Cetuximab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Sree Teja Yelamanchili, MBBS [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: SERIOUS INFUSION REACTIONS and CARDIOPULMONARY ARREST
See full prescribing information for complete Boxed Warning.
* Serious infusion reactions, some fatal, occurred in approximately 3% of patients.
|
Overview
Cetuximab is a monoclonal antibody that is FDA approved for the treatment of squamous cell carcinoma of the head and neck (SCCHN), and K-Ras Mutation-negative,EGFR-expressing colorectal cancer. There is a Black Box Warning for this drug as shown here. Common adverse reactions include acneiform eruption, dry skin, pruritus, radiation dermatitis, rash, hypomagnesemia, weight decreasing, constipation, diarrhea, nausea, neutropenia, infectious disease, asthenia, headache, sensory neuropathy, dyspnea, fatigue, late effect of radiation and pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Head and neck cancer
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Cetuximab in adult patients.
Non–Guideline-Supported Use
Gastric cancer
Dosing information
Malignant neoplasm of cardio-esophageal junction of stomach
Dosing information
- 400 mg/m(2) IV (loading dose) then 250 mg/m(2) IV (maintenance dose) every week[2]
Non-small cell lung cancer
Dosing information
- Not applicable
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Cetuximab FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Cetuximab in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Cetuximab in pediatric patients.
Contraindications
- None.
Warnings
|
WARNING: SERIOUS INFUSION REACTIONS and CARDIOPULMONARY ARREST
See full prescribing information for complete Boxed Warning.
* Serious infusion reactions, some fatal, occurred in approximately 3% of patients.
|
Infusion Reactions
Serious infusion reactions, requiring medical intervention and immediate, permanent discontinuation of Cetuximab include:
- Rapid onset of airway obstruction (bronchospasm, stridor, hoarseness)
- Hypotension
- Shock
- Loss of consciousness
- Myocardial infarction, and/or
- Cardiac arrest.
- Severe (NCI CTC Grades 3 and 4) infusion reactions occurred in 2–5% of 1373 patients in Studies 1, 3, 5, and 6 receiving Cetuximab, with fatal outcome in 1 patient.
- Approximately 90% of severe infusion reactions occurred with the first infusion despite premedication with antihistamines.
- Monitor patients for 1 hour following Cetuximab infusions in a setting with resuscitation equipment and other agents necessary to treat anaphylaxis (eg, epinephrine, corticosteroids, intravenous antihistamines, bronchodilators, and oxygen). Monitor longer to confirm resolution of the event in patients requiring treatment for infusion reactions.
- Immediately and permanently discontinue Cetuximab in patients with serious infusion reactions.
Cardiopulmonary Arrest
- Cardiopulmonary arrest and/or sudden death occurred in 4 (2%) of 208 patients treated with radiation therapy and Cetuximab as compared to none of 212 patients treated with radiation therapy alone in Study 1. *Three patients with prior history of coronary artery disease died at home, with myocardial infarction as the presumed cause of death.
- One of these patients had arrhythmia and one had congestive heart failure.
- Death occurred 27, 32, and 43 days after the last dose of Cetuximab.
- One patient with no prior history of coronary artery disease died one day after the last dose of Cetuximab.
- In Study 2, fatal cardiac disorders and/or sudden death occurred in 7 (3%) of 219 patients treated with EU-approved cetuximab and platinum-based therapy with 5-FU as compared to 4 (2%) of 215 patients treated with chemotherapy alone.
- Five of these 7 patients in the chemotherapy plus cetuximab arm received concomitant cisplatin and 2 patients received concomitant carboplatin.
- All 4 patients in the chemotherapy-alone arm received cisplatin. Carefully consider use of Cetuximab in combination with radiation therapy or platinum-based therapy with 5-FU in head and neck cancer patients with a history of coronary artery disease, congestive heart failure, or arrhythmias in light of these risks.
- Closely monitor serum electrolytes, including serum magnesium, potassium, and calcium, during and after Cetuximab.
Pulmonary Toxicity
- Interstitial lung disease (ILD), including 1 fatality, occurred in 4 of 1570 (<0.5%) patients receiving Cetuximab in Studies 1, 3, and 6, as well as other studies, in colorectal cancer and head and neck cancer.
- Interrupt Cetuximab for acute onset or worsening of pulmonary symptoms.
- Permanently discontinue Cetuximab for confirmed ILD.
Dermatologic Toxicity
Dermatologic toxicities, including
- Acneiform rash,
- skin drying and fissuring,
- paronychial inflammation,
- Infectious sequelae (for example, S. aureus sepsis, abscess formation, cellulitis, blepharitis, conjunctivitis, keratitis/ulcerative keratitis with decreased visual acuity, cheilitis)
- Hypertrichosis occurred in patients receiving Cetuximab therapy.
- Acneiform rash occurred in 76–88% of 1373 patients receiving Cetuximab in Studies 1, 3, 5, and 6.
- Severe acneiform rash occurred in 1–17% of patients.
- Acneiform rash usually developed within the first two weeks of therapy and resolved in a majority of the patients after cessation of treatment, although in nearly half, the event continued beyond 28 days.
- Monitor patients receiving Cetuximab for dermatologic toxicities and infectious sequelae.
