Olodaterol
{{DrugProjectFormSinglePage |authorTag=Vignesh Ponnusamy, M.B.B.S. [1] |aOrAn=a |drugClass=long-acting beta2-adrenergic agonist |indicationType=treatment |indication=airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema |hasBlackBoxWarning=Yes |adverseReactions=nasopharyngitis, upper respiratory tract infection, bronchitis, urinary tract infection, cough, dizziness, rash, diarrhea, back pain and arthralgia
|blackBoxWarningTitle=WARNING |blackBoxWarningBody=ASTHMA-RELATED DEATH:
- Long-acting beta2-adrenergic agonists (LABA) increase the risk of asthma-related death. Data from a large, placebo-controlled US study that compared the safety of another long-acting beta2-adrenergic agonist (salmeterol) or placebo added to usual asthma therapy showed an increase in asthma-related deaths in patients receiving salmeterol. This finding with salmeterol is considered a class effect of LABA, including olodaterol, the active ingredient in STRIVERDI RESPIMAT. The safety and efficacy of STRIVERDI RESPIMAT in patients with asthma have not been established. STRIVERDI RESPIMAT is not indicated for the treatment of asthma.
|fdaLIADAdult======Maintenance Treatment of COPD=====
- The recommended dose of STRIVERDI RESPIMAT is two inhalations once-daily at the same time of the day. Do not use STRIVERDI RESPIMAT more than two inhalations every 24 hours.
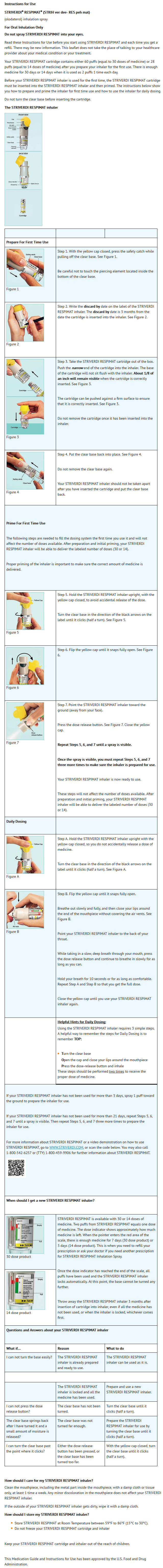
- Prior to first use, the STRIVERDI RESPIMAT cartridge is inserted into the STRIVERDI RESPIMAT inhaler and the unit is primed. When using the unit for the first time, patients are to actuate the inhaler toward the ground until an aerosol cloud is visible and then repeat the process three more times. The unit is then considered primed and ready for use. If not used for more than 3 days, patients are to actuate the inhaler once to prepare the inhaler for use. If not used for more than 21 days, patients are to actuate the inhaler until an aerosol cloud is visible and then repeat the process three more times to prepare the inhaler for use.
- No dosage adjustment is required for geriatric patients, patients with mild and moderate hepatic impairment, or renally-impaired patients. There are no data available for use of STRIVERDI RESPIMAT in severe hepatically impaired patients.
|offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Olodaterol in adult patients.
|offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Olodaterol in adult patients.
|fdaLIADPed=There is limited information regarding FDA-Labeled Use of Olodaterol in pediatric patients.
|offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Olodaterol in pediatric patients.
|offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Olodaterol in pediatric patients.
|contraindications=* All LABA are contraindicated in patients with asthma without use of a long-term asthma control medication. STRIVERDI RESPIMAT is not indicated for the treatment of asthma.
|warnings=====Precautions====
- Asthma-Related Death
- Data from a large placebo-controlled study in asthma patients showed that long-acting beta2-adrenergic agonists may increase the risk of asthma-related death. Data are not available to determine whether the rate of death in patients with COPD is increased by long-acting beta2-adrenergic agonists.
- A 28-week, placebo-controlled US study comparing the safety of another long-acting beta2-adrenergic agonist (salmeterol) with placebo, each added to usual asthma therapy, showed an increase in asthma-related deaths in patients receiving salmeterol (13/13,176 in patients treated with salmeterol vs. 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34). The increased risk of asthma-related death is considered a class effect of long-acting beta2-adrenergic agonists, including STRIVERDI RESPIMAT. No study adequate to determine whether the rate of asthma-related death is increased in patients treated with STRIVERDI RESPIMAT has been conducted. The safety and efficacy of STRIVERDI RESPIMAT in patients with asthma have not been established. STRIVERDI RESPIMAT is not indicated for the treatment of asthma.
- Deterioration of Disease and Acute Episodes
- STRIVERDI RESPIMAT should not be initiated in patients with acutely deteriorating COPD, which may be a life-threatening condition. STRIVERDI RESPIMAT has not been studied in patients with acutely deteriorating COPD. The use of STRIVERDI RESPIMAT in this setting is inappropriate.
- STRIVERDI RESPIMAT should not be used for the relief of acute symptoms, i.e., as rescue therapy for the treatment of acute episodes of bronchospasm. STRIVERDI RESPIMAT has not been studied in the relief of acute symptoms and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled short-acting beta2-agonist.
- When beginning STRIVERDI RESPIMAT, patients who have been taking inhaled, short-acting beta2-agonists on a regular basis (e.g., four times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. When prescribing STRIVERDI RESPIMAT, the healthcare provider should also prescribe an inhaled, short-acting beta2-agonist and instruct the patient on how it should be used. Increasing inhaled beta2-agonist use is a signal of deteriorating disease for which prompt medical attention is indicated.
- COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If STRIVERDI RESPIMAT no longer controls symptoms of bronchoconstriction, or the patient’s inhaled, short-acting beta2-agonist becomes less effective or the patient needs more inhalation of short-acting beta2-agonist than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dosage of STRIVERDI RESPIMAT beyond the recommended dose is not appropriate in this situation.
