Antihemophilic factor
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Sree Teja Yelamanchili, MBBS [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Antihemophilic factor is a human antihemophilic factor that is FDA approved for the treatment of hemophilia A. Common adverse reactions include nausea, headache, blurred vision.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hemophilia A
- Indication
- Antihemophilic factor is a recombinant antihemophilic factor indicated for:
- Control and prevention of bleeding episodes in adults and children with hemophilia A.
- Surgical prophylaxis in adults and children with hemophilia A.
- Routine prophylactic treatment to prevent or reduce the frequency of bleeding episodes in children with hemophilia A and to reduce the risk of joint damage in children without pre-existing joint damage.
- Routine prophylactic treatment to prevent or reduce the frequency of bleeding episodes in adults with hemophilia A.
- Antihemophilic factor is not indicated for the treatment of von Willebrand disease.
- Dosing Information
- Dosage and duration of treatment depend on the severity of the factor VIII deficiency, the location and extent of bleeding, and the patient's clinical condition.1 Careful control of replacement therapy is especially important in cases of major surgery or life-threatening bleeding episodes.
- Each vial of Antihemophilic factor has the recombinant factor VIII (rFVIII) potency in international units (IU, unit) stated on the label. One IU (unit), as defined by the World Health Organization standard for blood coagulation factor VIII, human, is approximately equal to the level of factor VIII activity found in 1 mL of fresh pooled human plasma.
- The expected in vivo peak increase in factor VIII level expressed as IU/dL (or % normal) can be estimated using the following formulas:
Dosage (units) = body weight (kg) × desired factor VIII rise (IU/dL or % of normal) × 0.5 (IU/kg per IU/dL) or IU/dL (or % normal) = Total Dose (IU)/body weight (kg) × 2 [IU/dL]/[IU/kg]
- Titrate dose to the patient's clinical response. Patients may vary in their pharmacokinetic (e.g., half-life, in vivo recovery) and clinical responses to Antihemophilic factor.2,3,4 Although the dose can be estimated by the calculations above, it is highly recommended that appropriate laboratory tests, including serial factor VIII activity assays, are performed.
- Control and Prevention of Bleeding Episodes
A guide for dosing Antihemophilic factor for the control and prevention of bleeding episodes is provided in Table 1. The goal of treatment is to maintain a plasma factor VIII activity level at or above the plasma levels (in % of normal or in IU/dL) outlined in Table 1.

- Peri-operative Management
A guide for dosing Antihemophilic factor during surgery (perioperative management) is provided in Table 2. The goal of treatment is to maintain a plasma factor VIII activity level at or above the plasma level (in % of normal or in IU/dL) outlined in Table 2.

- Routine Prophylaxis in Adults
- Recommended dosage: 25 units/kg body weight IV three times per week.
- Routine Prophylaxis in Children