- Instruct patients to limit sun exposure during Cetuximab therapy.
Use of Cetuximab in Combination With Radiation and Cisplatin
- In a controlled study, 940 patients with locally advanced SCCHN were randomized 1:1 to receive either Cetuximab in combination with radiation therapy and cisplatin or radiation therapy and cisplatin alone.
- The addition of Cetuximab resulted in an increase in the incidence of Grade 3–4 mucositis, radiation recall syndrome, acneiform rash, cardiac events, and electrolyte disturbances compared to radiation and cisplatin alone.
- Adverse reactions with fatal outcome were reported in 20 patients (4.4%) in the Cetuximab combination arm and 14 patients (3.0%) in the control arm.
- Nine patients in the Cetuximab arm (2.0%) experienced myocardial ischemia compared to 4 patients (0.9%) in the control arm.
- The main efficacy outcome of the study was progression-free survival (PFS).
- The addition of Cetuximab to radiation and cisplatin did not improve PFS.
Hypomagnesemia and Electrolyte Abnormalities
- In patients evaluated during clinical trials, hypomagnesemia occurred in 55% of 365 patients receiving Cetuximab in Study 5 and two other clinical trials in colorectal cancer and head and neck cancer, respectively, and was severe (NCI CTC Grades 3 and 4) in 6–17%.
- In Study 2, where EU-approved cetuximab was administered in combination with platinum-based therapy, the addition of cetuximab to cisplatin and 5-FU resulted in an increased incidence of hypomagnesemia (14% vs. 6%) and of Grade 3–4 hypomagnesemia (7% vs. 2%) compared to cisplatin and 5-FU alone.
- In contrast, the incidences of hypomagnesemia were similar for those who received cetuximab, carboplatin, and 5-FU compared to carboplatin and 5-FU (4% vs. 4%).
- No patient experienced Grade 3–4 hypomagnesemia in either arm in the carboplatin subgroup.
- The onset of hypomagnesemia and accompanying electrolyte abnormalities occurred days to months after initiation of Cetuximab.
- Periodically monitor patients for hypomagnesemia, hypocalcemia, and hypokalemia, during and for at least 8 weeks following the completion of Cetuximab. Replete electrolytes as necessary.
K-Ras Testing in Metastatic or Advanced colorectal cancer Patients
- Determination of K-Ras mutational status in colorectal tumors using an FDA-approved test indicated for this use is necessary for selection of patients for treatment with Cetuximab.
- Cetuximab is indicated only for patients with EGFR-expressing K-Ras mutation-negative (wild-type) mCRC.
- Cetuximab is not an effective treatment for patients with colorectal cancer that harbor somatic mutations in codons 12 and 13 (exon 2).
- Studies 4 and 5, conducted in patients with colorectal cancer, demonstrated a benefit with Cetuximab treatment only in the subset of patients whose tumors were K-Ras mutation-negative (wild-type).
- Cetuximab is not effective for the treatment of K-Ras mutation-positive colorectal cancer as determined by an FDA-approved test for this use.
- Perform the assesment for K-Ras mutation status in colorectal cancer in laboratories with demonstrated proficiency in the specific technology being utilized.
- Improper assay performance can lead to unreliable test results.
Refer to an FDA-approved test’s package insert for instructions on the identification of patients eligible for the treatment of Cetuximab.
Epidermal Growth Factor Receptor (EGFR) Expression and Response
- Because expression of EGFR has been detected in nearly all SCCHN tumor specimens, patients enrolled in the head and neck cancer clinical studies were not required to have immunohistochemical evidence of EGFR tumor expression prior to study entry.
- Patients enrolled in the colorectal cancer clinical studies were required to have immunohistochemical evidence of EGFR tumor expression.
- Primary tumor or tumor from a metastatic site was tested with the DakoCytomation EGFR pharmDxTM test kit.
- Specimens were scored based on the percentage of cells expressing EGFR and intensity (barely/faint, weak-to-moderate, and strong).
- Response rate did not correlate with either the percentage of positive cells or the intensity of EGFR expression.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data below reflect exposure to Cetuximab in 1373 patients with SCCHN or colorectal cancer in randomized Phase 3 (Studies 1 and 5) or Phase 2 (Studies 3 and 6) trials treated at the recommended dose and schedule for medians of 7 to 14 weeks.
Infusion reactions:
- Infusion reactions, which included pyrexia, chills, rigors, dyspnea, bronchospasm, angioedema, urticaria, hypertension, and hypotension occurred in 15–21% of patients across studies. Grades 3 and 4 infusion reactions occurred in 2–5% of patients; infusion reactions were fatal in 1 patient.
Infections:
- The incidence of infection was variable across studies, ranging from 13–35%. Sepsis occurred in 1–4% of patients.
Renal:
- Renal failure occurred in 1% of patients with colorectal cancer.
Squamous Cell Carcinoma of the Head and Neck
Cetuximab in Combination with Radiation Therapy
- Table 2 contains selected adverse reactions in 420 patients receiving radiation therapy either alone or with Cetuximab for locally or regionally advanced SCCHN in Study 1. Cetuximab was administered at the recommended dose and schedule (400 mg/m2 initial dose, followed by 250 mg/m2 weekly). Patients received a median of 8 infusions (range 1–11).

