Moxifloxacin warnings and precautions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
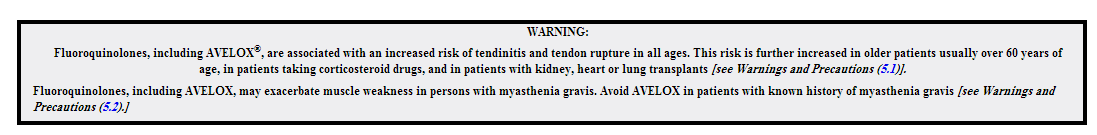
WARNINGS AND PRECAUTIONS
Tendinopathy and Tendon Rupture
Fluoroquinolones, including AVELOX, are associated with an increased risk of tendinitis and tendon rupture in all ages. This adverse reaction most frequently involves the Achilles tendon, and rupture of the Achilles tendon may require surgical repair. Tendinitis and tendon rupture in the rotator cuff (the shoulder), the hand, the biceps, the thumb, and other tendon sites have also been reported. The risk of developing fluoroquinolone-associated tendinitis and tendon rupture is further increased in older patients usually over 60 years of age, in patients taking corticosteroid drugs, and in patients with kidney, heart or lung transplants. Factors, in addition to age and corticosteroid use, that may independently increase the risk of tendon rupture include strenuous physical activity, renal failure, and previous tendon disorders such as rheumatoid arthritis. Tendinitis and tendon rupture have also occurred in patients taking fluoroquinolones who do not have the above risk factors. Tendon rupture can occur during or after completion of therapy; cases occurring up to several months after completion of therapy have been reported. AVELOX should be discontinued if the patient experiences pain, swelling, inflammation or rupture of a tendon. Patients should be advised to rest at the first sign of tendinitis or tendon rupture, and to contact their healthcare provider regarding changing to a non-quinolone antimicrobial drug. [see Adverse Reactions (6.4) and Patient Counseling Information (17.3).]
Exacerbation of Myasthenia Gravis
Fluoroquinolones, including AVELOX, have neuromuscular blocking activity and may exacerbate muscle weakness in persons with myasthenia gravis. Postmarketing serious adverse events, including deaths and requirement for ventilatory support, have been associated with fluoroquinolone use in persons with myasthenia gravis. Avoid AVELOX in patients with known history of myasthenia gravis [see Patient Counseling Information (17.3)].
QT Prolongation
AVELOX has been shown to prolong the QT interval of the electrocardiogram in some patients. Following oral dosing with 400 mg of AVELOX the mean (± SD) change in QTc from the pre-dose value at the time of maximum drug concentration was 6 msec (± 26) (n = 787). Following a course of daily intravenous dosing (400 mg; 1 hour infusion each day) the mean change in QTc from the Day 1 pre-dose value was 10 msec (±22) on Day 1 (n=667) and 7 msec (± 24) on Day 3 (n = 667).
The drug should be avoided in patients with known prolongation of the QT interval, patients with uncorrected hypokalemia and patients receiving Class IA (for example, quinidine, procainamide) or Class III (for example,amiodarone, sotalol) antiarrhythmic agents, due to the lack of clinical experience with the drug in these patient populations.
Pharmacokinetic studies between AVELOX and other drugs that prolong the QT interval such as cisapride, erythromycin, antipsychotics, and tricyclic antidepressants have not been performed. An additive effect of AVELOX and these drugs cannot be excluded; therefore caution should be exercised when AVELOX is given concurrently with these drugs. In premarketing clinical trials, the rate of cardiovascular adverse events was similar in 798 AVELOX and 702 comparator treated patients who received concomitant therapy with drugs known to prolong the QTc interval.
AVELOX should be used with caution in patients with ongoing proarrhythmic conditions, such as clinically significant bradycardia, acute myocardial ischemia. The magnitude of QT prolongation may increase with increasing concentrations of the drug or increasing rates of infusion of the intravenous formulation. Therefore the recommended dose or infusion rate should not be exceeded. QT prolongation may lead to an increased risk for ventricular arrhythmias including torsade de pointes. No excess in cardiovascular morbidity or mortality attributable to QTc prolongation occurred with AVELOX treatment in over 15,500 patients in controlled clinical studies, including 759 patients who were hypokalemic at the start of treatment, and there was no increase in mortality in over 18,000 AVELOX tablet treated patients in a postmarketing observational study in which ECGs were not performed. Elderly patients using IV AVELOX may be more susceptible to drug-associated QT prolongation. [see Use In Specific Populations, (8.5).] In addition, AVELOX should be used with caution in patients with mild, moderate, or severe liver cirrhosis. [See Clinical Pharmacology (12.3) and Patient Counseling Information (17.3).]
Hypersensitivity Reactions
Serious anaphylactic reactions, some following the first dose, have been reported in patients receiving quinolone therapy, including AVELOX. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, pharyngeal or facial edema, dyspnea, urticaria, and itching. Serious anaphylactic reactions require immediate emergency treatment with epinephrine. AVELOX should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity. Oxygen, intravenous steroids, and airway management, including intubation, may be administered as indicated.[see Adverse Reactions (6) and Patient Counseling Information (17.3).]