- Recommended dosage: 25 IU/kg body IV weight qod
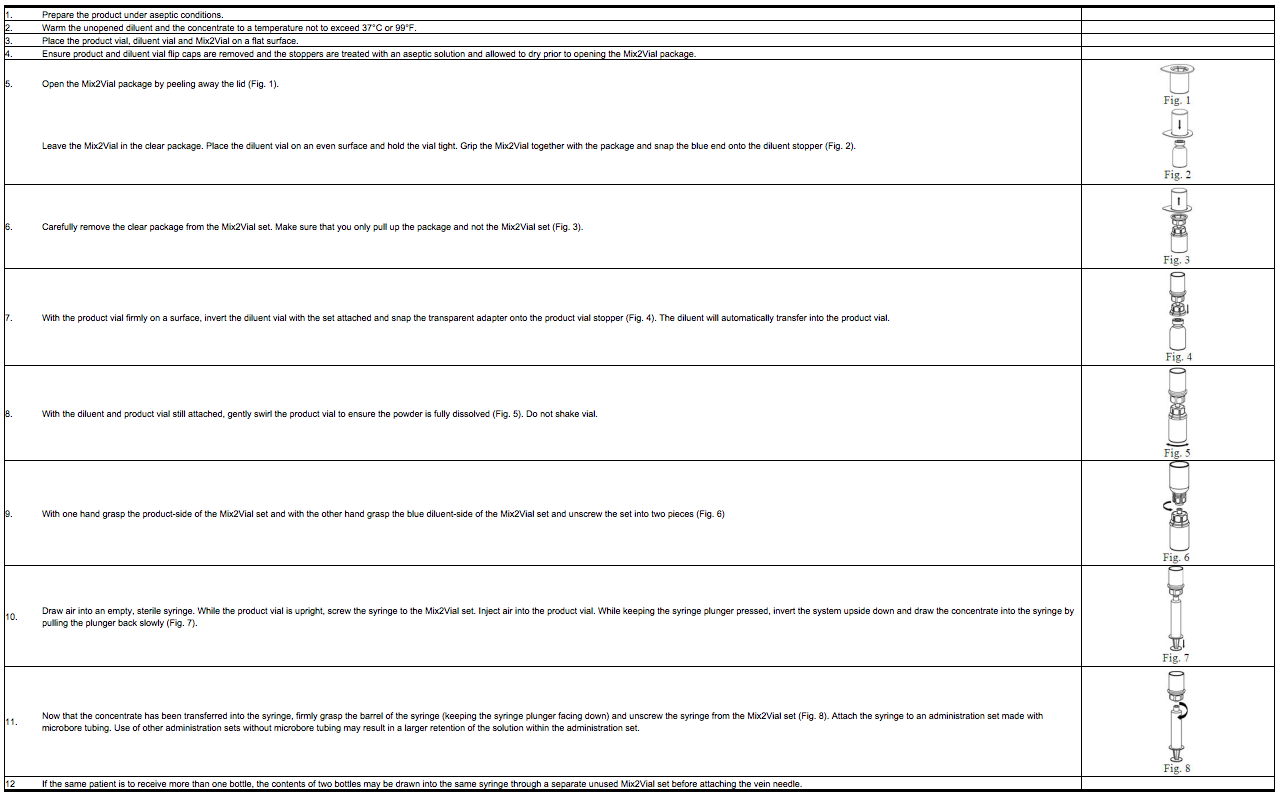
Preparation and Reconstitution
- Antihemophilic factor is administered by intravenous injection after reconstitution. Patients should follow the specific reconstitution and administration procedures provided by their physicians.
- Reconstitute and administer Antihemophilic factor with the components provided with each package. If any component of the package is opened or damaged, do not use this component.
- Product reconstitution, administration, and handling of the administration set and needles must be done with caution because percutaneous puncture with a needle contaminated with blood can transmit infectious viruses, including HIV (AIDS) and hepatitis. Place needles in a sharps container after single use. Discard all equipment, including any reconstituted Antihemophilic factor product, in an appropriate container. Obtain immediate medical attention if injury occurs.
- For instructions, patients should follow the recommendations in the FDA-Approved Patient Labeling.
- The procedures below are provided as general guidelines for the reconstitution of Antihemophilic factor.
- Work on a clean flat surface and wash hands thoroughly using soap and warm water before performing the procedures.
- Reconstitute the product with the components provided with each package. If any component of the package is opened or damaged, do not use this component.
- Filter the reconstituted product prior to administration to remove potential particulate matter in the solution. Filtering can be achieved by using the Mix2Vial™ vial adapter.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Amiodarone in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Amiodarone in adult patients
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
FDA Package Insert for Antihemophilic factor contains no information regarding FDA-labeled indications and dosage information for children.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Amiodarone in pediatric patients
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Amiodarone in pediatric patients
Contraindications
Antihemophilic factor is contraindicated in patients who have life-threatening hypersensitivity reactions, including anaphylaxis to mouse or hamster protein or other constituents of the product (sucrose, glycine, histidine, sodium, calcium chloride, polysorbate 80, sucrose, imidazole, tri-n-butyl phosphate, and copper).
Warnings
Hypersensitivity Reactions
- Hypersensitivity reactions, including anaphylaxis have been reported with Antihemophilic factor. Reported symptoms included facial swelling, flushing, hives, decrease in blood pressure, nausea, rash, restlessness, shortness of breath, tachycardia, tightness of the chest, tingling, urticaria, and vomiting.
- Antihemophilic factor contains trace amounts of mouse immunoglobulin G (MuIgG) and hamster (BHK) proteins. Patients treated with this product may develop hypersensitivity to these non-human mammalian proteins.
- Discontinue Antihemophilic factor if symptoms occur and seek immediate emergency treatment.