- The incidence and severity of mucositis, stomatitis, and xerostomia were similar in both arms of the study.
Late Radiation Toxicity
- The overall incidence of late radiation toxicities (any grade) was higher in Cetuximab in combination with radiation therapy compared with radiation therapy alone. The following sites were affected: salivary glands (65% versus 56%), larynx (52% versus 36%), subcutaneous tissue (49% versus 45%), mucous membrane (48% versus 39%), esophagus (44% versus 35%), skin (42% versus 33%). The incidence of Grade 3 or 4 late radiation toxicities was similar between the radiation therapy alone and the Cetuximab plus radiation treatment groups.
Study 2: EU-Approved Cetuximab in Combination with Platinum-based Therapy with 5-fluorouracil
- Study 2 used EU-approved cetuximab. Since U.S.-licensed Cetuximab provides approximately 22% higher exposure relative to the EU-approved cetuximab, the data provided below may underestimate the incidence and severity of adverse reactions anticipated with Cetuximab for this indication. However, the tolerability of the recommended dose is supported by safety data from additional studies of Cetuximab .
Table 3 contains selected adverse reactions in 434 patients with recurrent locoregional disease or metastatic SCCHN receiving EU-approved cetuximab in combination with platinum-based therapy with 5-FU or platinum-based therapy with 5-FU alone in Study 2. Cetuximab was administered at 400 mg/m2 for the initial dose, followed by 250 mg/m2 weekly. Patients received a median of 17 infusions (range 1–89).

- For cardiac disorders, approximately 9% of subjects in both the EU-approved cetuximab plus chemotherapy and chemotherapy-only treatment arms in Study 2 experienced a cardiac event. The majority of these events occurred in patients who received cisplatin/5-FU, with or without cetuximab as follows: 11% and 12% in patients who received cisplatin/5-FU with or without cetuximab, respectively, and 6% or 4% in patients who received carboplatin/5-FU with or without cetuximab, respectively. In both arms, the incidence of cardiovascular events was higher in the cisplatin with 5-FU containing subgroup. Death attributed to cardiovascular event or sudden death was reported in 3% of the patients in the cetuximab plus platinum-based therapy with 5-FU arm and 2% in the platinum-based chemotherapy with 5-FU alone arm.
Colorectal Cancer
Study 4: EU-Approved Cetuximab in Combination with FOLFIRI
- Study 4 used EU-approved cetuximab. U.S.-licensed Cetuximab provides approximately 22% higher exposure to cetuximab relative to the EU-approved cetuximab. The data provided below for Study 4 is consistent in incidence and severity of adverse reactions with those seen for Cetuximab in this indication. The tolerability of the recommended dose is supported by safety data from additional studies of Cetuximab.
Table 4 contains selected adverse reactions in 667 patients with K-Ras mutation-negative (wild-type), EGFR-expressing, metastatic colorectal cancer receiving EU-approved cetuximab plus FOLFIRI or FOLFIRI alone in Study 4. Cetuximab was administered at the recommended dose and schedule (400 mg/m2 initial dose, followed by 250 mg/m2 weekly). Patients received a median of 26 infusions (range 1–224).

Cetuximab in Combination with irinotecan
- The most frequently reported adverse reactions in 354 patients treated with Cetuximab plus irinotecan in clinical trials were acneiform rash (88%), asthenia/malaise (73%), diarrhea (72%), and nausea (55%). The most common Grades 3–4 adverse reactions included diarrhea (22%), leukopenia (17%), asthenia/malaise (16%), and acneiform rash (14%).
Immunogenicity
- As with all therapeutic proteins, there is potential for immunogenicity. * Immunogenic responses to cetuximab were assessed using either a double antigen radiometric assay or an ELISA assay.
- Due to limitations in assay performance and sampling timing, the incidence of antibody development in patients receiving Cetuximab has not been adequately determined.
- Non-neutralizing anti-cetuximab antibodies were detected in 5% (49 of 1001) of evaluable patients without apparent effect on the safety or antitumor activity of Cetuximab.
- The incidence of antibody formation is highly dependent on the sensitivity and specificity of the assay.
- Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
- For these reasons, comparison of the incidence of antibodies to Cetuximab with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
- The following adverse reactions have been identified during post-approval use of Cetuximab. Because these reactions are reported from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Aseptic meningitis
- Mucosal inflammation
Drug Interactions
- A drug interaction study was performed in which Cetuximab was administered in combination with irinotecan. There was no evidence of any pharmacokinetic interactions between Cetuximab and irinotecan.
Use in Specific Populations
Pregnancy
- There are no adequate and well-controlled studies of Cetuximab in pregnant women. Based on animal models, EGFR has been implicated in the control of prenatal development and may be essential for normal organogenesis, proliferation, and differentiation in the developing embryo. Human IgG is known to cross the placental barrier; therefore, Cetuximab may be transmitted from the mother to the developing fetus, and has the potential to cause fetal harm when administered to pregnant women. Cetuximab should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Pregnant cynomolgus monkeys were treated weekly with 0.4 to 4 times the recommended human dose of cetuximab (based on body surface area) during the period of organogenesis (gestation day [GD] 20–48). Cetuximab was detected in the amniotic fluid and in the serum of embryos from treated dams at GD 49. No fetal malformations or other teratogenic effects occurred in offspring. However, significant increases in embryolethality and abortions occurred at doses of approximately 1.6 to 4 times the recommended human dose of cetuximab (based on total body surface area).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cetuximab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cetuximab during labor and delivery.
