Azithromycin clinical pharmacology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Clinical Pharmacology
Pharmacokinetics
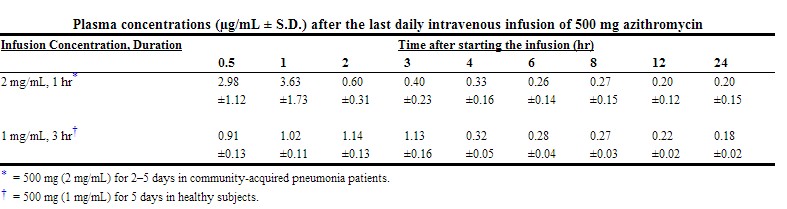
In patients hospitalized with community-acquired pneumonia receiving single daily one-hour intravenous infusions for 2 to 5 days of 500 mg azithromycin at a concentration of 2 mg/mL, the mean Cmax ± S.D. achieved was 3.63 ± 1.6 mcg/mL, while the 24-hour trough level was 0.2 ± 0.15 mcg/mL, and the AUC24 was 9.6 ± 4.8 mcg•h/mL.
The mean Cmax, 24-hour trough and AUC24 values were 1.14 ± 0.14 mcg/mL, 0.18 ± 0.02 mcg/mL, and 8.03 ± 0.86 mcg•h/mL, respectively, in normal volunteers receiving a 3-hour intravenous infusion of 500 mg azithromycin at a concentration of 1 mg/mL. Similar pharmacokinetic values were obtained in patients hospitalized with community-acquired pneumonia who received the same 3-hour dosage regimen for 2 to 5 days.
 |
The average CLt and Vd values were 10.18 mL/min/kg and 33.3 L/kg, respectively, in 18 normal volunteers receiving 1000 to 4000-mg doses given as 1 mg/mL over 2 hours.
Comparison of the plasma pharmacokinetic parameters following the 1st and 5th daily doses of 500 mg intravenous azithromycin showed only an 8% increase in Cmax but a 61% increase in AUC24 reflecting a threefold rise in C24 trough levels.
Following single oral doses of 500-mg azithromycin (two 250-mg capsules) to 12 healthy volunteers, Cmax, trough level, and AUC24 were reported to be 0.41 µg/mL, 0.05 µg/mL, and 2.6 µg∙h/mL, respectively. These oral values are approximately 38%, 83%, and 52% of the values observed following a single 500-mg I.V. 3-hour infusion (Cmax: 1.08 µg/mL, trough: 0.06 µg/mL, and AUC24: 5.0 µg∙h/mL). Thus, plasma concentrations are higher following the intravenous regimen throughout the 24-hour interval. The pharmacokinetic parameters on day 5 of azithromycin 250-mg capsules following a 500-mg oral loading dose to healthy young adults (age 18–40 years old) were as follows: Cmax: 0.24 µg/mL, AUC24: 2.1 µg∙h/mL. Azithromycin 250-mg capsules are no longer commercially available. Azithromycin 250-mg tablets are bioequivalent to 250-mg capsules in the fasting state.
Median azithromycin exposure (AUC0–288) in mononuclear (MN) and polymorphonuclear (PMN) leukocytes following 1,500 mg of oral azithromycin, administered in single daily doses over either 5 days (two 250-mg tablets on day 1, followed by one 250-mg tablet on days 2–5) or 3 days (500 mg per day for days 1–3) to 12 healthy volunteers, was more than a 1000-fold and 800-fold greater than in serum, respectively.
Distribution
The serum protein binding of azithromycin is variable in the concentration range approximating human exposure, decreasing from 51% at 0.02 µg/mL to 7% at 2 µg/mL.
Tissue concentrations have not been obtained following intravenous infusions of azithromycin. Selected tissue (or fluid) concentration and tissue (or fluid) to plasma/serum concentration ratios following oral administration of azithromycin are shown in the following table:
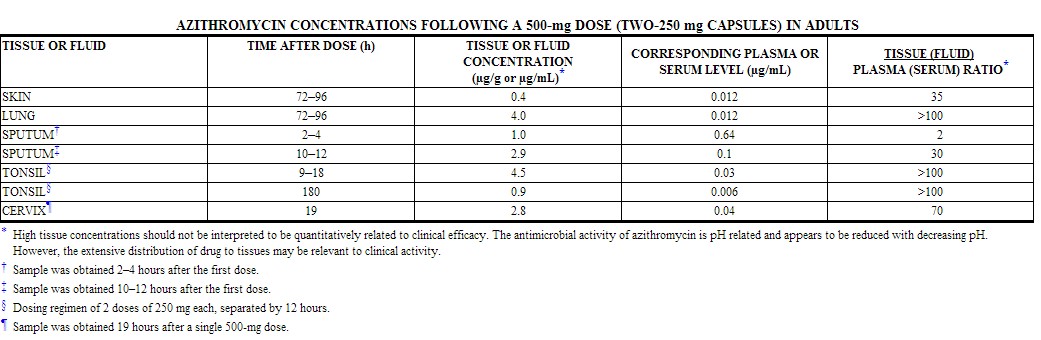 |
Tissue levels were determined following a single oral dose of 500-mg azithromycin in 7 gynecological patients. Approximately 17 hours after dosing, azithromycin concentrations were 2.7 µg/g in ovarian tissue, 3.5 µg/g in uterine tissue, and 3.3 µg/g in salpinx. Following a regimen of 500 mg on the first day followed by 250 mg daily for 4 days, concentrations in the cerebrospinal fluid were less than 0.01 µg/mL in the presence of non-inflamed meninges.