- Excessive Use of STRIVERDI RESPIMAT and Use with Long-Acting Beta2-Agonists
- As with other inhaled drugs containing beta2-adrenergic agents, STRIVERDI RESPIMAT should not be used more often than recommended, at higher doses than recommended, or in conjunction with other medications containing long-acting beta2-agonists, as an overdose may result. Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs.
- Paradoxical Bronchospasm
- As with other inhaled beta2-agonists, STRIVERDI RESPIMAT may produce paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs, STRIVERDI RESPIMAT should be discontinued immediately and alternative therapy instituted.
- Cardiovascular Effects
- STRIVERDI RESPIMAT, like other beta2-agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic or diastolic blood pressure, and/or symptoms. If such effects occur, STRIVERDI RESPIMAT may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Long acting beta2-adrenergic agonists should be administered with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, hypertrophic obstructive cardiomyopathy, and hypertension.
- Co-existing Conditions
- STRIVERDI RESPIMAT, like other sympathomimetic amines, should be used with caution in patients with convulsive disorders or thyrotoxicosis, in patients with known or suspected prolongation of the QT interval, and in patients who are unusually responsive to sympathomimetic amines. Doses of the related beta2-agonist albuterol, when administered intravenously, have been reported to aggravate pre-existing diabetes mellitus and ketoacidosis.
- Hypokalemia and Hyperglycemia
- Beta-adrenergic agonists may produce significant hypokalemia in some patients, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation. Inhalation of high doses of beta2-adrenergic agonists may produce increases in plasma glucose.
- In patients with severe COPD, hypokalemia may be potentiated by hypoxia and concomitant treatment, which may increase the susceptibility for cardiac arrhythmias.
- Clinically notable decreases in serum potassium or changes in blood glucose were infrequent during clinical studies with long-term administration of STRIVERDI RESPIMAT with the rates similar to those for placebo controls. STRIVERDI RESPIMAT has not been investigated in patients whose diabetes mellitus is not well controlled.
- Hypersensitivity Reactions
- Immediate hypersensitivity reactions, including angioedema, may occur after administration of STRIVERDI RESPIMAT. If such a reaction occurs, therapy with STRIVERDI RESPIMAT should be stopped at once and alternative treatment should be considered.
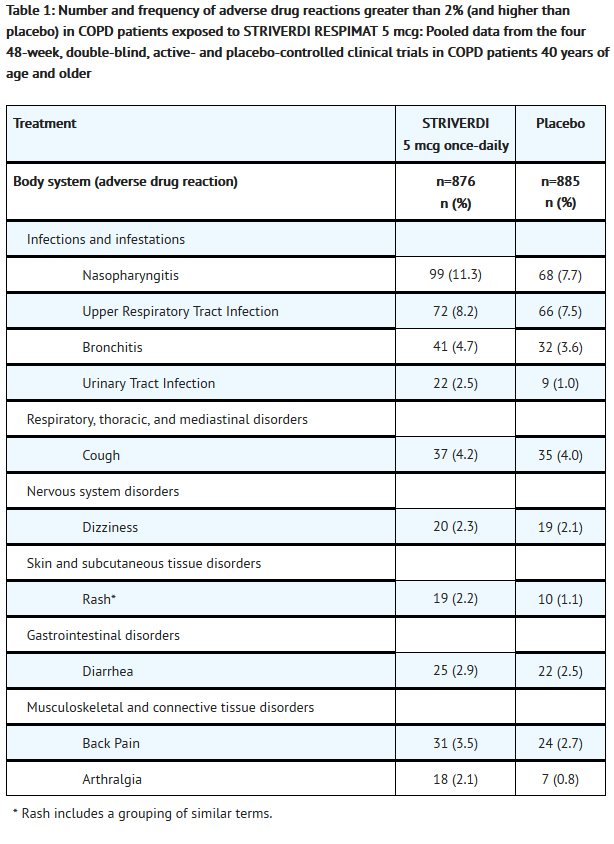
|clinicalTrials=*Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The STRIVERDI RESPIMAT clinical development program included seven dose-ranging trials and eight confirmatory trials. Four of the confirmatory trials were 6-week cross-over trials and four were 48-week parallel group trials. Adverse reactions observed in the dose-ranging trials and four 6-week cross-over trials were consistent with those observed in the 48-week parallel group trials, which formed the primary safety database.
- The primary safety database consisted of pooled data from the four 48-week double-blind, active and placebo-controlled, parallel group confirmatory clinical trials. These trials included 3104 adult COPD patients (77% males and 23% females) 40 years of age and older. Of these patients, 876 and 883 patients were treated with STRIVERDI RESPIMAT 5 mcg and 10 mcg once-daily, respectively. The STRIVERDI RESPIMAT groups were composed of mostly Caucasians (66%) with a mean age of 64 years and a mean percent predicted FEV1 at baseline of 44% for both the 5 mcg and 10 mcg treatment groups. Control arms for comparison included placebo in all four trials plus formoterol 12 mcg in two trials.
- In these four clinical trials, seventy-two percent (72%) of patients exposed to any dose of STRIVERDI RESPIMAT reported an adverse reaction compared to 71% in the placebo group. The proportion of patients who discontinued due to an adverse reaction was 7.2% for STRIVERDI RESPIMAT treated patients compared to 8.8% for placebo treated patients. The adverse reaction most commonly leading to discontinuation was worsening COPD. The most common serious adverse reactions were COPD exacerbation, pneumonia, and atrial fibrillation.
- Table 1 shows all adverse drug reactions reported by at least 2% of patients (and higher than placebo) who received STRIVERDI RESPIMAT 5 mcg during the 48-week trials.
- Additional adverse reactions that occurred in greater than 2% (and higher than placebo) of patients exposed to STRIVERDI RESPIMAT 10 mcg were pneumonia, constipation, and pyrexia.