Nursing Mothers
- It is not known whether Cetuximab is secreted in human milk. IgG antibodies, such as Cetuximab, can be excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Cetuximab, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. If nursing is interrupted, based on the mean half-life of cetuximab, nursing should not be resumed earlier than 60 days following the last dose of Cetuximab.
Pediatric Use
- The safety and effectiveness of Cetuximab in pediatric patients have not been established. The pharmacokinetics of cetuximab, in combination with irinotecan, were evaluated in pediatric patients with refractory solid tumors in an open-label, single-arm, dose-finding study. Cetuximab was administered once-weekly, at doses up to 250 mg/m2, to 27 patients ranging from 1 to 12 years old; and in 19 patients ranging from 13 to 18 years old. No new safety signals were identified in pediatric patients. The pharmacokinetic profiles of cetuximab between the two age groups were similar at the 75 and 150 mg/m2 single dose levels. The volume of the distribution appeared to be independent of dose and approximated the vascular space of 2–3 L/m2. Following a single dose of 250 mg/m2, the geometric mean AUC0-inf (CV%) value was 17.7 mg•h/mL (34%) in the younger age group (1–12 years, n=9) and 13.4 mg•h/mL (38%) in the adolescent group (13–18 years, n=6). The mean half-life of cetuximab was 110 hours (range 69 to 188 hours) for the younger age group, and 82 hours (range 55 to 117 hours) for the adolescent age group.
Geriatic Use
- Of the 1662 patients who received Cetuximab with irinotecan, FOLFIRI or Cetuximab monotherapy in six studies of advanced colorectal cancer, 588 patients were 65 years of age or older. No overall differences in safety or efficacy were observed between these patients and younger patients.
- Clinical studies of Cetuximab conducted in patients with head and neck cancer did not include sufficient number of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Gender
There is no FDA guidance on the use of Cetuximab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Cetuximab with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Cetuximab in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Cetuximab in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Cetuximab in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Cetuximab in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous infusion
Monitoring
- FDA Package Insert for Cetuximab contains no information regarding Adverse Reactions.
IV Compatibility
- There is limited information about the IV Compatibility.
Overdosage
- The maximum single dose of Cetuximab administered is 1000 mg/m2 in one patient. No adverse events were reported for this patient.
Pharmacology
| |
Cetuximab?
| |
| Therapeutic monoclonal antibody | |
| Source | xi/o |
| Target | EGF receptor |
| Identifiers | |
| CAS number | |
| ATC code | L01 |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 145781.6 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | 114 hrs |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
, |
| Pregnancy cat. |
? |
| Legal status |
Prescription Only (S4)(AU) ?(CA) POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | intravenous |
Mechanism of Action
- The epidermal growth factor receptor (EGFR, HER1, c-ErbB-1) is a transmembrane glycoprotein that is a member of a subfamily of type I receptor tyrosine kinases including EGFR, HER2, HER3, and HER4.
- The EGFR is constitutively expressed in many normal epithelial tissues, including the skin and hair follicle. Expression of EGFR is also detected in many human cancers including those of the head and neck, colon, and rectum.
- Cetuximab binds specifically to the EGFR on both normal and tumor cells, and competitively inhibits the binding of epidermal growth factor (EGF) and other ligands, such as transforming growth factor-alpha.
- In vitro assays and in vivo animal studies have shown that binding of cetuximab to the EGFR blocks phosphorylation and activation of receptor-associated kinases, resulting in inhibition of cell growth, induction of apoptosis, and decreased matrix metalloproteinase and vascular endothelial growth factor production.
- Signal transduction through the EGFR results in activation of wild-type K-Ras protein. However, in cells with activating K-Ras somatic mutations, the mutant K-Ras protein is continuously active and appears independent of EGFR regulation.
- In vitro, cetuximab can mediate antibody-dependent cellular cytotoxicity (ADCC) against certain human tumor types.
- In vitro assays and in vivo animal studies have shown that cetuximab inhibits the growth and survival of tumor cells that express the EGFR.
- No anti-tumor effects of cetuximab were observed in human tumor xenografts lacking EGFR expression.
- The addition of cetuximab to radiation therapy or irinotecan in human tumor xenograft models in mice resulted in an increase in anti-tumor effects compared to radiation therapy or chemotherapy alone.