Neutralizing Antibodies
Neutralizing antibodies (inhibitors) have been reported following administration of Antihemophilic factor predominantly in previously untreated patients. Carefully monitor patients for the development of factor VIII inhibitors, using appropriate clinical observations and laboratory tests. If expected plasma factor VIII activity levels are not attained, or if bleeding is not controlled with an expected dose, perform an assay that measures factor VIII inhibitor concentration.
Cardiovascular Risk Factors
Hemophilic patients with cardiovascular risk factors or diseases may be at the same risk to develop cardiovascular events as non-hemophilic patients when clotting has been normalized by treatment with factor VIII.
Monitoring Laboratory Tests
- Monitor plasma factor VIII activity levels by the one-stage clotting assay to confirm the adequate factor VIII levels have been achieved and maintained, when clinically indicated.
- Monitor for development of factor VIII inhibitors. Perform assay to determine if factor VIII inhibitor is present. If expected factor VIII activity plasma levels are not attained or if bleeding is not controlled with the expected dose of Antihemophilic factor, use Bethesda Units (BU) to titer inhibitors.
- If the inhibitor is less than 10 BU per mL, the administration of additional Antihemophilic factor concentrate may neutralize the inhibitor and may permit an appropriate hemostatic response.
- If inhibitor titers are above 10 BU per mL, adequate hemostasis may not be achieved. The inhibitor titer may rise following Antihemophilic factor infusion as a result of an anamnestic response to factor VIII. The treatment or prevention of bleeding in such patients requires the use of alternative therapeutic approaches and agents.
Adverse Reactions
Clinical Trials Experience
- Serious adverse reactions seen with Antihemophilic factor are systemic hypersensitivity reactions, including bronchospastic reactions and/or hypotension and anaphylaxis, and the development of high-titer inhibitors necessitating alternative treatments to factor VIII.
- The most common adverse reactions (≥ 4%) observed in clinical trials were inhibitor formation in previously untreated patients (PUPs) and minimally treated patients (MTPs), skin-related hypersensitivity reactions (e.g., rash, pruritus), infusion site reactions (e.g., inflammation, pain), and central venous access device (CVAD) associated infections.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in clinical practice.
Previously Treated Patients (PTPs)
During the open-label clinical studies conducted in 73 PTPs, there were 24 adverse reactions reported in the course of 24,936 infusions. Adverse reactions reported by ≥ 4% of the patients are listed in Table 3 below.

Previously Untreated Patients (PUPs) and Minimally Treated Patients (MTPs)
In clinical studies with pediatric PUPs and MTPs, there were 29 adverse reactions reported in the course of 9,389 infusions. Adverse reactions reported by ≥ 4% of the patients are listed in Table 4 below.

Minimally Treated Patients (MTPs) in the Joint Outcome Study
In the Joint Outcome Study with pediatric MTPs treated with routine prophylaxis or episodic enhanced treatment for 5.5 years, 46 of the 65 randomized patients experienced adverse events over the study duration.

Immunogenicity
- In clinical studies with 73 PTPs (defined as having more than 100 exposure days), one patient had a pre-existing inhibitor.
- In the other 72 patients, followed over 4 years, no de novo inhibitors were observed.
- In clinical studies with pediatric PUPs and MTPs, inhibitor development was observed in 9 out of 60 patients (15%), 6 were high titer1 (> 5 BU) and 3 were low-titer inhibitors.
- Inhibitors were detected at a median number of 7 exposure days (range 2 to 16 exposure days).
- In the Joint Outcome Study with Antihemophilic factor,5 de novo inhibitor development was observed in 8 of 64 patients with negative baseline values (12.5%), 2 patients developed high titer1 (> 5 BU) and were withdrawn from the study. Six patients developed low-titer inhibitors.
- Inhibitors were detected at a median number of 44 exposure days (range 5 to 151 exposure days).
- The detection of antibody formation is dependent on the sensitivity and specificity of the assay.
- Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease.
- For these reasons, comparison of the incidence of antibodies to Antihemophilic factor with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
The following adverse reaction has been identified during post approval use of Antihemophilic factor. Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Sensory System – Dysgeusia
Additionally, available registries have reported inhibitor rates for PUPs with severe hemophilia A in the range of 28% to 38% for factor VIII products.
Drug Interactions
FDA Package Insert for Antihemophilic factor contains no information regarding drug interactions.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Animal reproduction studies have not been conducted with Antihemophilic factor. It is also not known whether Antihemophilic factor can cause fetal harm when administered to a pregnant woman or affect reproductive capacity. Antihemophilic factor should be given to a pregnant woman only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Antihemophilic factor in women who are pregnant.
