Lidocaine (patch)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Lidocaine (patch) is an anesthetic agent that is FDA approved for the treatment of pain associated with post-herpetic neuralgia. Common adverse reactions include hypotension, nausea, dermatitis, hypersensitivity, pruritus and urticaria.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- LIDODERM is indicated for relief of pain associated with post-herpetic neuralgia. It should be applied only to intact skin.
Dosage
- Apply LIDODERM to intact skin to cover the most painful area. Apply the prescribed number of patches (maximum of 3), only once for up to 12 hours within a 24 hour period. Patches may be cut into smaller sizes with scissors prior to removal of the release liner.Clothing may be worn over the area of application. Smaller areas of treatment are recommended in a debilitated patient, or a patient with impaired elimination.
- If irritation or a burning sensation occurs during application, remove the patch(es) and do not reapply until the irritation subsides.
- When LIDODERM is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lidocaine (patch) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lidocaine (patch) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Label Guideline-Supported Use of Lidocaine (patch) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lidocaine (patch) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lidocaine (patch) in pediatric patients.
Contraindications
- LIDODERM is contraindicated in patients with a known history of sensitivity to local anesthetics of the amide type, or to any other component of the product.
Warnings
Accidental Exposure in Children
- Even a used LIDODERM patch contains a large amount of lidocaine (at least 665 mg). The potential exists for a small child or a pet to suffer serious adverse effects from chewing or ingesting a new or used LIDODERM patch, although the risk with this formulation has not been evaluated. It is important for patients to store and dispose of LIDODERM out of the reach of children, pets and others.
Excessive Dosing
- Excessive dosing by applying LIDODERM to larger areas or for longer than the recommended wearing time could result in increased absorption of lidocaine and high blood concentrations, leading to serious adverse effects. Lidocaine toxicity could be expected at lidocaine blood concentrations above 5 µg/mL. The blood concentration of lidocaine is determined by the rate of systemic absorption and elimination. Longer duration of application, application of more than the recommended number of patches, smaller patients, or impaired elimination may all contribute to increasing the blood concentration of lidocaine. With recommended dosing of LIDODERM, the average peak blood concentration is about 0.13 µg/mL, but concentrations higher than 0.25 µg/mL have been observed in some individuals.
PRECAUTIONS
General
Hepatic Disease
- Patients with severe hepatic disease are at greater risk of developing toxic blood concentrations of lidocaine, because of their inability to metabolize lidocaine normally.
Allergic Reactions
- Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine. However, LIDODERM should be used with caution in patients with a history of drug sensitivities, especially if the etiologic agent is uncertain.
Non-intact Skin
- Application to broken or inflamed skin, although not tested, may result in higher blood concentrations of lidocaine from increased absorption. LIDODERM is only recommended for use on intact skin.
External Heat Sources
- Placement of external heat sources, such as heating pads or electric blankets, over LIDODERM patches is not recommended as this has not been evaluated and may increase plasma lidocaine levels.
Eye Exposure
- The contact of LIDODERM with eyes, although not studied, should be avoided based on the findings of severe eye irritation with the use of similar products in animals. If eye contact occurs, immediately wash out the eye with water or saline and protect the eye until sensation returns.
Adverse Reactions
Clinical Trials Experience
Application Site Reactions
- During or immediately after treatment with LIDODERM (lidocaine patch 5%), the skin at the site of application may develop blisters, bruising, burning sensation, depigmentation, dermatitis, discoloration, edema, erythema, exfoliation, irritation, papules, petechia, pruritus, vesicles, or may be the locus of abnormal sensation. These reactions are generally mild and transient, resolving spontaneously within a few minutes to hours.
Allergic Reactions
- Allergic and anaphylactoid reactions associated with lidocaine, although rare, can occur. They are characterized by angioedema, bronchospasm, dermatitis, dyspnea, hypersensitivity, laryngospasm, pruritus, shock, and urticaria. If they occur, they should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
Postmarketing Experience
- Due to the nature and limitation of spontaneous reports in postmarketing surveillance, causality has not been established for additional reported adverse events including:
- Asthenia, confusion, disorientation, dizziness, headache, hyperesthesia, hypoesthesia, lightheadedness, metallic taste, nausea, nervousness, pain exacerbated, paresthesia, somnolence, taste alteration, vomiting, visual disturbances such as blurred vision, flushing, tinnitus, and tremor.
Systemic (Dose-Related) Reactions
- Systemic adverse reactions following appropriate use of LIDODERM are unlikely, due to the small dose absorbed. Systemic adverse effects of lidocaine are similar in nature to those observed with other amide local anesthetic agents, including CNS excitation and/or depression (light headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest). Excitatory CNS reactions may be brief or not occur at all, in which case the first manifestation may be drowsiness merging into unconsciousness. Cardiovascular manifestations may include bradycardia, hypotension and cardiovascular collapse leading to arrest.
Drug Interactions
Antiarrhythmic Drugs
- LIDODERM should be used with caution in patients receiving Class I antiarrhythmic drugs (such as tocainide and mexiletine) since the toxic effects are additive and potentially synergistic.