Metabolism
In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed.
Elimination
Plasma concentrations of azithromycin following single 500-mg oral and i.v. doses declined in a polyphasic pattern with a mean apparent plasma clearance of 630 mL/min and terminal elimination half-life of 68 hours. The prolonged terminal half-life is thought to be due to extensive uptake and subsequent release of drug from tissues.
In a multiple-dose study in 12 normal volunteers utilizing a 500-mg (1 mg/mL) one-hour intravenous-dosage regimen for five days, the amount of administered azithromycin dose excreted in urine in 24 hours was about 11% after the 1st dose and 14% after the 5th dose. These values are greater than the reported 6% excreted unchanged in urine after oral administration of azithromycin. Biliary excretion is a major route of elimination for unchanged drug, following oral administration.
Special Populations
Renal Insufficiency
Azithromycin pharmacokinetics were investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1,000-mg dose of azithromycin, mean Cmax and AUC0–120 increased by 5.1% and 4.2%, respectively in subjects with mild to moderate renal impairment (GFR 10 to 80 mL/min) compared to subjects with normal renal function (GFR >80 mL/min). The mean Cmax and AUC0–120 increased 61% and 35%, respectively in subjects with severe renal impairment (GFR <10 mL/min) compared to subjects with normal renal function (GFR >80 mL/min). (See DOSAGE AND ADMINISTRATION.)
Hepatic Insufficiency
The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established.
Gender
There are no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment is recommended based on gender.
Geriatric Patients
Pharmacokinetic studies with intravenous azithromycin have not been performed in older volunteers. Pharmacokinetics of azithromycin following oral administration in older volunteers (65–85 years old) were similar to those in younger volunteers (18–40 years old) for the 5-day therapeutic regimen.
Pediatric Patients
Pharmacokinetic studies with intravenous azithromycin have not been performed in children.
Drug-Drug Interactions
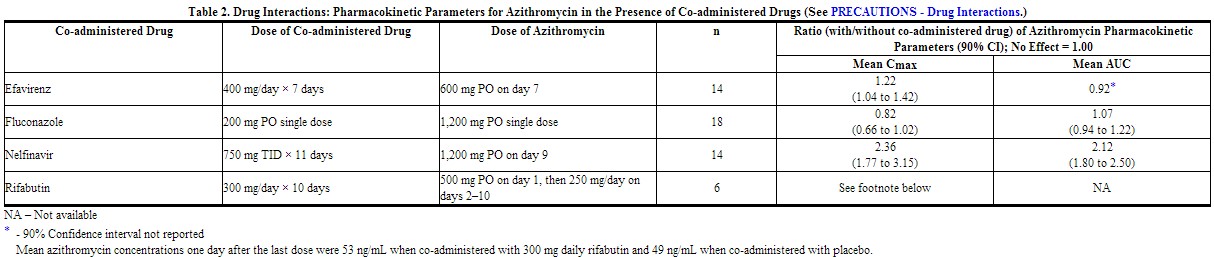
Drug interaction studies were performed with oral azithromycin and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 2.
Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is recommended when co-administered with azithromycin.
Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the pharmacokinetics of azithromycin. Nelfinavir significantly increased the Cmax and AUC of azithromycin. No dosage adjustment of azithromycin is recommended when administered with drugs listed in Table 2. (See PRECAUTIONS - Drug Interactions.)
 |
NA - Not Available
- - 90% Confidence interval not reported
Mean rifabutin concentrations one-half day after the last dose of rifabutin were 60 ng/mL when co-administered with azithromycin and 71 ng/mL when co-administered with placebo.
 |
Pharmacodynamics
Cardiac Electrophysiology
QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116 healthy subjects who received either chloroquine (1000 mg) alone or in combination with azithromycin (500 mg, 1000 mg, and 1500 mg once daily). Co-administration of azithromycin increased the QTc interval in a dose- and concentration-dependent manner. In comparison to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1000 mg and 1500 mg azithromycin, respectively.[1]
References
- ↑ "http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/050710s039,050711s036,050784s023lbl.pdf" (PDF). External link in
|title=(help)
Adapted from the FDA Package Insert.