- Lung cancers were reported in 6 (0.7%), 3 (0.3%), and 2 (0.2%) patients who received STRIVERDI RESPIMAT 10 mcg, 5 mcg, and placebo, respectively.
|postmarketing=There is limited information regarding Postmarketing Experience of Olodaterol in the drug label.
|drugInteractions=* Adrenergic Drugs
- If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of STRIVERDI RESPIMAT may be potentiated.
- Xanthine Derivatives, Steroids, or Diuretics
- Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of STRIVERDI RESPIMAT.
- Non-Potassium Sparing Diuretics
- The ECG changes and/or hypokalemia that may result from the administration of non-potassium sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the co-administration of beta-agonists with non-potassium-sparing diuretics.
- Monoamine Oxidase Inhibitors, Tricyclic Antidepressants, QTc Prolonging Drugs
- STRIVERDI RESPIMAT, as with other beta2-agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants or other drugs known to prolong the QTc interval because the action of adrenergic agonists on the cardiovascular system may be potentiated by these agents. Drugs that are known to prolong the QTc interval may be associated with an increased risk of ventricular arrhythmias.
- Beta-Blockers
- Beta-adrenergic receptor antagonists (beta-blockers) and STRIVERDI RESPIMAT may interfere with the effect of each other when administered concurrently. Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. However, under certain circumstances, e.g. as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
- Inhibitors of Cytochrome P450 and P-gp Efflux Transporter
- In a drug interaction study using the strong dual CYP and P-gp inhibitor ketoconazole, a 1.7-fold increase of maximum plasma concentrations and AUC was observed. STRIVERDI RESPIMAT was evaluated in clinical trials for up to one year at doses up to twice the recommended therapeutic dose. No dose adjustment is necessary.
|useInPregnancyFDA=* Pregnancy Category C
- There are no adequate and well-controlled studies with STRIVERDI RESPIMAT in pregnant women. STRIVERDI RESPIMAT should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- STRIVERDI RESPIMAT was not teratogenic in rats at inhalation doses approximately 2,731 times the maximum recommended human daily inhalation dose (MRHDID) on an AUC basis (at a rat maternal inhalation dose of 1,054 mcg/kg/day). Placental transfer of STRIVERDI RESPIMAT was observed in pregnant rats.
- STRIVERDI RESPIMAT has been shown to be teratogenic in New Zealand rabbits at inhalation doses approximately 7,130 times the MRHDID in adults on an AUC basis (at a rabbit maternal inhalation dose of 2,489 mcg/kg/day). STRIVERDI RESPIMAT exhibited the following fetal toxicities: enlarged or small heart atria or ventricles, eye abnormalities, and split or distorted sternum. No significant effects occurred at an inhalation dose approximately 1,353 times the MRHDID in adults on an AUC basis (at a rabbit maternal inhalation dose of 974 mcg/kg/day).
|useInPregnancyAUS=* Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Olodaterol in women who are pregnant. |useInLaborDelivery=*There are no adequate and well-controlled human studies that have investigated the effects of STRIVERDI RESPIMAT on preterm labor or labor at term. Because of the potential for beta-agonist interference with uterine contractility, use of STRIVERDI RESPIMAT during labor should be restricted to those patients in whom the benefits clearly outweigh the risks. |useInNursing=*Olodaterol, the active component of STRIVERDI RESPIMAT, and/or its metabolites are excreted into the milk of lactating rats. Excretion of olodaterol and/or its metabolites into human milk is probable. There are no human studies that have investigated the effects of STRIVERDI RESPIMAT on nursing infants. Caution should be exercised when STRIVERDI RESPIMAT is administered to nursing women. |useInPed=*STRIVERDI RESPIMAT is not indicated for use in children. The safety and effectiveness of STRIVERDI RESPIMAT in the pediatric population have not been established. |useInGeri=*Based on available data, no adjustment of STRIVERDI RESPIMAT dosage in geriatric patients is necessary.
- Of the 876 patients who received STRIVERDI RESPIMAT at the recommended dose of 5 mcg once-daily in the clinical studies from the pooled 1-year database, 485 were less than or equal to 65 years of age and 391 (44.6%) were greater than 65 years of age.
- No overall differences in effectiveness were observed, and in the 1-year pooled data, the adverse drug reaction profiles were similar in the older population compared to the patient population overall.
|useInGender=There is no FDA guidance on the use of Olodaterol with respect to specific gender populations. |useInRace=There is no FDA guidance on the use of Olodaterol with respect to specific racial populations. |useInRenalImpair=*Subjects with severe renal impairment showed no clinically relevant changes in Cmax or AUC compared to their healthy controls. |useInHepaticImpair=*Subjects with mild and moderate hepatic impairment showed no changes in Cmax or AUC, nor did protein binding differ between mild and moderate hepatically impaired subjects and their healthy controls. A study in subjects with severe hepatic impairment was not performed. |useInReproPotential=There is no FDA guidance on the use of Olodaterol in women of reproductive potentials and males. |useInImmunocomp=There is no FDA guidance one the use of Olodaterol in patients who are immunocompromised.
|administration=* Inhalational |monitoring=There is limited information regarding Monitoring of Olodaterol in the drug label.
|IVCompat=There is limited information regarding IV Compatibility of Olodaterol in the drug label.
|overdose====Acute Overdose===
Signs and Symptoms
- The expected signs and symptoms with overdosage of STRIVERDI RESPIMAT are those of excessive beta-adrenergic stimulation and occurrence or exaggeration of any of the signs and symptoms, e.g., myocardial ischemia, angina pectoris, hypertension or hypotension, tachycardia, arrhythmias, palpitations, dizziness, nervousness, insomnia, anxiety, headache, tremor, dry mouth, muscle spasms, nausea, fatigue, malaise, hypokalemia, hyperglycemia, and metabolic acidosis. As with all inhaled sympathomimetic medications, cardiac arrest and even death may be associated with an overdose of STRIVERDI RESPIMAT.