Local Anesthetics
- When LIDODERM is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Teratogenic Effects
Pregnancy Category B.
- LIDODERM (lidocaine patch 5%) has not been studied in pregnancy. Reproduction studies with lidocaine have been performed in rats at doses up to 30 mg/kg subcutaneously and have revealed no evidence of harm to the fetus due to lidocaine. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, LIDODERM should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lidocaine (patch) in women who are pregnant.
Labor and Delivery
- LIDODERM has not been studied in labor and delivery. Lidocaine is not contraindicated in labor and delivery. Should LIDODERM be used concomitantly with other products containing lidocaine, total doses contributed by all formulations must be considered.
Nursing Mothers
- LIDODERM has not been studied in nursing mothers. Lidocaine is excreted in human milk, and the milk:plasma ratio of lidocaine is 0.4. Caution should be exercised when LIDODERM is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
There is no FDA guidance on the use of Lidocaine (patch) in geriatric settings.
Gender
There is no FDA guidance on the use of Lidocaine (patch) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lidocaine (patch) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Lidocaine (patch) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Lidocaine (patch) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Lidocaine (patch) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Lidocaine (patch) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Transdermal patch
- LIDODERM may not stick if it gets wet. Avoid contact with water, such as bathing, swimming or showering.
Monitoring
There is limited information regarding Lidocaine (patch) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Lidocaine (patch) and IV administrations.
Overdosage
- Lidocaine overdose from cutaneous absorption is rare, but could occur. If there is any suspicion of lidocaine overdose , drug blood concentration should be checked. The management of overdose includes close monitoring, supportive care, and symptomatic treatment. Dialysis is of negligible value in the treatment of acute overdose with lidocaine.
- In the absence of massive topical overdose or oral ingestion, evaluation of symptoms of toxicity should include consideration of other etiologies for the clinical effects, or overdosage from other sources of lidocaine or other local anesthetics.
- The oral LD50 of lidocaine HCl is 459 (346-773) mg/kg (as the salt) in non-fasted female rats and 214 (159-324) mg/kg (as the salt) in fasted female rats, which are equivalent to roughly 4000 mg and 2000 mg, respectively, in a 60 to 70 kg man based on the equivalent surface area dosage conversion factors between species.
Pharmacology
Mechanism of Action
There is limited information regarding Lidocaine (patch) Mechanism of Action in the drug label.
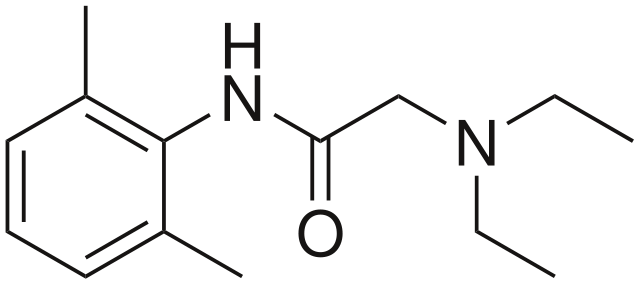
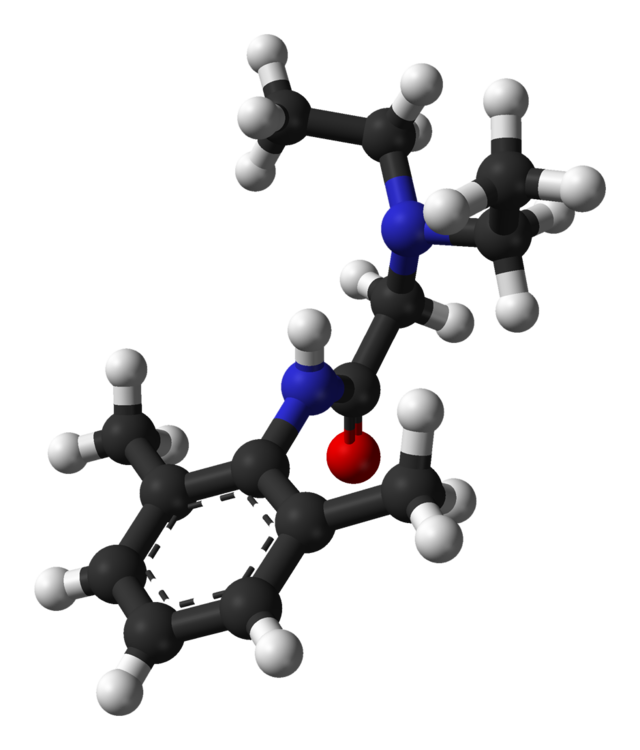
Structure
- LIDODERM (lidocaine patch 5%) is comprised of an adhesive material containing 5% lidocaine, which is applied to a non-woven polyester felt backing and covered with a polyethylene terephthalate (PET) film release liner. The release liner is removed prior to application to the skin. The size of the patch is 10 cm × 14 cm.
- Lidocaine is chemically designated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl), has an octanol: water partition ratio of 43 at pH 7.4, and has the following structure:

- Each adhesive patch contains 700 mg of lidocaine (50 mg per gram adhesive) in an aqueous base. It also contains the following inactive ingredients: dihydroxyaluminum aminoacetate, disodium edetate, gelatin, glycerin, kaolin, methylparaben, polyacrylic acid, polyvinyl alcohol, propylene glycol, propylparaben, sodium carboxymethylcellulose, sodium polyacrylate, D-sorbitol, tartaric acid, and urea.