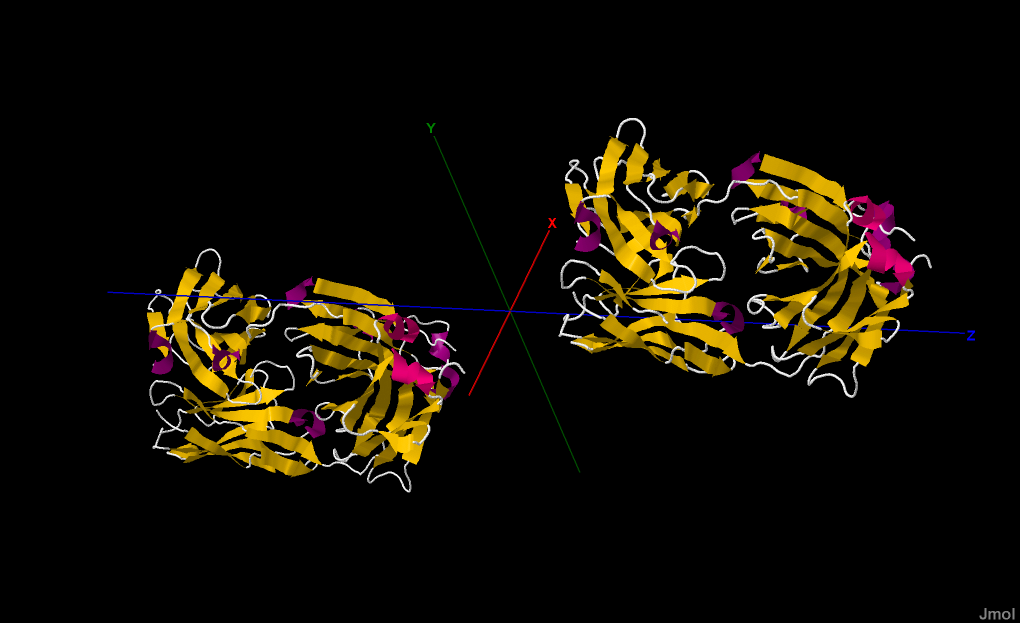
Structure
Cetuximab® (cetuximab) is a recombinant, human/mouse chimeric monoclonal antibody that binds specifically to the extracellular domain of the human epidermal growth factor receptor (EGFR). Cetuximab is composed of the Fv regions of a murine anti-EGFR antibody with human IgG1 heavy and kappa light chain constant regions and has an approximate molecular weight of 152 kDa. Cetuximab is produced in mammalian (murine myeloma) cell culture. Cetuximab is a sterile, clear, colorless liquid of pH 7.0 to 7.4, which may contain a small amount of easily visible, white, amorphous cetuximab particulates. Cetuximab is supplied at a concentration of 2 mg/mL in either 100 mg (50 mL) or 200 mg (100 mL), single-use vials. Cetuximab is formulated in a solution with no preservatives, which contains 8.48 mg/mL sodium chloride, 1.88 mg/mL sodium phosphate dibasic heptahydrate, 0.41 mg/mL sodium phosphate monobasic monohydrate, and Water for Injection, USP.
Pharmacodynamics
Effects on Electrocardiogram (ECG)
The effect of cetuximab on QT interval was evaluated in an open-label, single-arm, monotherapy trial in 37 subjects with advanced malignancies who received an initial dose of 400 mg/m2, followed by weekly infusions of 250 mg/m2 for a total of 5 weeks. No large changes in the mean QT interval of >20 ms from baseline were detected in the trial based on the Fridericia correction method. A small increase in the mean QTc interval of <10 ms cannot be excluded because of the limitations in the trial design.
Pharmacokinetics
Cetuximab administered as monotherapy or in combination with concomitant chemotherapy or radiation therapy exhibits nonlinear pharmacokinetics. The area under the concentration time curve (AUC) increased in a greater than dose proportional manner while clearance of cetuximab decreased from 0.08 to 0.02 L/h/m2 as the dose increased from 20 to 200 mg/m2, and at doses >200 mg/m2, it appeared to plateau. The volume of the distribution for cetuximab appeared to be independent of dose and approximated the vascular space of 2–3 L/m2. Following the recommended dose regimen (400 mg/m2 initial dose; 250 mg/m2 weekly dose), concentrations of cetuximab reached steady-state levels by the third weekly infusion with mean peak and trough concentrations across studies ranging from 168 to 235 and 41 to 85 µg/mL, respectively. The mean half-life of cetuximab was approximately 112 hours (range 63–230 hours). The pharmacokinetics of cetuximab were similar in patients with SCCHN and those with colorectal cancer. Cetuximab had an approximately 22% (90% confidence interval; 6%, 38%) higher systemic exposure relative to the EU-approved cetuximab used in Studies 2 and 4 based on a population pharmacokinetic analysis.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to test cetuximab for carcinogenic potential, and no mutagenic or clastogenic potential of cetuximab was observed in the Salmonella-Escherichia coli (Ames) assay or in the in vivo rat micronucleus test. Menstrual cyclicity was impaired in female cynomolgus monkeys receiving weekly doses of 0.4 to 4 times the human dose of cetuximab (based on total body surface area). Cetuximab-treated animals exhibited increased incidences of irregular or absent cycles, as compared to control animals. These effects were initially noted beginning week 25 of cetuximab treatment and continued through the 6-week recovery period. In this same study, there were no effects of cetuximab treatment on measured male fertility parameters (ie, serum testosterone levels and analysis of sperm counts, viability, and motility) as compared to control male monkeys. It is not known if cetuximab can impair fertility in humans.
Animal Pharmacology and/or Toxicology
In cynomolgus monkeys, cetuximab, when administered at doses of approximately 0.4 to 4 times the weekly human exposure (based on total body surface area), resulted in dermatologic findings, including inflammation at the injection site and desquamation of the external integument. At the highest dose level, the epithelial mucosa of the nasal passage, esophagus, and tongue were similarly affected, and degenerative changes in the renal tubular epithelium occurred. Deaths due to sepsis were observed in 50% (5/10) of the animals at the highest dose level beginning after approximately 13 weeks of treatment.