Labor and Delivery
There is no information available on the effect of factor VIII replacement therapy on labor and delivery. Antihemophilic factor should be used only if clinically needed.
Nursing Mothers
It is not known whether this drug is excreted into human milk. Because many drugs are excreted into human milk, caution should be exercised if Antihemophilic factor is administered to a nursing woman.
Pediatric Use
There is no FDA guidance on the use of Tranexamic Acid in pediatric patients.
Geriatic Use
Clinical studies with Antihemophilic factor did not include patients aged 65 and over. Dose selection for an elderly patient should be individualized.
Gender
Safety and efficacy studies have been performed in previously untreated and minimally treated pediatric patients. Children, in comparison to adults, present higher factor VIII clearance values and, thus, lower half-life and recovery of factor VIII. This may be due to differences in body composition.7 Account for this difference in clearance when dosing or following factor VIII levels in the pediatric population. Routine prophylactic treatment in children ages 0–2.5 years with no pre-existing joint damage has been shown to reduce spontaneous joint bleeding and the risk of joint damage. This data can be extrapolated to ages >2.5–16 years for children who have no existing joint damage.
Race
There is no FDA guidance on the use of Antihemophilic factor with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Antihemophilic factor in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Antihemophilic factor in patients with hepatic impairment.
Females of Reproductive Potential and Males
here is no FDA guidance on the use of Antihemophilic factor in women of reproductive potentials and males
Immunocompromised Patients
There is no FDA guidance one the use of Antihemophilic factor in patients who are immunocompromised.
Others
(Description)
Administration and Monitoring
Administration
For intravenous use after reconstitution only.
- Inspect Antihemophilic factor visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Turbid or discolored solution should be discarded.
- Store the reconstituted Antihemophilic factor at room temperature prior to administration, but administer it within 3 hours.
- Administer Antihemophilic factor over a period of 1 to 15 minutes. Adapt the rate of administration to the response of each individual patient. Determine the pulse rate before and during administration of Antihemophilic factor. If there is a significant increase in pulse rate, reduce the rate of administration or temporarily halt the infusion allowing the symptoms to disappear promptly.
Monitoring
- Monitor plasma factor VIII activity levels by the one-stage clotting assay to confirm the adequate factor VIII levels have been achieved and maintained, when clinically indicated.
- Monitor for development of factor VIII inhibitors. Perform assay to determine if factor VIII inhibitor is present. If expected factor VIII activity plasma levels are not attained or if bleeding is not controlled with the expected dose of Antihemophilic factor, use Bethesda Units (BU) to titer inhibitors.
- If the inhibitor is less than 10 BU per mL, the administration of additional Antihemophilic factor concentrate may neutralize the inhibitor and may permit an appropriate hemostatic response.
- If inhibitor titers are above 10 BU per mL, adequate hemostasis may not be achieved. The inhibitor titer may rise following Antihemophilic factor infusion as a result of an anamnestic response to factor VIII. The treatment or prevention of bleeding in such patients requires the use of alternative therapeutic approaches and agents.
IV Compatibility
There is limited information about the IV Compatibilty.
Overdosage
FDA Package Insert for Antihemophilic factor contains no information regarding Adverse Reactions.
Pharmacology
Mechanism of Action
Antihemophilic factor temporarily replaces the missing clotting factor VIII that is needed for effective hemostasis.
Structure
(Description with picture)
Pharmacodynamics
The activated partial thromboplastin time (aPTT) is prolonged in patients with hemophilia. Determination of aPTT is a conventional in vitro assay for biological activity of factor VIII. Treatment with Antihemophilic factor normalizes the aPTT over the effective dosing period.
Pharmacokinetics
The pharmacokinetic properties of Antihemophilic factor were investigated in two separate studies in adult and pediatric previously treated patients (PTPs). Pharmacokinetic studies with Antihemophilic factor were conducted in 20 PTPs (ages 12 to 33 years) with severe hemophilia A. The pharmacokinetic parameters for Antihemophilic factor were measured in a randomized, crossover clinical trial with the predecessor HELIXATE product using a single dose administration of 50 IU per kg. After 24 weeks, the same dose of Antihemophilic factor was administered to the same patients. The recovery and half-life data for Antihemophilic factor were unchanged after 24 weeks of continued treatment with sustained efficacy and no evidence of factor VIII inhibition.