Pharmacodynamics
- Lidocaine is an amide-type local anesthetic agent and is suggested to stabilize neuronal membranes by inhibiting the ionic fluxes required for the initiation and conduction of impulses.
- The penetration of lidocaine into intact skin after application of LIDODERM is sufficient to produce an analgesic effect, but less than the amount necessary to produce a complete sensory block.
Pharmacokinetics
Absorption
- The amount of lidocaine systemically absorbed from LIDODERM is directly related to both the duration of application and the surface area over which it is applied. In a pharmacokinetic study, three LIDODERM patches were applied over an area of 420 cm2 of intact skin on the back of normal volunteers for 12 hours. Blood samples were withdrawn for determination of lidocaine concentration during the application and for 12 hours after removal of patches. The results are summarized in Table 1.

- When LIDODERM is used according to the recommended dosing instructions, only 3 ± 2% of the dose applied is expected to be absorbed. At least 95% (665 mg) of lidocaine will remain in a used patch. Mean peak blood concentration of lidocaine is about 0.13 µg/mL (about 1/10 of the therapeutic concentration required to treat cardiac arrhythmias). Repeated application of three patches simultaneously for 12 hours (recommended maximum daily dose), once per day for three days, indicated that the lidocaine concentration does not increase with daily use. The mean plasma pharmacokinetic profile for the 15 healthy volunteers is shown in Figure 1.
- Figure 1
Mean lidocaine blood concentrations after three consecutive daily applications of three LIDODERM patches simultaneously for 12 hours per day in healthy volunteers (n = 15).

Distribution
- When lidocaine is administered intravenously to healthy volunteers, the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 ± 0.6 SD, n = 15). At concentrations produced by application of LIDODERM, lidocaine is approximately 70% bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much higher plasma concentrations (1 to 4 µg/mL of free base), the plasma protein binding of lidocaine is concentration dependent. Lidocaine crosses the placental and blood brain barriers, presumably by passive diffusion.
Metabolism
- It is not known if lidocaine is metabolized in the skin. Lidocaine is metabolized rapidly by the liver to a number of metabolites, including monoethylglycinexylidide (MEGX) and glycinexylidide (GX), both of which have pharmacologic activity similar to, but less potent than that of lidocaine. A minor metabolite, 2,6-xylidine, has unknown pharmacologic activity but is carcinogenic in rats. The blood concentration of this metabolite is negligible following application of LIDODERM (lidocaine patch 5%). Following intravenous administration, MEGX and GX concentrations in serum range from 11 to 36% and from 5 to 11% of lidocaine concentrations, respectively.
Excretion
- Lidocaine and its metabolites are excreted by the kidneys. Less than 10% of lidocaine is excreted unchanged. The half-life of lidocaine elimination from the plasma following IV administration is 81 to 149 minutes (mean 107 ± 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min (mean 0.64 ± 0.18 SD, n = 15).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- A minor metabolite, 2,6-xylidine, has been found to be carcinogenic in rats. The blood concentration of this metabolite is negligible following application of LIDODERM.
Mutagenesis
- Lidocaine HCl is not mutagenic in Salmonella/mammalian microsome test nor clastogenic in chromosome aberration assay with human lymphocytes and mouse micronucleus test.
Impairment of Fertility
- The effect of LIDODERM on fertility has not been studied.
Clinical Studies
- Single-dose treatment with LIDODERM was compared to treatment with vehicle patch (without lidocaine), and to no treatment (observation only) in a double-blind, crossover clinical trial with 35 post-herpetic neuralgia patients. Pain intensity and pain relief scores were evaluated periodically for 12 hours. LIDODERM performed statistically better than vehicle patch in terms of pain intensity from 4 to 12 hours.
- Multiple-dose, two-week treatment with LIDODERM was compared to vehicle patch (without lidocaine) in a double-blind, crossover clinical trial of withdrawal-type design conducted in 32 patients, who were considered as responders to the open-label use of LIDODERM prior to the study. The constant type of pain was evaluated but not the pain induced by sensory stimuli (dysesthesia). Statistically significant differences favoring LIDODERM were observed in terms of time to exit from the trial (14 versus 3.8 days at p-value <0.001), daily average pain relief, and patient's preference of treatment. About half of the patients also took oral medication commonly used in the treatment of post-herpetic neuralgia. The extent of use of concomitant medication was similar in the two treatment groups.
How Supplied
- LIDODERM (lidocaine patch 5%) is available as the following:
- Carton of 30 patches, packaged into individual child-resistant envelopes
NDC 63481-687-06
Storage
- Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F).
Images
Drug Images
{{#ask: Page Name::Lidocaine (patch) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel



{{#ask: Label Page::Lidocaine (patch) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Lidocaine (patch) Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Lidocaine (patch) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- LIDODERM®[1]
Look-Alike Drug Names
There is limited information regarding Lidocaine (patch) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.