Management
- Treatment of overdosage consists of discontinuation of STRIVERDI RESPIMAT together with institution of appropriate symptomatic and supportive therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of STRIVERDI RESPIMAT. Cardiac monitoring is recommended in cases of overdosage.
Chronic Overdose
There is limited information regarding Chronic Overdose of Olodaterol in the drug label.
|drugBox={{Drugbox2
| IUPAC_name = 6-hydroxy-8-{(1R)-1-hydroxy-2-{[1-(4-methoxyphenyl)-2-methylpropan-2-yl]amino}ethyl}-4H-1,4-benzoxazin-3-one
| image = Olodaterol00.png
| alt =
| caption =
| tradename = Striverdi | Drugs.com = UK Drug Information | MedlinePlus = | pregnancy_AU = | pregnancy_US = | pregnancy_category= No experience | legal_AU = | legal_CA = | legal_UK = POM | legal_US = | legal_status = | routes_of_administration = Inhalation
| bioavailability = | protein_bound = | metabolism = | elimination_half-life = | excretion =
| CAS_number = 868049-49-4
| ATCvet =
| ATC_prefix = R03
| ATC_suffix = AC19
| UNII = VD2YSN1AFD
| PubChem = 11504295
| DrugBank =
| ChEBI_Ref =
| ChEBI = 82700
| ChEMBL = 605846
| synonyms = BI 1744 CL
| C=21 | H=26 | N=2 | O=5 | molecular_weight = 386.44 g/mol | smiles = CC(C)(CC1=CC=C(C=C1)OC)NCC(C2=CC(=CC3=C2OCC(=O)N3)O)O | ChemSpiderID = 9679097 | InChI = 1/C21H26N2O5/c1-21(2,10-13-4-6-15(27-3)7-5-13)22-11-18(25)16-8-14(24)9-17-20(16)28-12-19(26)23-17/h4-9,18,22,24-25H,10-12H2,1-3H3,(H,23,26)/t18-/m0/s1 | InChIKey = COUYJEVMBVSIHV-SFHVURJKBP | StdInChI = 1S/C21H26N2O5/c1-21(2,10-13-4-6-15(27-3)7-5-13)22-11-18(25)16-8-14(24)9-17-20(16)28-12-19(26)23-17/h4-9,18,22,24-25H,10-12H2,1-3H3,(H,23,26)/t18-/m0/s1 | StdInChIKey = COUYJEVMBVSIHV-SFHVURJKSA-N }}
|mechAction=* Olodaterol is a long-acting beta2-adrenergic agonist (LABA). The compound exerts its pharmacological effects by binding and activation of beta2-adrenoceptors after topical administration by inhalation. Activation of these receptors in the airways results in a stimulation of intracellular adenyl cyclase, an enzyme that mediates the synthesis of cyclic-3’, 5’ adenosine monophosphate (cAMP). Elevated levels of cAMP induce bronchodilation by relaxation of airway smooth muscle cells. In vitro studies have shown that olodaterol has 241-fold greater agonist activity at beta2-adrenoceptors compared to beta1-adrenoceptors and 2,299-fold greater agonist activity compared to beta3-adrenoceptors. The clinical significance of these findings is unknown.
- Beta-adrenoceptors are divided into three subtypes: beta1-adrenoceptors predominantly expressed on cardiac smooth muscle, beta2-adrenoceptors predominantly expressed on airway smooth muscle, and beta3-adrenoceptors predominantly expressed on adipose tissue. Beta2-agonists cause bronchodilation. Although the beta2-adrenoceptor is the predominant adrenergic receptor in the airway smooth muscle, it is also present on the surface of a variety of other cells, including lung epithelial and endothelial cells and in the heart. The precise function of beta2-receptors in the heart is not known, but their presence raises the possibility that even highly selective beta2-agonists may have cardiac effects.
|structure=* The active moiety olodaterol is a selective beta2-adrenergic bronchodilator. The drug substance, olodaterol hydrochloride, is chemically described as 2H-1,4-Benzoxazin-3H(4H)-one, 6-hydroxy-8-[(1R)-1-hydroxy-2-[2-(4-methoxyphenyl)-1,1-dimethylethyl]-amino]ethyl]-, monohydrochloride. Olodaterol hydrochloride is a white to off-white powder that is sparingly-slightly soluble in water and slightly soluble in ethanol. The molecular weight is 422.9 g/mole (salt): 386.5 g/mole (base), and the molecular formula is C21H26N2O5 x HCl as a hydrochloride. The conversion factor from salt to free base is 1.094.
- The structural formula is:
- The drug product, STRIVERDI RESPIMAT, is composed of a sterile, aqueous solution of olodaterol hydrochloride filled into a 4.5 mL plastic container crimped into an aluminum cylinder (STRIVERDI RESPIMAT cartridge) for use with the STRIVERDI RESPIMAT inhaler.
- Excipients include water for injection, benzalkonium chloride, edetate disodium, and anhydrous citric acid. The STRIVERDI RESPIMAT cartridge is only intended for use with the STRIVERDI RESPIMAT inhaler. The STRIVERDI RESPIMAT inhaler is a hand held, pocket sized oral inhalation device that uses mechanical energy to generate a slow-moving aerosol cloud of medication from a metered volume of the drug solution. The STRIVERDI RESPIMAT inhaler has a yellow-colored cap.