The pharmacokinetics of Antihemophilic factor were investigated in pediatric PTPs (4.4–18.1 years of age, average age 12).7 The pharmacokinetic parameters in children compared to adults show differences in higher clearance, lower incremental in vivo factor VIII recovery and a shorter factor VIII half-life. The pharmacokinetic parameters are depicted in Table 9.

Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been conducted with Antihemophilic factor to assess its mutagenic or carcinogenic potential and impairment of fertility. By inference, the predecessor product HELIXATE and Antihemophilic factor would be expected to have equivalent mutagenic and carcinogenic potential. The predecessor product did not demonstrate reverse mutation or chromosomal aberrations at doses substantially greater than the maximum expected clinical dose. In vivo evaluation with the predecessor product in animals using doses ranging between 10 and 40 times the expected clinical maximum also indicated that the predecessor product did not possess a mutagenic potential. Long-term investigations of carcinogenic potential in animals have not been performed due to the immune response to heterologous proteins in all non-human mammalian species.
Animal Toxicology and/or Pharmacology
Preclinical studies evaluating Antihemophilic factor in hemophilia A with mice, rats, rabbits, and dogs demonstrated safe and effective restoration of hemostasis. Doses several fold higher than the recommended clinical dose (related to body weight) did not demonstrate any acute or subacute toxic effect for Antihemophilic factor in laboratory animals. Antihemophilic factor has been shown to be comparable to the predecessor product HELIXATE with respect to its biochemical and physiochemical properties, as well as its non-clinical in vivo pharmacology and toxicology.
Clinical Studies
Previously Treated Patients (PTPs) Clinical Studies
A total of 73 patients with severe (≤ 2% FVIII) hemophilia A, ages 12–59, who had been previously treated with other recombinant or with plasma-derived AHF products, were treated up to 54 months in open label studies with Antihemophilic factor. A total of 5,684 bleeding episodes were treated during the studies; 92.7% of the bleeds were treated with one (79.7%) or two (13.0%) infusions. Patients could be treated with on-demand or prophylaxis. Regularly scheduled prophylaxis treatment represented 76% of all infusions (treatment regimens of 2–3 infusions per week). A total of 30 patients received Antihemophilic factor for 41 surgical procedures during the PTP studies. There were both minor and major surgery types, 16 and 25 respectively. Efficacy was measured by the attending surgeon based on a comparison of estimated blood loss from experience with non-hemophilic patients undergoing similar procedures. The surgeon or treating physician assigned a rating to the hemostatic outcome according to 4 categories: "excellent (blood loss less than expected)," "good (blood loss as expected)," "moderate (blood loss more than expected)," or "none (uncontrolled bleeding)." Hemostasis was rated as satisfactory ("excellent" or "good") in all cases.
Previously Untreated Patients (PUPs) and Minimally Treated Patients (MTPs) Clinical Study
Antihemophilic factor has been used in the treatment of bleeding episodes in pediatric PUPs and MTPs with severe (<2% FVIII) hemophilia A. There were 37 PUPs and 24 MTPs (defined as having equal to or less than 4 exposure days) treated with a total of 9,419 infusions of Antihemophilic factor for a follow up duration up to 3.1 years. A total of 1047 bleeding episodes were treated; the bleeds were treated with one (73%) or two (15%) infusions. A total of 27 surgical procedures were performed in 22 patients during the PUPs and MTPs study. There were both minor and major surgery types, 21 and 6 respectively. The attending surgeon measured efficacy and assigned a rating to the hemostatic outcome according to 4 categories as described above for PTPs. Hemostasis was rated as satisfactory ("excellent" or "good") in all cases.
