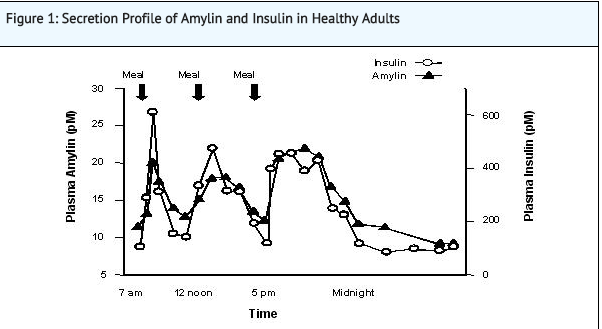
- Pramlintide is an analog of human amylin. Amylin is colocated with insulin in secretory granules and cosecreted with insulin by pancreatic beta cells in response to food intake. Amylin and insulin show similar fasting and postprandial patterns in healthy individuals (Figure 1).
- In patients with type 1 and type 2 diabetes, there is reduced secretion from pancreatic beta cells of both insulin and amylin in response to food.
- Amylin affects the rate of postprandial glucose appearance through a variety of mechanisms, as determined by nonclinical studies. Amylin slows gastric emptying (i.e., the rate at which food is released from the stomach to the small intestine) without altering the overall absorption of nutrients. * In addition, amylin suppresses glucagon secretion (not normalized by insulin alone), which leads to suppression of endogenous glucose output from the liver. Amylin also regulates food intake due to centrally-mediated modulation of appetite.
- In human studies, pramlintide, acting as an amylin analog, slows gastric emptying, reduces the postprandial rise in plasma glucagon, and modulates satiety leading to decreased caloric intake.
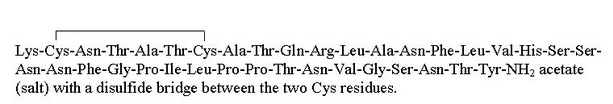
Structure
- Pramlintide acetate injection is an anti-diabetic medication for use in patients with diabetes treated with insulin. Pramlintide is a synthetic analog of human amylin, a naturally occurring neuroendocrine hormone synthesized by pancreatic beta cells that contributes to glucose control during the postprandial period. Pramlintide is provided as an acetate salt of the synthetic 37-amino acid polypeptide, which differs in amino acid sequence from human amylin by replacement with proline at positions 25 (alanine), 28 (serine), and 29 (serine).
Pramlintide acetate is a white powder that has a molecular formula of C171H267N51O53S2• × C2H4O2 (3≤ × ≤8); the molecular weight is 3949.4. Pramlintide acetate is soluble in water.
- Pramlintide acetate is formulated as a clear, isotonic, sterile solution for subcutaneous administration. The disposable multidose pramlintide acetatePen® pen-injector contains 1000 mcg/mL of pramlintide (as acetate). The formulation contains 2.25 mg/mL of metacresol as a preservative, D-mannitol as a tonicity modifier, acetic acid, sodium acetate as pH modifiers, and water for injection. Pramlintide acetate has a pH of approximately 4.0.
Pharmacodynamics
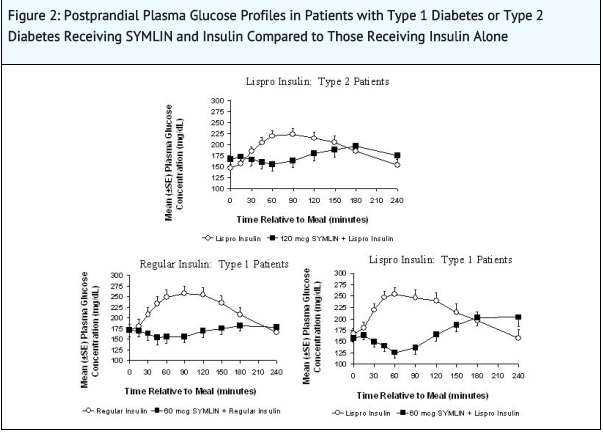
- In clinical studies in patients with type 1 diabetes and patients with type 2 diabetes using mealtime insulin, pramlintide acetate reduced mean postprandial glucose concentrations, reduced glucose fluctuations, and reduced food intake.