- When used with the STRIVERDI RESPIMAT inhaler, each cartridge containing a minimum of 4 grams of a sterile aqueous solution, delivers 60 (or 28) metered actuations after preparation for use, the equivalent of 30 days’ or 14 days’ medication when used as two actuations once a day. Each dose (1 dose equals 2 actuations) from the STRIVERDI RESPIMAT inhaler delivers 5 mcg olodaterol in 22.1 mcL of solution from the mouthpiece. As with all inhaled drugs, the actual amount of drug delivered to the lung may depend on patient factors, such as the coordination between the actuation of the inhaler and inspiration through the delivery system. The duration of inspiration should be at least as long as the spray duration (1.5 seconds).
- Prior to first use, the STRIVERDI RESPIMAT cartridge is inserted into the STRIVERDI RESPIMAT inhaler and the unit is primed. When using for the first time, patients are to actuate the inhaler toward the ground until an aerosol cloud is visible and then repeat the process three more times. The unit is then considered primed and ready for use. If not used for more than 3 days, patients are to actuate the inhaler once to prepare the inhaler for use. If not used for more than 21 days, patients are to actuate the inhaler until an aerosol cloud is visible and then repeat the process three more times to prepare the inhaler for use.
|PD=*Systemic Safety
- The major adverse effects of inhaled beta2-adrenergic agonists occur as a result of excessive activation of systemic beta-adrenergic receptors. The most common adverse effects in adults include skeletal muscle tremor and cramps, insomnia, tachycardia, decreases in serum potassium, and increases in plasma glucose.
- Changes in serum potassium were evaluated in COPD patients in double-blind phase 3 studies. In pooled data, at the recommended 5 mcg dose there was no clinically relevant change compared to placebo in serum potassium.
- Electrophysiology
- The effect of STRIVERDI RESPIMAT on the QT/QTc interval of the ECG was investigated in 24 healthy male and female volunteers in a double-blind, randomized, placebo- and active (moxifloxacin)- controlled study at single doses of 10, 20, 30, and 50 mcg. Dose-dependent QTcI (individual subject corrected QT interval) prolongation was observed. The maximum mean (one-sided 95% upper confidence bound) difference in QTcI from placebo after baseline correction was 2.5 (5.6) ms, 6.1 (9.2) ms, 7.5 (10.7) ms and 8.5 (11.6) ms following doses of 10, 20, 30 and 50 mcg, respectively.
- The effect of 5 mcg and 10 mcg STRIVERDI RESPIMAT on heart rate and rhythm was assessed using continuous 24-hour ECG recording (Holter monitoring) in a subset of 772 patients in the 48-week, placebo-controlled phase 3 trials. There were no dose- or time-related trends or patterns observed for the magnitudes of mean changes in heart rate or premature beats. Shifts from baseline to the end of treatment in premature beats did not indicate meaningful differences between STRIVERDI RESPIMAT 5 mcg, 10 mcg, and placebo.
|PK=*Olodaterol showed linear pharmacokinetics. On repeated once-daily inhalation steady-state of olodaterol plasma concentrations was achieved after 8 days, and the extent of exposure was increased up to 1.8-fold as compared to a single dose.
- Absorption
- Olodaterol reaches maximum plasma concentrations generally within 10 to 20 minutes following drug inhalation. In healthy volunteers, the absolute bioavailability of olodaterol following inhalation was estimated to be approximately 30%, whereas the absolute bioavailability was below 1% when given as an oral solution. Thus, the systemic availability of olodaterol after inhalation is mainly determined by lung absorption, while any swallowed portion of the dose only negligibly contributes to systemic exposure.
- Distribution
- Olodaterol exhibits multi-compartmental disposition kinetics after inhalation as well as after intravenous administration. The volume of distribution is high (1110 L), suggesting extensive distribution into tissue. In vitro binding of [14C] olodaterol to human plasma proteins is independent of concentration and is approximately 60%.
- Metabolism
- Olodaterol is substantially metabolized by direct glucuronidation and by O-demethylation at the methoxy moiety followed by conjugation. Of the six metabolites identified, only the unconjugated demethylation product binds to beta2-receptors. This metabolite, however, is not detectable in plasma after chronic inhalation of the recommended therapeutic dose.
- Cytochrome P450 isozymes CYP2C9 and CYP2C8, with negligible contribution of CYP3A4, are involved in the O-demethylation of olodaterol, while uridine diphosphate glycosyl transferase isoforms UGT2B7, UGT1A1, 1A7, and 1A9 were shown to be involved in the formation of olodaterol glucuronides.
- Elimination
- Total clearance of olodaterol in healthy volunteers is 872 mL/min, and renal clearance is 173 mL/min. The terminal half-life following intravenous administration is 22 hours. The terminal half-life following inhalation in contrast is about 45 hours, indicating that the latter is determined by absorption rather than by elimination processes. However, the effective half-life at daily dose of 5 μg calculated from Cmax from COPD patients is 7.5 hours.
- Following intravenous administration of [14C]-labeled olodaterol, 38% of the radioactive dose was recovered in the urine and 53% was recovered in feces. The amount of unchanged olodaterol recovered in the urine after intravenous administration was 19%. Following oral administration, only 9% of olodaterol and/or its metabolites was recovered in urine, while the major portion was recovered in feces (84%). More than 90% of the dose was excreted within 6 and 5 days following intravenous and oral administration, respectively. Following inhalation, excretion of unchanged olodaterol in urine within the dosing interval in healthy volunteers at steady state accounted for 5% to 7% of the dose.
- Special Populations
- A pharmacokinetic meta-analysis showed that no dose adjustment is necessary based on the effect of age, gender, and weight on systemic exposure in COPD patients after inhalation of STRIVERDI RESPIMAT.
- Renal Impairment
- Olodaterol levels were increased by approximately 40% in subjects with severe renal impairment. A study in subjects with mild and moderate renal impairment was not performed.
- Hepatic Impairment
- Subjects with mild and moderate hepatic impairment showed no changes in Cmax or AUC, nor did protein binding differ between mild and moderate hepatically impaired subjects and their healthy controls. A study in subjects with severe hepatic impairment was not performed.