Clinical Studies
Studies 2 and 4 were conducted outside the U.S. using an EU-approved cetuximab as the clinical trial material. Cetuximab provides approximately 22% higher exposure relative to the EU-approved cetuximab used in Studies 2 and 4; these pharmacokinetic data, together with the results of Studies 2, 4, and other clinical trial data establish the efficacy of Cetuximab at the recommended dose in SCCHN and mCRC [see Clinical Pharmacology (12.3)].
Squamous Cell Carcinoma of the Head and Neck (SCCHN)
Study 1 was a randomized, multicenter, controlled trial of 424 patients with locally or regionally advanced SCCHN. Patients with Stage III/IV SCCHN of the oropharynx, hypopharynx, or larynx with no prior therapy were randomized (1:1) to receive either Cetuximab plus radiation therapy or radiation therapy alone. Stratification factors were Karnofsky performance status (60–80 versus 90–100), nodal stage (N0 versus N+), tumor stage (T1–3 versus T4 using American Joint Committee on Cancer 1998 staging criteria), and radiation therapy fractionation (concomitant boost versus once-daily versus twice-daily). Radiation therapy was administered for 6–7 weeks as once-daily, twice-daily, or concomitant boost. Cetuximab was administered as a 400 mg/m2 initial dose beginning one week prior to initiation of radiation therapy, followed by 250 mg/m2 weekly administered 1 hour prior to radiation therapy for the duration of radiation therapy (6–7 weeks). Of the 424 randomized patients, the median age was 57 years, 80% were male, 83% were Caucasian, and 90% had baseline Karnofsky performance status ≥80. There were 258 patients enrolled in U.S. sites (61%). Sixty percent of patients had oropharyngeal, 25% laryngeal, and 15% hypopharyngeal primary tumors; 28% had AJCC T4 tumor stage. Fifty-six percent of the patients received radiation therapy with concomitant boost, 26% received once-daily regimen, and 18% twice-daily regimen. The main outcome measure of this trial was duration of locoregional control. Overall survival was also assessed. Results are presented in Table 6.

Study 2 was an open-label, randomized, multicenter, controlled trial of 442 patients with recurrent locoregional disease or metastatic SCCHN. Patients with no prior therapy for recurrent locoregional disease or metastatic SCCHN were randomized (1:1) to receive EU-approved cetuximab plus cisplatin or carboplatin and 5-FU, or cisplatin or carboplatin and 5-FU alone. Choice of cisplatin or carboplatin was at the discretion of the treating physician. Stratification factors were Karnofsky performance status (<80 versus ≥80) and previous chemotherapy. cisplatin (100 mg/m2, Day 1) or carboplatin (AUC 5, Day 1) plus intravenous 5-FU (1000 mg/m2/day, Days 1–4) were administered every 3 weeks (1 cycle) for a maximum of 6 cycles in the absence of disease progression or unacceptable toxicity. Cetuximab was administered at a 400 mg/m2 initial dose, followed by a 250 mg/m2 weekly dose in combination with chemotherapy. Patients demonstrating at least stable disease on cetuximab in combination with chemotherapy were to continue cetuximab monotherapy at 250 mg/m2 weekly, in the absence of disease progression or unacceptable toxicity after completion of 6 planned courses of platinum-based therapy. For patients where treatment was delayed because of the toxic effects of chemotherapy, weekly cetuximab was continued. If chemotherapy was discontinued for toxicity, cetuximab could be continued as monotherapy until disease progression or unacceptable toxicity. Of the 442 randomized patients, the median age was 57 years, 90% were male, 98% were Caucasian, and 88% had baseline Karnofsky performance status ≥80. Thirty-four percent of patients had oropharyngeal, 25% laryngeal, 20% oral cavity, and 14% hypopharyngeal primary tumors. Fifty-three percent of patients had recurrent locoregional disease only and 47% had metastatic disease. Fifty-eight percent had AJCC Stage IV disease and 21% had Stage III disease. Sixty-four percent of patients received cisplatin therapy and 34% received carboplatin as initial therapy. Approximately fifteen percent of the patients in the cisplatin alone arm switched to carboplatin during the treatment period. The main outcome measure of this trial was overall survival. Results are presented in Table 7 and Figure 1.