Other Serious and Sometimes Fatal Reactions
Other serious and sometimes fatal events, some due to hypersensitivity, and some due to uncertain etiology, have been reported rarely in patients receiving therapy with quinolones, including AVELOX . These events may be severe and generally occur following the administration of multiple doses. Clinical manifestations may include one or more of the following:
• Fever, rash, or severe dermatologic reactions (for example, toxic epidermal necrolysis, Stevens-Johnson syndrome) • Vasculitis; arthralgia; myalgia; serum sickness • Allergic pneumonitis • Interstitial nephritis; acute renal insufficiency or failure • Hepatitis; jaundice; acute hepatic necrosis or failure • Anemia, including hemolytic and aplastic; thrombocytopenia, including thrombotic thrombocytopenic purpura; leukopenia; agranulocytosis; pancytopenia; and/or other hematologic abnormalities
The drug should be discontinued immediately at the first appearance of a skin rash, jaundice, or any other sign of hypersensitivity and supportive measures instituted [see Patient Counseling Information (17.3) and Adverse Reactions (6.4).
Central Nervous System Effects
Fluoroquinolones, including AVELOX, may cause central nervous system (CNS) events, including: nervousness, agitation, insomnia, anxiety, nightmares or paranoia [see Adverse Reactions (6.2, 6.4)].
Convulsions and increased intracranial pressure (including pseudotumor cerebri) have been reported in patients receiving fluoroquinolones. Fluoroquinolones may also cause central nervous system (CNS) events including: dizziness, confusion, tremors, hallucinations, depression, and, rarely, suicidal thoughts or acts. These reactions may occur following the first dose. If these reactions occur in patients receiving AVELOX, the drug should be discontinued and appropriate measures instituted. As with all fluoroquinolones, AVELOX should be used with caution in patients with known or suspected CNS disorders (for example, severe cerebral arteriosclerosis, epilepsy) or in the presence of other risk factors that may predispose to seizures or lower the seizure threshold. [See Drug Interactions (7.4) Adverse Reactions (6.2, 6.4) and Patient Counseling Information (17.3).]
Clostridium Difficile-Associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including AVELOX, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated [see Adverse Reactions (6.2) and Patient Counseling Information (17.3)].
Peripheral Neuropathy
Cases of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias and weakness have been reported in patients receiving fluoroquinolones including AVELOX. Symptoms may occur soon after initiation of AVELOX and may be irreversible. AVELOX should be discontinued immediately if the patient experiences symptoms of peripheral neuropathy including pain, burning, tingling, numbness, and/or weakness or other alterations of sensation including light touch, pain, temperature, position sense, and vibratory sensation [see Adverse Reactions (6.2, 6.4) and Patient Counseling Information (17.3)].
Arthropathic Effects in Animals
The oral administration of AVELOX caused lameness in immature dogs. Histopathological examination of the weight-bearing joints of these dogs revealed permanent lesions of the cartilage. Related quinolone-class drugs also produce erosions of cartilage of weight-bearing joints and other signs of arthropathy in immature animals of various species. [See Animal Toxicology and/or Pharmacology (13.2).]
Photosensitivity/Phototoxicity
Moderate to severe photosensitivity/phototoxicity reactions, the latter of which may manifest as exaggerated sunburn reactions (for example, burning, erythema, exudation, vesicles, blistering, edema) involving areas exposed to light (typically the face, “V” area of the neck, extensor surfaces of the forearms, dorsa of the hands), can be associated with the use of quinolone antibiotics after sun or UV light exposure. Therefore, excessive exposure to these sources of light should be avoided. Drug therapy should be discontinued if phototoxicity occurs. [see Adverse Reactions (6.4) and Pharmacokinetics (12.3).]
Development of Drug Resistant Bacteria
Prescribing AVELOX in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria
USE IN SPECIFIC POPULATIONS
Pregnancy
Pregnancy Category C.
Because no adequate or well-controlled studies have been conducted in pregnant women, AVELOX should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Moxifloxacin was not teratogenic when administered to pregnant rats during organogenesis at oral doses as high as 500 mg/kg/day or 0.24 times the maximum recommended human dose based on systemic exposure (AUC), but decreased fetal body weights and slightly delayed fetal skeletal development (indicative of fetotoxicity) were observed. Intravenous administration of 80 mg/kg/day (approximately 2 times the maximum recommended human dose based on body surface area (mg/m2) to pregnant rats resulted in maternal toxicity and a marginal effect on fetal and placental weights and the appearance of the placenta. There was no evidence of teratogenicity at intravenous doses as high as 80 mg/kg/day. Intravenous administration of 20 mg/kg/day (approximately equal to the maximum recommended human oral dose based upon systemic exposure) to pregnant rabbits during organogenesis resulted in decreased fetal body weights and delayed fetal skeletal ossification. When rib and vertebral malformations were combined, there was an increased fetal and litter incidence of these effects. Signs of maternal toxicity in rabbits at this dose included mortality, abortions, marked reduction of food consumption, decreased water intake, body weight loss and hypoactivity. There was no evidence of teratogenicity when pregnant cynomolgus monkeys were given oral doses as high as 100 mg/kg/day (2.5 times the maximum recommended human dose based upon systemic exposure). An increased incidence of smaller fetuses was observed at 100 mg/kg/day. In an oral pre- and postnatal development study conducted in rats, effects observed at 500 mg/kg/day included slight increases in duration of pregnancy and prenatal loss, reduced pup birth weight and decreased neonatal survival. Treatment-related maternal mortality occurred during gestation at 500 mg/kg/day in this study.