- Drug-Drug Interactions
- Drug-drug interaction studies were carried out using fluconazole as a model inhibitor of CYP 2C9 and ketoconazole as a potent P-gp (and CYP3A4, 2C8, 2C9) inhibitor.
- Fluconazole: Co-administration of 400 mg fluconazole once a day for 14 days had no relevant effect on systemic exposure to olodaterol.
- Ketoconazole: Co-administration of 400 mg ketoconazole once a day for 14 days increased olodaterol Cmax by 66% and AUC0-1 by 68%.
- Tiotropium: Co-administration of tiotropium bromide, delivered as fixed-dose combination with olodaterol, for 21 days had no relevant effect on systemic exposure to olodaterol, and vice versa.
|nonClinToxic=*Two-year inhalation studies were conducted in rats and mice to assess the carcinogenic potential of olodaterol. Lifetime treatment of female rats induced leiomyomas of the mesovarium at doses of 25.8 and 270 mcg/kg/day (approximately 18- and 198-fold, respectively, the MRHDID on an AUC basis). No tumor findings were observed in male rats at doses up to 270 mcg/kg/day (approximately 230-fold the MRHDID on an AUC basis). Lifetime treatment of female mice induced leiomyomas and leiomyosarcomas of the uterus at doses ≥76.9 mcg/kg/day (approximately 106-fold the MRHDID on an AUC basis). No tumor findings were observed in male mice at doses up to 255 mcg/kg/day (approximately 455-fold the MRHDID on an AUC basis). Increases in leiomyomas and leiomyosarcomas of the female rodent reproductive tract have been similarly demonstrated with other β2-adrenergic agonist drugs. The relevance of these findings to human use is unknown.
- Olodaterol was not mutagenic in the in vitro Ames test or in the in vitro mouse lymphoma assay. Olodaterol produced increased frequency of micronuclei in rats after intravenous doses. The increased frequency of micronuclei was likely related to drug enhanced (compensatory) erythropoiesis. The mechanism for induction of micronuclei formation is likely not relevant at clinical exposures.
- Olodaterol did not impair male or female fertility in rats at inhalation doses up to 3,068 mcg/kg/day (approximately 2,322 times the MRHDID on an AUC basis).
|clinicalStudies=*The STRIVERDI RESPIMAT clinical development program included three dose-ranging trials in COPD patients, four dose-ranging trials in asthma patients, and eight confirmatory trials in patients with COPD.
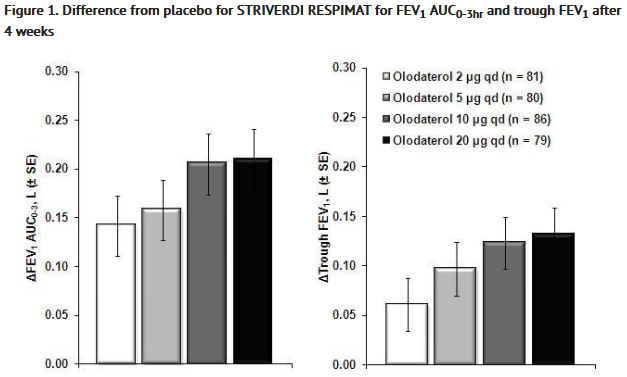
- Dose-ranging trials
- The first COPD dose-ranging trial was a randomized, double-blind, placebo-controlled, single-dose, 5-way cross-over trial in 36 patients. Results demonstrated dose-related improvements in forced expiratory volume in one second (FEV1) compared to placebo. The difference in trough FEV1 from placebo for the 2, 5, 10, and 20 mcg doses were 0.07L (95% CI 0.03, 0.11), 0.10L (0.06, 0.14), 0.11L (0.07, 0.15), and 0.12L (0.08, 0.16), respectively. The second COPD dose-ranging trial was a 4-week, randomized, double-blind, placebo-controlled, parallel group trial in 405 patients. Dose-related improvements in lung function were also seen, with no added benefit of the 20 mcg dose over the 10 mcg dose (Figure 1). The third COPD dose-ranging trial was a randomized, double-blind, 4-way cross-over, dose-regimen trial in 47 patients. Treatment arms included 2 mcg twice-daily, 5 mcg once-daily, 5 mcg twice-daily, and 10 mcg once-daily. There was no clear difference in treatment effect when comparing twice-daily dosing to once-daily dosing.
- Four randomized, double-blind, placebo-controlled dose-ranging trials were performed in patients with asthma, evaluating doses from 2 to 20 mcg. Results from patients with asthma were consistent with results from dose-ranging trials in patients with COPD.
- STRIVERDI RESPIMAT is not indicated for asthma.
- Based upon the results of the dose-ranging trials, 5 and 10 mcg doses were further evaluated in the confirmatory COPD trials.
- Confirmatory Trials
- The eight confirmatory trials in the STRIVERDI RESPIMAT clinical development program were four pairs of replicate, randomized, double-blind, placebo-controlled trials in 3533 COPD patients (1281 received the 5 mcg dose, 1284 received the 10 mcg dose):
(i) two replicate, placebo-controlled, parallel group, 48 week trials (Trials 1 and 2) (ii) two replicate, placebo- and active- [[[formoterol]] 12 mcg twice-daily] controlled, parallel group, 48-week trials (Trials 3 and 4) (iii) two replicate, placebo- and active- [[[formoterol]] 12 mcg twice-daily] controlled, 6-week cross-over trials (Trials 5 and 6) (iv) two replicate, placebo- and active- [[[tiotropium bromide]] 18 mcg once-daily] controlled, 6-week cross-over trials (Trials 7 and 8).
- These eight trials enrolled patients who were 40 years of age or older with a clinical diagnosis of COPD, a smoking history of at least 10 pack-years, and moderate to very severe pulmonary impairment (post-bronchodilator FEV1 less than 80% predicted normal [GOLD II – IV] and a post-bronchodilator FEV1 to FVC ratio of less than 70%).
