Cryptosporidiosis pathophysiology
Jump to navigation
Jump to search
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Kalsang Dolma, M.B.B.S.[2]
|
Cryptosporidiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cryptosporidiosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cryptosporidiosis pathophysiology |
|
Risk calculators and risk factors for Cryptosporidiosis pathophysiology |
Overview
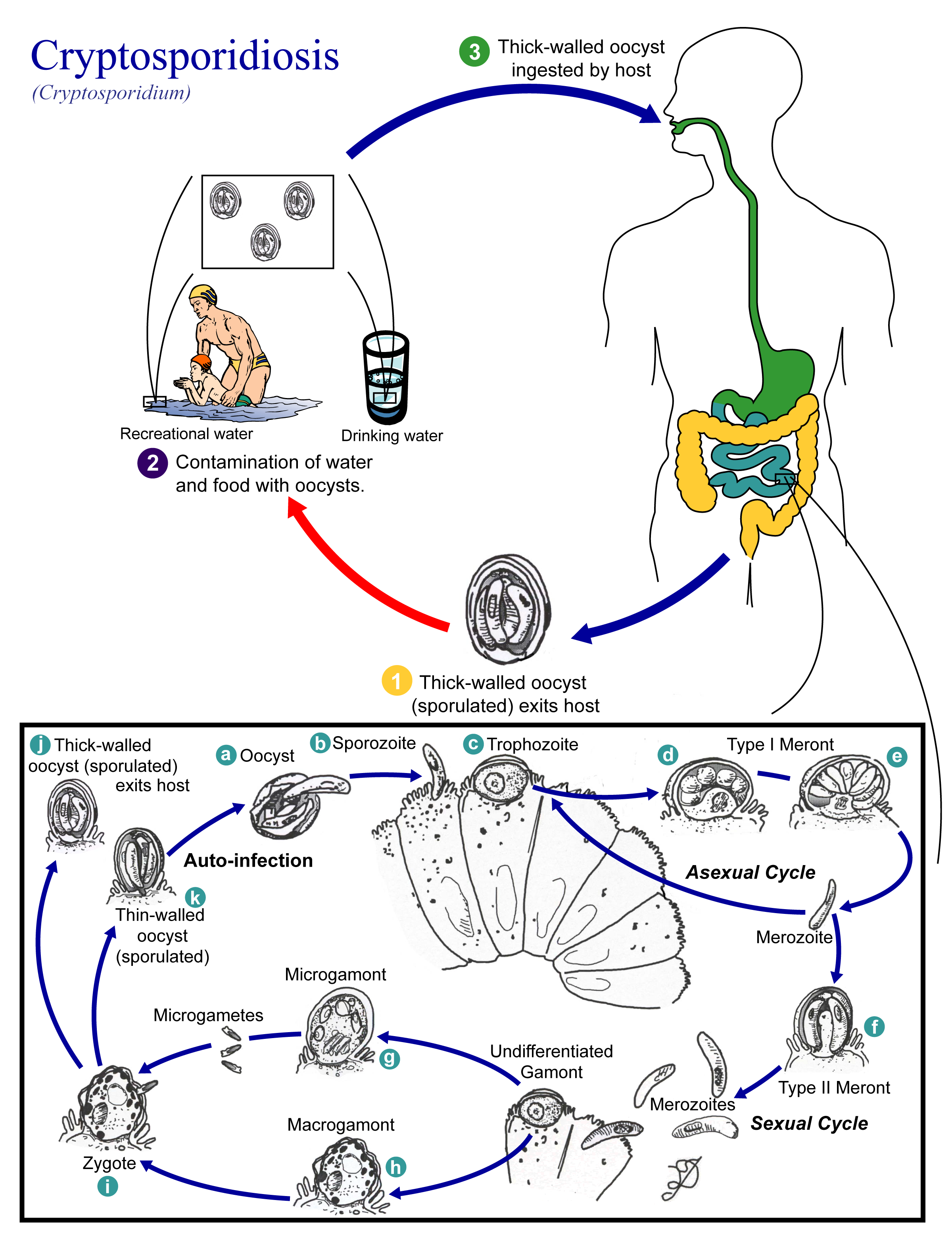
Cryptosporidiosis is a zoonotic disease, humans could be infected by contact with contaminated water and through inhalation of the spores. Following transmission, white blood cells phagocyte the pathogen and transports it via hematologic or lymphatic route to different organs.[1][2]
Pathophysiology
The pathophysiology of cryptosporidiosis can be described in the following steps
Transmission
- Transmission of Cryptosporidium parvum and C. hominis occurs mainly through contact with contaminated water (e.g., drinking or recreational water).
- Occasionally food sources, such as chicken salad, may serve as vehicles for transmission.
- Many outbreaks in the United States have occurred in waterparks, community swimming pools, and day care centers.
- Zoonotic and anthroponotic transmission of C. parvum and anthroponotic transmission of C. hominis occur through exposure to infected animals or exposure to water contaminated by feces of infected animals.
Incubation
- Incubation period for cryptosporidiosis is of 7 days (but can vary from 2 to 10 days).
Dissemination
- Following ingestion (and possibly inhalation) by a suitable host, excystation occurs.
- The sporozoites are released and parasitize epithelial cells of the gastrointestinal tract or other tissues such as the respiratory tract.
Pathogenesis
- In these cells, the parasites undergo asexual multiplication (schizogony or merogony) and then sexual multiplication (gametogony) producing microgamonts (male) and macrogamonts (female).
- Upon fertilization of the macrogamonts by the microgametes, oocysts develop that sporulate in the infected host.
- Two different types of oocysts are produced, the thick-walled, which is commonly excreted from the host, and the thin-walled oocyst, which is primarily involved in autoinfection.
- Oocysts are infective upon excretion, thus permitting direct and immediate fecal-oral transmission.
- Oocysts of Cyclospora cayetanensis, another important coccidian parasite, are unsporulated at the time of excretion and do not become infective until sporulation is completed.
Gallery
-
Life cycle of different species of Cryptosporidium, the causal agents of Cryptosporidiosis. From Public Health Image Library (PHIL). [3]
References
- ↑ "General Information | Cryptosporidium | Parasites | CDC".
- ↑ Leitch GJ, He Q (2012). "Cryptosporidiosis-an overview". J Biomed Res. 25 (1): 1–16. doi:10.1016/S1674-8301(11)60001-8. PMC 3368497. PMID 22685452.
- ↑ "Public Health Image Library (PHIL)".
![Life cycle of different species of Cryptosporidium, the causal agents of Cryptosporidiosis. From Public Health Image Library (PHIL). [3]](/images/c/cd/Cryptosporidiosis07.jpeg)