Nursing Mothers
Moxifloxacin is excreted in the breast milk of rats. Moxifloxacin may also be excreted in human milk. Because of the potential for serious adverse reactions in infants who are nursing from mothers taking AVELOX, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients and adolescents less than 18 years of age have not been established. AVELOX causes arthropathy in juvenile animals [see Boxed Warning, Warnings and Precautions (5.9), and Clinical Pharmacology (12.3)].
Geriatric Use
Geriatric patients are at increased risk for developing severe tendon disorders including tendon rupture when being treated with a fluoroquinolone such as AVELOX. This risk is further increased in patients receiving concomitant corticosteroid therapy. Tendinitis or tendon rupture can involve the Achilles, hand, shoulder, or other tendon sites and can occur during or after completion of therapy; cases occurring up to several months after fluoroquinolone treatment have been reported. Caution should be used when prescribing AVELOX to elderly patients especially those on corticosteroids. Patients should be informed of this potential side effect and advised to discontinue AVELOX and contact their healthcare provider if any symptoms of tendinitis or tendon rupture occur.[see Boxed Warning, Warnings and Precautions (5.1), and Adverse Reactions (6.2).]
In controlled multiple-dose clinical trials, 23% of patients receiving oral AVELOX were greater than or equal to 65 years of age and 9% were greater than or equal to 75 years of age. The clinical trial data demonstrate that there is no difference in the safety and efficacy of oral AVELOX in patients aged 65 or older compared to younger adults.
In trials of intravenous use, 42% of AVELOX patients were greater than or equal to 65 years of age, and 23% were greater than or equal to 75 years of age. The clinical trial data demonstrate that the safety of intravenous AVELOX in patients aged 65 or older was similar to that of comparator-treated patients. In general, elderly patients may be more susceptible to drug-associated effects of the QT interval. Therefore, AVELOX should be avoided in patients taking drugs that can result in prolongation of the QT interval (for example, class IA or class III antiarrhythmics) or in patients with risk factors for torsade de pointes (for example, known QT prolongation, uncorrected hypokalemia). [see Warnings and Precautions (5.3), Drug Interactions (7.4), and Clinical Pharmacology (12.3).]
Renal Impairment
The pharmacokinetic parameters of moxifloxacin are not significantly altered in mild, moderate, severe, or end-stage renal disease. No dosage adjustment is necessary in patients with renal impairment, including those patients requiring hemodialysis (HD) or continuous ambulatory peritoneal dialysis (CAPD)[see Dosage and Administration (2), and Clinical Pharmacology (12.3).]
Hepatic Impairment
No dosage adjustment is recommended for mild, moderate, or severe hepatic insufficiency (Child-Pugh Classes A, B, or C). However, due to metabolic disturbances associated with hepatic insufficiency, which may lead to QT prolongation, AVELOX should be used with caution in these patients
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals to determine the carcinogenic potential of moxifloxacin have not been performed.
Moxifloxacin was not mutagenic in 4 bacterial strains (TA 98, TA 100, TA 1535, TA 1537) used in the Ames Salmonella reversion assay. As with other quinolones, the positive response observed with moxifloxacin in strain TA 102 using the same assay may be due to the inhibition of DNA gyrase. Moxifloxacin was not mutagenic in the CHO/HGPRT mammalian cell gene mutation assay. An equivocal result was obtained in the same assay when v79 cells were used. Moxifloxacin was clastogenic in the v79 chromosome aberration assay, but it did not induce unscheduled DNA synthesis in cultured rat hepatocytes. There was no evidence of genotoxicity in vivo in a micronucleus test or a dominant lethal test in mice.
Moxifloxacin had no effect on fertility in male and female rats at oral doses as high as 500 mg/kg/day, approximately 12 times the maximum recommended human dose based on body surface area (mg/m2), or at intravenous doses as high as 45 mg/kg/day, approximately equal to the maximum recommended human dose based on body surface area (mg/m2). At 500 mg/kg orally there were slight effects on sperm morphology (head-tail separation) in male rats and on the estrous cycle in female rats.
References
http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/21277slr018,21085slr023_avelox_lbl.pdf