Figure 1: Kaplan-Meier Curve for Overall Survival in Patients with Recurrent Locoregional Disease or Metastatic Squamous Cell Carcinoma of the Head and Neck

In exploratory subgroup analyses of Study 2 by initial platinum therapy (cisplatin or carboplatin), for patients (N=284) receiving cetuximab plus cisplatin with 5-FU compared to cisplatin with 5-FU alone, the difference in median overall survival was 3.3 months (10.6 versus 7.3 months, respectively; HR 0.71; 95% CI 0.54, 0.93). The difference in median progression-free survival was 2.1 months (5.6 versus 3.5 months, respectively; HR 0.55; 95% CI 0.41, 0.73). The objective response rate was 39% and 23% respectively (OR 2.18; 95% CI 1.29, 3.69). For patients (N=149) receiving cetuximab plus carboplatin with 5-FU compared to carboplatin with 5-FU alone, the difference in median overall survival was 1.4 months (9.7 versus 8.3 months; HR 0.99; 95% CI 0.69, 1.43). The difference in median progression-free survival was 1.7 months (4.8 versus 3.1 months, respectively; HR 0.61; 95% CI 0.42, 0.89). The objective response rate was 30% and 15% respectively (OR 2.45; 95% CI 1.10, 5.46). Study 3 was a single-arm, multicenter clinical trial in 103 patients with recurrent or metastatic SCCHN. All patients had documented disease progression within 30 days of a platinum-based chemotherapy regimen. Patients received a 20-mg test dose of Cetuximab on Day 1, followed by a 400 mg/m2 initial dose, and 250 mg/m2 weekly until disease progression or unacceptable toxicity. The median age was 57 years, 82% were male, 100% Caucasian, and 62% had a Karnofsky performance status of ≥80. The objective response rate was 13% (95% confidence interval 7%–21%). Median duration of response was 5.8 months (range 1.2–5.8 months).
colorectal cancer
Cetuximab Clinical Trials in K-Ras Mutation-negative (Wild-type), EGFR-expressing, Metastatic colorectal cancer Study 4 was a randomized, open-label, multicenter, study of 1217 patients with EGFR-expressing metastatic colorectal cancer. Patients were randomized (1:1) to receive either EU-approved cetuximab in combination with FOLFIRI or FOLFIRI alone as first-line treatment. Stratification factors were Eastern Cooperative Oncology Group (ECOG) performance status (0 and 1 versus 2) and region (sites in Western Europe versus Eastern Europe versus other). FOLFIRI regimen included 14-day cycles of irinotecan (180 mg/m2 administered intravenously on Day 1), folinic acid (400 mg/m2 [racemic] or 200 mg/m2 [L-form] administered intravenously on Day 1), and 5-FU (400 mg/m2 bolus on Day 1 followed by 2400 mg/m2 as a 46-hour continuous infusion). Cetuximab was administered as a 400 mg/m2 initial dose on Day 1, Week 1, followed by 250 mg/m2 weekly administered 1 hour prior to chemotherapy. Study treatment continued until disease progression or unacceptable toxicity occurred. Of the 1217 randomized patients, the median age was 61 years, 60% were male, 86% were Caucasian, and 96% had a baseline ECOG performance status 0–1, 60% had primary tumor localized in colon, 84% had 1–2 metastatic sites and 20% had received prior adjuvant and/or neoadjuvant chemotherapy. Demographics and baseline characteristics were similar between study arms. K-Ras mutation status was available for 1079/1217 (89%) of the patients: 676 (63%) patients had K-Ras mutation-negative (wild-type) tumors and 403 (37%) patients had K-Ras mutation-positive tumors where testing assessed for the following somatic mutations in codons 12 and 13 (exon 2): G12A, G12D, G12R, G12C, G12S, G12V, G13D [see Warnings and Precautions (5.7)]. Baseline characteristics and demographics in the K-Ras mutation-negative (wild-type) subset were similar to that seen in the overall population [see Warnings and Precautions (5.7)]. The main outcome measure of this trial was progression-free survival assesed by an independent review committee (IRC). Overall survival and response rate were also assessed. A statistically significant improvement in PFS was observed for the cetuximab plus FOLFIRI arm compared with the FOLFIRI arm (median PFS 8.9 vs 8.1 months, HR 0.85 [95% CI 0.74, 0.99], p-value=0.036). Overall survival was not significantly different at the planned, final analysis based on 838 events [HR=0.93, 95% CI (0.8, 1.1), p-value 0.327]. Results of the planned PFS and ORR analysis in all randomized patients and post-hoc PFS and ORR analysis in subgroups of patients defined by K-Ras mutation status, and post-hoc analysis of updated OS based on additional follow-up (1000 events) in all randomized patients and in subgroups of patients defined by K-Ras mutation status are presented in Table 8 and Figure 2. The treatment effect in the all-randomized population for PFS was driven by treatment effects limited to patients who have K-Ras mutation-negative (wild-type) tumors. There is no evidence of effectiveness in the subgroup of patients with K-Ras mutation-positive tumors.

Figure 2: Kaplan-Meier Curve for Overall Survival in the K-Ras Mutation-negative (Wild-type) Population in Study 4

Study 5 was a multicenter, open-label, randomized, clinical trial conducted in 572 patients with EGFR-expressing, previously treated, recurrent mCRC. Patients were randomized (1:1) to receive either Cetuximab plus best supportive care (BSC) or BSC alone. Cetuximab was administered as a 400 mg/m2 initial dose, followed by 250 mg/m2 weekly until disease progression or unacceptable toxicity. Of the 572 randomized patients, the median age was 63 years, 64% were male, 89% were Caucasian, and 77% had baseline ECOG performance status of 0–1. Demographics and baseline characteristics were similar between study arms. All patients were to have received and progressed on prior therapy including an irinotecan-containing regimen and an oxaliplatin-containing regimen. K-Ras status was available for 453/572 (79%) of the patients: 245 (54%) patients had K-Ras mutation-negative (wild-type) tumors and 208 (46%) patients had K-Ras mutation-positive tumors where testing assessed for the following somatic mutations in codons 12 and 13 (exon 2): G12A, G12D, G12R, G12C, G12S, G12V, G13D [see Warnings and Precautions (5.7)]. The main outcome measure of the study was overall survival. Results are presented in Table 9 and Figure 3.

