Esophageal candidiasis pathophysiology
|
Esophageal candidiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Esophageal candidiasis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Esophageal candidiasis pathophysiology |
|
Risk calculators and risk factors for Esophageal candidiasis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Candida is a normal commensal of the skin and mucous membranes. The balance between the virulence of the fungus and the host immune defense is responsible avoiding opportunistic infection of candida. Deficiency of cell-mediated immunity or poor general status are the main risk factors for having opportunistic candidiasis. Candidiasis is usually localized to skin and mucous membranes. In rare cases, candidiasis can spread causing candidemia and distant infection. These cases are usually associated with deficient immunity . C. albicans is the main species causing infection in humans more than any other candida species.
Pathophysiology
Pathogenesis
Candida is a normal commensal of skin and mucous membranes. A competent immune system and an intact regenerating healthy mucosa oppose the virulence of Candida.
Candida Virulence factors
The main virulence factors that mediate the infection:[1]
- Secreting molecules that mediate adherence into host cells
- Production of hydrolases which has a lytic effect on tissues and facilitate the invasion by the fungus.
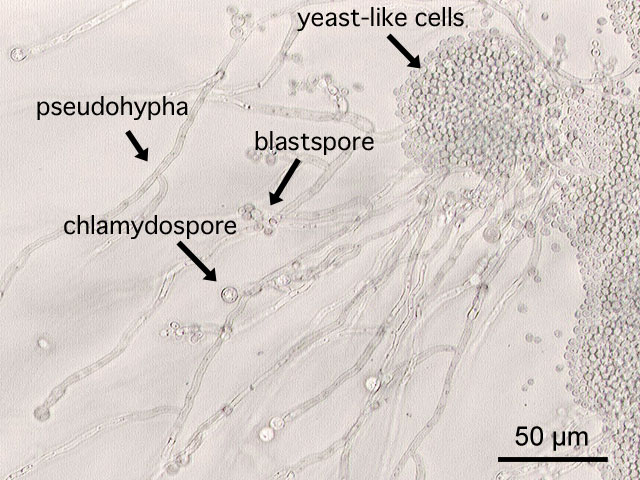
- Polymorphism: Candida has the ability to grow either as pseudohyphae (elongated ellipsoid form) or in a yeast form (rounded to oval budding form. While the role of polymorphism is not clearly understood in the virulence of Candida, it’s noted that the species that are capable of producing the most severe form of the disease has this ability.
- Biofilm production: which means the ability to form a thick layer of the organism on the mucosal surfaces or even on catheters and dentures.
Any condition that compromises cell-mediated immunity, worsens the general status of the patient or provide a favorable medium for Candida to form biofilms put the patient at increased risk for having candidiasis.[2]
Candidal gene VPS4 plays an important role in mucosal candidiasis specifically. Moreover, fungi with mutations affecting this gene were found to be less virulent.[3][4]
Gross Pathology
By upper endoscopy, candida esophagitis appears as white patches on the esophageal mucosa.
{{#ev:youtube|PKK-V07AXv8}}
Microscopic pathology:
 |
`
- Microscopic examination of the wet mount with 10% KOH or saline demonstrates hyphae, pseudohyphae, and blastospores.
References
- ↑ Mayer FL, Wilson D, Hube B (2013). "Candida albicans pathogenicity mechanisms". Virulence. 4 (2): 119–28. doi:10.4161/viru.22913. PMC 3654610. PMID 23302789.
- ↑ Pappas PG (2006). "Invasive candidiasis". Infect. Dis. Clin. North Am. 20 (3): 485–506. doi:10.1016/j.idc.2006.07.004. PMID 16984866.
- ↑ Rane HS, Hardison S, Botelho C, Bernardo SM, Wormley F, Lee SA (2014). "Candida albicans VPS4 contributes differentially to epithelial and mucosal pathogenesis". Virulence. 5 (8): 810–8. doi:10.4161/21505594.2014.956648. PMID 25483774.
- ↑ Lee SA, Jones J, Hardison S, Kot J, Khalique Z, Bernardo SM, Lazzell A, Monteagudo C, Lopez-Ribot J (2009). "Candida albicans VPS4 is required for secretion of aspartyl proteases and in vivo virulence". Mycopathologia. 167 (2): 55–63. doi:10.1007/s11046-008-9155-7. PMID 18814053.