Reduction in Postprandial Glucose Concentrations
- In a randomized, single-blind, placebo-controlled, crossover study, 19 subjects with type 2 diabetes using insulin lispro, 19 subjects with type 1 diabetes using regular human insulin, and 21 subjects with type 1 diabetes using insulin lispro underwent mixed-meal tests. Pramlintide acetate administered subcutaneously immediately prior to a meal reduced plasma glucose concentrations following the meal when used with mealtime insulin (rapid-acting insulin analogs or regular human insulin) (Figure 2). When rapid-acting insulin analogs were used, plasma glucose concentrations tended to rise during the interval between 150 minutes following pramlintide acetate injection and the next meal
- While pramlintide acetate reduces postprandial glucose, clinical studies employing a controlled hypoglycemic challenge have demonstrated that pramlintide acetate does not alter the counter-regulatory hormonal response to insulin-induced hypoglycemia. Likewise, in pramlintide acetate-treated patients, the perception of hypoglycemic symptoms was not altered with plasma glucose concentrations as low as 45 mg/dL. In a separate clinical trial pramlintide also reduced the 24-hour glucose fluctuations based upon 24-hour glucose monitoring.
Reduced Food Intake
- A single, subcutaneous dose of 30 mcg of pramlintide acetate to patients with type 1 diabetes and 120 mcg of pramlintide acetate to patients with type 2 diabetes administered 1 hour prior to an unlimited buffet meal was associated with reductions in total caloric intake (placebo-subtracted mean changes of ~21% and 23%, respectively), which occurred without decreases in meal duration.
Pharmacokinetics
Absorption
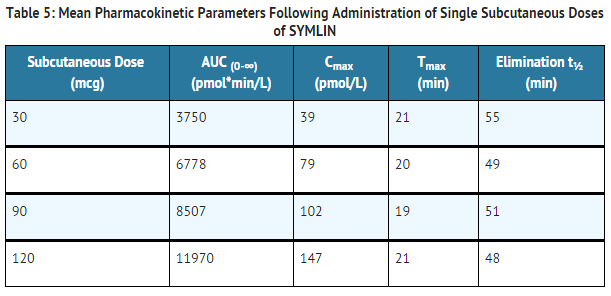
- The absolute bioavailability of pramlintide following a single subcutaneous dose of pramlintide acetate is approximately 30% to 40%. Subcutaneous administration of different doses of pramlintide acetate into the abdominal area or thigh of healthy individuals showed a linear, dose-dependent increase in maximum plasma concentrations (Cmax) and overall exposure (AUC) (Table 5).
- Table 5: Mean Pharmacokinetic Parameters Following Administration of Single Subcutaneous Doses of pramlintide acetate
- Injection of pramlintide acetate into the arm in obese patients with type 1 or type 2 diabetes showed higher overall exposure (20%-36%) with greater variability (% CV for AUC: 73%-106%), compared with exposure after injection of pramlintide acetate into the abdominal area or thigh.
- Relative bioavailability of pramlintide was not significantly different between obese and non-obese patients and based on BMI or skin fold thickness. Injections administered with 6.0-mm and 12.7-mm needles yielded similar bioavailability.
Distribution
- Pramlintide acetate does not extensively bind to red blood cells or albumin (approximately 40% of the drug is unbound in plasma).
Metabolism and Elimination
- In healthy individuals, the half-life of pramlintide is approximately 48 minutes. The primary metabolite, Des-lys1 pramlintide (2-37 pramlintide), is biologically active in vitro. Overall exposure (AUC) to pramlintide is relatively constant with repeat dosing of pramlintide acetate, indicating no bioaccumulation.
Specific Populations
Renal Impairment
- No studies have been conducted in patients with end-stage renal disease. In a single-dose pharmacokinetic study in patients with type 1 diabetes, 60 mcg of pramlintide acetate was administered to 4 patients with normal renal function (ClCr >90 mL/min), 9 patients with mild renal impairment (ClCr 60-89 mL/min), 5 patients with moderate renal impairment (ClCr 30-59 mL/min) and 3 patients with severe renal impairment (ClCr 15-29 mL/min). No statistically significant differences were noted in total (AUC0-∞) and peak (Cmax) exposure of pramlintide for mild, moderate, and severe renal impairment categories in comparison to patients with normal renal function; although, inter-patient variability in pharmacokinetic parameters was high.
Hepatic Impairment
- Pharmacokinetic studies have not been conducted in patients with hepatic impairment.
Geriatric
- Pharmacokinetic studies have not been conducted in the geriatric population.
Pediatric
- The efficacy and safety of pramlintide acetate have not been established in the pediatric population. The use of SYMLIN is not recommended in pediatric patients due to the risk of severe hypoglycemia.
Gender
- No study has been conducted to evaluate the effect of gender on pramlintide pharmacokinetics.
Race/Ethnicity
- No study has been conducted to evaluate the effect of ethnicity on pramlintide pharmacokinetics.