Figure 3: Kaplan-Meier Curve for Overall Survival in Patients with K-Ras Mutation-negative (Wild-type) Metastatic colorectal cancer in Study 5

Study 6 was a multicenter, clinical trial conducted in 329 patients with EGFR-expressing recurrent mCRC. Tumor specimens were not available for testing for K-Ras mutation status. Patients were randomized (2:1) to receive either Cetuximab plus irinotecan (218 patients) or Cetuximab monotherapy (111 patients). Cetuximab was administered as a 400 mg/m2 initial dose, followed by 250 mg/m2 weekly until disease progression or unacceptable toxicity. In the Cetuximab plus irinotecan arm, irinotecan was added to Cetuximab using the same dose and schedule for irinotecan as the patient had previously failed. Acceptable irinotecan schedules were 350 mg/m2 every 3 weeks, 180 mg/m2 every 2 weeks, or 125 mg/m2 weekly times four doses every 6 weeks. Of the 329 patients, the median age was 59 years, 63% were male, 98% were Caucasian, and 88% had baseline Karnofsky performance status ≥80. Approximately two-thirds had previously failed oxaliplatin treatment. The efficacy of Cetuximab plus irinotecan or Cetuximab monotherapy, based on durable objective responses, was evaluated in all randomized patients and in two pre-specified subpopulations: irinotecan refractory patients, and irinotecan and oxaliplatin failures. In patients receiving Cetuximab plus irinotecan, the objective response rate was 23% (95% confidence interval 18%–29%), median duration of response was 5.7 months, and median time to progression was 4.1 months. In patients receiving Cetuximab monotherapy, the objective response rate was 11% (95% confidence interval 6%–18%), median duration of response was 4.2 months, and median time to progression was 1.5 months. Similar response rates were observed in the pre-defined subsets in both the combination arm and monotherapy arm of the study.
How Supplied
Cetuximab® (cetuximab) is supplied at a concentration of 2 mg/mL as a 100 mg/50 mL, single-use vial or as a 200 mg/100 mL, single-use vial as a sterile, injectable liquid containing no preservatives.
NDC 66733-948-23 100 mg/50 mL, single-use vial, individually packaged in a carton NDC 66733-958-23 200 mg/100 mL, single-use vial, individually packaged in a carton
Storage
Store vials under refrigeration at 2° C to 8° C (36° F to 46° F). Do not freeze. Increased particulate formation may occur at temperatures at or below 0° C. This product contains no preservatives. Preparations of Cetuximab in infusion containers are chemically and physically stable for up to 12 hours at 2° C to 8° C (36° F to 46° F) and up to 8 hours at controlled room temperature (20° C to 25° C; 68° F to 77° F). Discard any remaining solution in the infusion container after 8 hours at controlled room temperature or after 12 hours at 2° C to 8° C. Discard any unused portion of the vial.
Images
Drug Images
{{#ask: Page Name::Cetuximab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Cetuximab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise patients:
- To report signs and symptoms of infusion reactions such as fever, chills, or breathing problems.
- Of the potential risks of using Cetuximab during pregnancy or nursing and of the need to use adequate contraception in both males and females during and for 6 months following the last dose of Cetuximab therapy.
- That nursing is not recommended during, and for 2 months following the last dose of Cetuximab therapy.
- To limit sun exposure (use sunscreen, wear hats) while receiving and for 2 months following the last dose of Cetuximab.
Precautions with Alcohol
Alcohol-Cetuximab interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Erbitux
Look-Alike Drug Names
cetuximab - rituximab[4]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 Kim C, Lee JL, Ryu MH, Chang HM, Kim TW, Lim HY; et al. (2011). "A prospective phase II study of cetuximab in combination with XELOX (capecitabine and oxaliplatin) in patients with metastatic and/or recurrent advanced gastric cancer". Invest New Drugs. 29 (2): 366–73. doi:10.1007/s10637-009-9363-0. PMID 19997960.
- ↑ 2.0 2.1 Moehler M, Mueller A, Trarbach T, Lordick F, Seufferlein T, Kubicka S; et al. (2011). "Cetuximab with irinotecan, folinic acid and 5-fluorouracil as first-line treatment in advanced gastroesophageal cancer: a prospective multi-center biomarker-oriented phase II study". Ann Oncol. 22 (6): 1358–66. doi:10.1093/annonc/mdq591. PMID 21119032.
- ↑ Lordick F, Luber B, Lorenzen S, Hegewisch-Becker S, Folprecht G, Wöll E; et al. (2010). "Cetuximab plus oxaliplatin/leucovorin/5-fluorouracil in first-line metastatic gastric cancer: a phase II study of the Arbeitsgemeinschaft Internistische Onkologie (AIO)". Br J Cancer. 102 (3): 500–5. doi:10.1038/sj.bjc.6605521. PMC 2822949. PMID 20068568.
- ↑ "https://www.ismp.org". External link in
|title=(help)