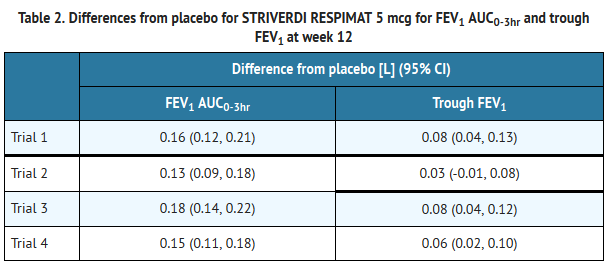
- The majority of the 3104 patients in the 48-week trials (Trials 1 and 2, Trials 3 and 4) were male (77%), white (66%) or Asian (32%), with a mean age of 64 years. Mean post-bronchodilator FEV1 was 1.38 L (GOLD II [50%], GOLD III [40%], GOLD IV [10%]). Mean beta2-agonist responsiveness was 15% of baseline (0.16 L). With the exception of other LABAs, all pulmonary medications were allowed as concomitant therapy (e.g., tiotropium [24%], ipratropium [25%], inhaled corticosteroids [45%], xanthines [16%]); patient enrollment was stratified by tiotropium use. In all four trials, the primary efficacy endpoints were change from pre-treatment baseline in FEV1 AUC0-3 and trough (pre-dose) FEV1 (after 12 weeks in Trials 1 and 2; after 24 weeks in Trials 3 and 4).
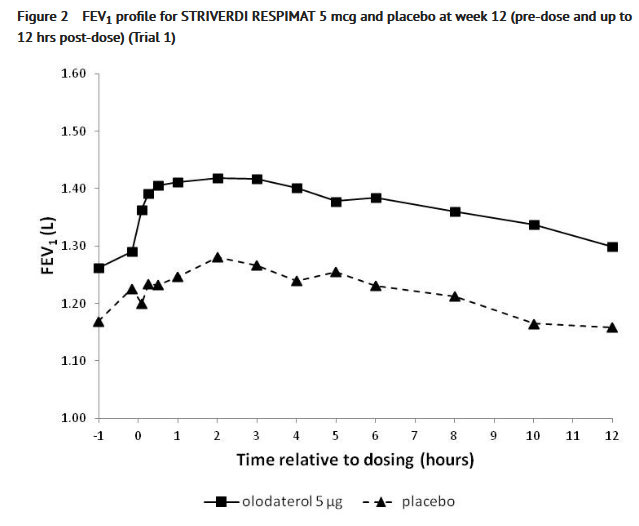
- In all four 48-week trials, STRIVERDI RESPIMAT 5 mcg demonstrated significant improvements in FEV1 AUC 0-3hr compared to placebo at week 12 (Table 2) and at week 24. In the four 48-week trials, STRIVERDI RESPIMAT 5 mcg demonstrated significant improvements in trough FEV1 compared to placebo at week 12 (Table 2; 3 of 4 trials) and at week 24 (4 trials). STRIVERDI RESPIMAT 5 mcg demonstrated a bronchodilatory treatment effect at 5 minutes after the first dose with a mean increase in FEV1 compared to placebo of 0.11L (range: 0.10L to 0.12L). The 10 mcg dose demonstrated no additional benefit over the 5 mcg dose (data not shown). Patients treated with STRIVERDI RESPIMAT 5 mcg used less rescue albuterol compared to patients treated with placebo.
- In Trials 1 and 2, serial spirometric evaluations were performed pre-dose and up to 12 hours after dosing in a sub-group of 562 patients (201 patients receiving STRIVERDI RESPIMAT 5 mcg, 192 patients receiving 10 mcg, and 169 patients receiving placebo) after 12 weeks of treatment. Dosing occurred at approximately the same time of the day in the morning. The spirometric curves from Trial 1 are displayed in Figure 2.
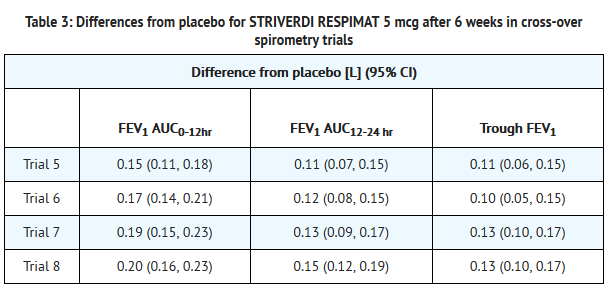
- The bronchodilatory profile of STRIVERDI RESPIMAT 5 mcg over the 24 hour dosing interval was evaluated in two pairs of replicate, placebo- and active-controlled, 6 week cross-over trials in 199 patients (Trials 5 and 6) and 230 patients (Trials 7 and 8) with moderate to very severe COPD. Mean beta2-agonist responsiveness ranged from 14% -21% of baseline (0.18 to 0.22 L). All pulmonary medications were allowed as concomitant therapy with the exception of other LABAs (all trials) and anti-cholinergics (Trials 7 and 8). In all four trials, the primary endpoints were change from pre-treatment baseline in FEV1 AUC0-12hr and FEV1 AUC12-24hr after 6 weeks; although not a primary endpoint, trough FEV1 was also measured after 6 weeks. Results are shown in Table 3.
|howSupplied=* STRIVERDI RESPIMAT Inhalation Spray is supplied in a labeled carton containing one STRIVERDI RESPIMAT cartridge and one STRIVERDI RESPIMAT inhaler.
- The STRIVERDI RESPIMAT cartridge is an aluminum cylinder with a tamper protection seal on the cap. The STRIVERDI RESPIMAT cartridge is only intended for use with the STRIVERDI RESPIMAT inhaler.