Drug Interactions
=Effect of Pre-Mixing Pramlintide Acetate with Insulin=
- Pharmacokinetic profiles of pramlintide and insulins after coadministration of 30 mcg pramlintide acetate with different insulins (regular, NPH, and 70/30 premixed formulations of recombinant human insulin) as one subcutaneous injection, premixed in one syringe, were compared to those observed after the coadministration of pramlintide acetate and different insulins given as separate subcutaneous injections. The effects of premixing on pramlintide pharmacokinetics varied across the different insulin products with a maximum decrease of 40% in pramlintide Cmax and a maximum increase of 36% in pramlintide AUC0-∞. Similarly, effects of premixing on insulin pharmacokinetics varied across different insulin products with a maximum increase of 15% in insulin Cmax and up to a 20% increase in insulin AUC0-600min. Always administer SYMLIN and insulin as separate injections and never mix.
Acetaminophen
- When 1000 mg acetaminophen was given within 0, 1, and 2 hours after a 120 mcg pramlintide acetate injection in patients with type 2 diabetes (n=24), acetaminophen Cmax decreased by 29%, 23%, and 20%, respectively compared to placebo. The time to maximum plasma concentration or Tmax increased by 72, 48, and 48 minutes, respectively. pramlintide acetate did not significantly affect acetaminophen Tmax or Cmax when acetaminophen was administered 1 to 2 hours before pramlintide acetate injection. pramlintide acetate did not affect acetaminophen AUC regardless of the time of acetaminophen administration in relation to pramlintide acetate injection.
Oral Contraceptives
- When a single dose of a combination oral contraceptive product, containing 30 mcg ethinyl estradiol and 300 mcg norgestrel, was administered 15 minutes after pramlintide acetate injection (90 mcg dose) in healthy female subjects, there was no statistically significant change in the Cmax and AUC of ethinyl estradiol. However, the norgestrel Cmax was reduced by about 30% and Tmax was delayed by 45 minutes; there was no effect on norgestrel AUC. The clinical relevance of this change is unknown.
Ampicillin
- The effect of concomitant administration of pramlintide acetate and ampicillin was evaluated in healthy volunteers. The administration of a single oral 500 mg dose of ampicillin 15 minutes after a single dose of pramlintide acetate (90 mcg) did not alter the Cmax or AUC for ampicillin. However, the Tmax for ampicillin was delayed by approximately 60 minutes.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- A two-year carcinogenicity study was conducted in CD-1 mice with doses of 0.2, 0.5, and 1.2 mg/kg/day of pramlintide acetate (32, 67, and 159 times the exposure resulting from the human dose of 360 mcg/day based on area under the plasma concentration curve or AUC, respectively). No drug-induced tumors were observed. A two-year carcinogenicity study was conducted in Sprague-Dawley rats with doses of 0.04, 0.2, and 0.5 mg/kg/day of pramlintide acetate (3, 9, and 25 times the exposure resulting from the human dose of 360 mcg/day based on AUC, respectively). No drug-induced tumors were observed in any organ.
Mutagenesis
- Pramlintide acetate was not mutagenic in the Ames test and did not increase chromosomal aberration in the human lymphocytes assay. Pramlintide acetate was not clastogenic in the in vivo mouse micronucleus test or in the chromosomal aberration assay utilizing Chinese hamster ovary cells.
Impairment of Fertility
- Administration of 0.3, 1, or 3 mg/kg/day of pramlintide acetate (8, 17, and 82 times the exposure resulting from the human dose of 360 mcg/day of mcg based on body surface area) had no significant effects on fertility in male or female rats. The highest dose of 3 mg/kg/day resulted in dystocia in 8/12 female rats secondary to significant decreases in serum calcium levels.
Clinical Studies
- A total of 2333 patients with type 1 diabetes and 1852 patients with type 2 diabetes received pramlintide acetate in controlled clinical trials.
Type 1 Diabetes
- The efficacy and safety of pramlintide acetate were evaluated in 3 (26-52-week), randomized, double-blind, placebo-controlled trials in patients with type 1 diabetes. In these studies, insulin adjustments were minimized in order to isolate the pramlintide acetate effect with insulin adjustments allowed, at the investigator's discretion, when excessive hypoglycemia was encountered. Patients participating in these 3 trials had a mean age of 40 years, a mean duration of diabetes of 17 years, and a mean body mass index of 25.9 kg/m2.
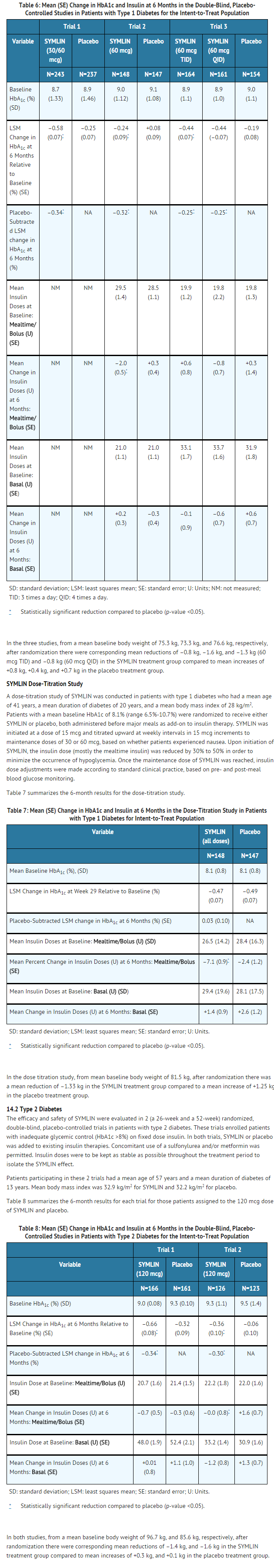
- Table 6 summarizes the 6-month results for those patients assigned to the 30 or 60 mcg dose of pramlintide acetate or placebo.
- In both studies, from a mean baseline body weight of 96.7 kg, and 85.6 kg, respectively, after randomization there were corresponding mean reductions of –1.4 kg, and –1.6 kg in the pramlintide acetate treatment group compared to mean increases of +0.3 kg, and +0.1 kg in the placebo treatment group.
How Supplied
- pramlintide acetate Injection is available in the following package sizes:
- Pramlintide acetatePen ® 60 pen-injector, containing 1000 mcg/mL pramlintide (as acetate)
- Two 1.5 mL disposable multidose pen-injectors (NDC 0310-6615-02)
- Pramlintide acetatePen ® 120 pen-injector, containing 1000 mcg/mL pramlintide (as acetate)
- Two 2.7 mL disposable multidose pen-injectors (NDC 0310-6627-02)
Storage
Storage and Handling
- Pramlintide acetate pen-injectors not in use: Refrigerate (2°C to 8°C; 36°F to 46°F), and protect from light. Do not freeze. Do not use if product has been frozen. Unused pramlintide acetate (opened or unopened) should not be used after the expiration (EXP) date printed on the carton and the label.
- Pramlintide acetate pen-injectors in use: After first use, refrigerate or keep at a temperature not greater than 86°F (30°C) for 30 days. Use within 30 days, whether or not refrigerated.
- Storage conditions are summarized in Table 9.
Images
Drug Images
{{#ask: Page Name::Pramlintide |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Pramlintide |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Risk of Hypoglycemia
- Discuss the risk and consequences of hypoglycemia and approaches to minimize its occurrence. Inform patients about the importance of self-management practices including glucose monitoring and timing of dosing. In addition, reinforce the importance of adherence to meal planning, physical activity, recognition and management of hypoglycemia and hyperglycemia, and assessment of diabetes complications.
- Advise patients that they should never share a SymlinPen with another person, even if the needle is changed, because doing so carries a risk for transmission of blood-borne pathogens.
Never Mix SYMLIN and Insulin
- Inform patients that SYMLpramlintide acetateIN and insulin should always be administered as separate injections and never be mixed.
- Show patients how to administer SYMLIN using the pen-injector. Advise patients to use a new needle for each injection.
Instructions
- Inform patients of the potential risks and advantages of SYMLIN therapy. Advise women with diabetes to inform their healthcare professional if they are pregnant or contemplating pregnancy. Instruct patients on the proper injection technique and proper storage of SYMLIN. Instruct patients on handling of special situations such as intercurrent conditions (illness or stress), an inadequate or omitted insulin dose, inadvertent administration of increased insulin or SYMLIN dose, inadequate food intake or missed meals. Refer patients to the SYMLIN Medication Guide and Patient Instructions for Use for additional information.
Precautions with Alcohol
- Alcohol-Pramlintide interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- SYMLINPEN ®[1]
Look-Alike Drug Names
There is limited information regarding Pramlintide Look-Alike Drug Names in the drug label.
Drug Shortage Status
{{#subobject:
|Label Page=Pramlintide |Label Name=Pram01.jpg
}}
{{#subobject:
|Label Page=Pramlintide |Label Name=Pram 02.jpg
}}
{{#subobject:
|Label Page=Pramlintide |Label Name=DailyMed - SYMLINPEN- pramlintide acetate injection .png
}}
Price
References
The contents of this FDA label are provided by the National Library of Medicine.