- The STRIVERDI RESPIMAT inhaler is a cylindrical-shaped plastic inhalation device with a gray-colored body and a clear base. The clear base is removed to insert the cartridge. The inhaler contains a dose indicator. The yellow colored cap and the written information on the label of the gray inhaler body indicates that it is labeled for use with the STRIVERDI RESPIMAT cartridge.
- STRIVERDI RESPIMAT Inhalation Spray is available as:
- STRIVERDI RESPIMAT Inhalation Spray: 60 metered actuations (NDC 0597-0192-61)
- STRIVERDI RESPIMAT Inhalation Spray: 28 metered actuations (NDC 0597-0192-31) (institutional pack)
- The STRIVERDI RESPIMAT cartridge has a net fill weight of at least 4 grams and when used with the STRIVERDI RESPIMAT inhaler, is designed to deliver the labeled number of metered actuations (60 or 28) after preparation for use; which is respectively equivalent to 30 or 14 days of medication when used according to the directions for use (one dose equals two actuations).
- When the labeled number of metered actuations (60 or 28) has been dispensed from the inhaler, the STRIVERDI RESPIMAT locking mechanism will be engaged and no more actuations can be dispensed.
- After assembly, the STRIVERDI RESPIMAT inhaler should be discarded at the latest 3 months after first use or when the locking mechanism is engaged, whichever comes first.
- Keep out of reach of children. Do not spray into eyes.
- Storage
- Store at 25°C (77°F); excursions permitted to 15°C–30°C (59°F–86°F). Avoid freezing.
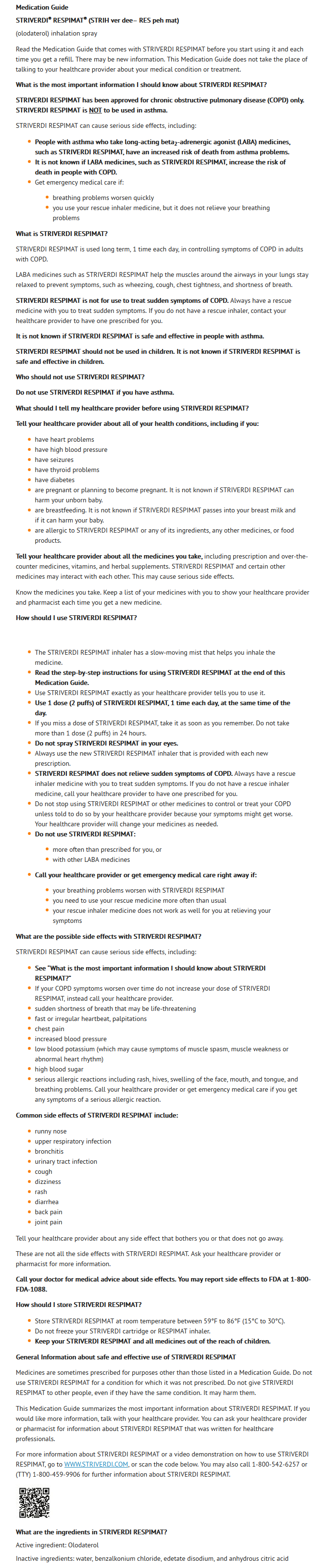
|fdaPatientInfo=*Asthma-Related Death
- Preparation for Use and Priming
- Instruct patients that priming STRIVERDI RESPIMAT is essential to ensure appropriate content of the medication in each actuation.
- When using the unit for the first time, the STRIVERDI RESPIMAT cartridge is inserted into the STRIVERDI RESPIMAT inhaler and the unit is primed. STRIVERDI RESPIMAT patients are to actuate the inhaler toward the ground until an aerosol cloud is visible and then repeat the process three more times. The unit is then considered primed and ready for use. If not used for more than 3 days, patients are to actuate the inhaler once to prepare the inhaler for use. If not used for more than 21 days, patients are to actuate the inhaler until an aerosol cloud is visible and then repeat the process three more times to prepare the inhaler for use.
- Not for Acute Symptoms
- STRIVERDI RESPIMAT is not meant to relieve acute asthma symptoms or exacerbations of COPD and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist such as albuterol. (The healthcare provider should provide the patient with such medication and instruct the patient in how it should be used.)
- Instruct patients to notify their physician immediately if they experience any of the following:
- Worsening of symptoms
- Decreasing effectiveness of inhaled, short-acting beta2-agonists
- Need for more inhalations than usual of inhaled, short-acting beta2-agonists
- Significant decrease in lung function as outlined by the physician
- Instruct patients not to stop therapy with STRIVERDI RESPIMAT without physician/provider guidance since symptoms may recur after discontinuation.
- Do Not Use Additional Long-Acting Beta2-Agonists
- Patients who have been taking inhaled, short-acting beta2-agonists on a regular basis should be instructed to discontinue the regular use of these products and use them only for the symptomatic relief of acute symptoms.
- When patients are prescribed STRIVERDI RESPIMAT, other inhaled medications containing long-acting beta2-agonists should not be used. Patients should not use more than the recommended once-daily dose of STRIVERDI RESPIMAT. Excessive use of sympathomimetics may cause significant cardiovascular effects, and may be fatal.
- Risks Associated with Beta2-Agonist Therapy
- Inform patients of adverse effects associated with beta2-agonists, such as palpitations, chest pain, rapid heart rate, tremor, or nervousness.
|alcohol=* Alcohol-Olodaterol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
|brandNames=* STRIVERDI RESPIMAT®[1]
|lookAlike= |drugShortage= }} {{#subobject:
|Page Name=Olodaterol
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol06.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol07.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol08.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol09.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol10.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol11.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol12.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol13.png
}}
{{#subobject:
|Label Page=Olodaterol |Label Name=Olodaterol14.png
}}