Adult Prophylaxis for Bleeding Frequency Reduction
An ongoing, 3-year, multicenter, open-label, parallel-group, prospective, randomized, controlled clinical study of the effect of routine prophylaxis with Antihemophilic factor versus on-demand use on bleeding frequency in adults and adolescents included 84 PTPs with severe Hemophilia A (FVIII level < 1 IU/dL), age 15 to 50 years. Patients were matched at baseline on demographic and disease characteristics. The median number of bleeds in the year before enrollment was 18. Patients were randomized 1:1 to prophylaxis (25 units per kg three times a week) or on-demand use of Antihemophilic factor. Escalation of the prophylaxis dose by 5 units per kg/infusion after years 1 and 2, up to a maximum of 35 units per kg/infusion, was allowed. Bleeding frequency was analyzed in the intent-to-treat population after a median follow-up period of 1.4 years. Patients who received prophylaxis experienced statistically significantly fewer bleeds (p<0.0001) compared to patients treated on-demand regardless of baseline subgroups examined including age, bleeding history, and presence or absence of target joints. The ratio of the mean bleeding frequency was 15.2 (95% CI: 8.5, 27.2; p<0.0001) for on-demand versus prophylaxis, indicating that patients who received on-demand treatment experienced on average 15.2 times as many bleeds compared to patients treated with prophylaxis. The mean annualized bleed rates (bleeds/subject/year) were 37 in the on-demand group versus 2 in the prophylaxis group. The median annualized bleed rate (bleeds/subject/year) in the on-demand group was 33 versus zero in the prophylaxis group. Most of the bleeding occurred in joints: the median joint bleed rate (joint bleeds/subject/year) was 24 in the on-demand group versus zero in the prophylaxis group. The mean annualized joint bleed rate was 29 in the on-demand group versus 2 in the prophylaxis group. Twenty-two of 42 (52%) prophylaxis subjects experienced no bleeding, and 12 of 42 (29%) prophylaxis subjects experienced only 1–2 bleeds during the follow-up period. Among prophylaxis patients the mean number of infusions/week was 2.8, and the median dose per prophylaxis infusion was 26 units per kg.
Pediatric Prophylaxis for Joint Damage Risk Reduction
A total of 65 boys less than 30 months of age with severe hemophilia A (FVIII level ≤ 2 IU/dL) and with ≤ 2 bleeds into each index joint and normal baseline joint imaging, were observed for up to 5.5 years in a multicenter, open-label, prospective, randomized, controlled clinical study.5 Patients received either 25 IU per kg every other day (primary prophylaxis; n = 32) or at least 3 doses totaling a minimum of 80 IU per kg at the time of a bleeding episode (enhanced episodic; n = 33). Joint damage was evaluated by magnetic resonance imaging (MRI) or radiography, as well as the frequency of bleeding episodes. Joint damage detected by MRI or radiography in the ankles, knees, and elbows (i.e., index joints) was statistically significantly lower (p = 0.002) for subjects receiving prophylactic therapy (7%) than for subjects receiving episodic therapy (42%). This corresponds to a 6.29-fold relative risk of joint damage for subjects treated with enhanced episodic therapy compared to prophylaxis. The mean rate of index joint hemorrhages for subjects on episodic therapy was 4.89 bleeds per year, versus 0.63 bleeds per year observed in the prophylaxis arm. Three of 33 (9.1%) subjects in the episodic arm experienced recurrent life threatening bleeds (intracranial, gastrointestinal) compared to no subjects in the prophylaxis arm. On a per joint basis, joints in the regular prophylaxis arm were 8-fold more likely to remain damage-free than those in the episodic arm. Joint damage was most frequently observed in ankle joints and was detected at higher rates by MRI than by radiography. Ankles were also the index joint that demonstrated the highest frequency of bleeding events in this study (left ankle, mean 2.7 hemorrhages; right ankle, mean 2.6 hemorrhages). As shown in Table 10 below, the incidence of joint damage was statistically significantly lower in the prophylactic group as compared to the episodic treatment group when assessed by MRI, or either MRI or radiography, using predefined criteria (described below) for establishing joint damage. However, there was no statistically significant difference between the two groups when joint damage was assessed by radiography alone. To evaluate joint damage, MRIs were scored using a scale developed by Nuss et al.,14 and X-rays were scored using the method of Pettersson et al.15 Both scales have been validated in various clinical trials and are routinely used for joint damage evaluation in hemophiliacs. Joint damage was defined as bone and/or cartilage damage including subchondral cysts, erosions and cartilage loss with narrowing of joint space. This corresponded to a total MRI score of ≥ 7 or an X-ray score of ≥1 in any of the following categories: subchondral cysts, erosions of joint surfaces or narrowing of joint spaces. Images were read separately by two independent radiologists centrally. Any discrepant reading was read by an independent third radiologist who was not aware of the initial reading results. The concordant reading of two out of three readers was used for analysis purposes.

How Supplied
Antihemophilic factor is available as a kit in the following single-use glass vial sizes. A suitable volume of Sterile Water for Injection, USP and Mix2Vial™ filter transfer device are provided in the kit.
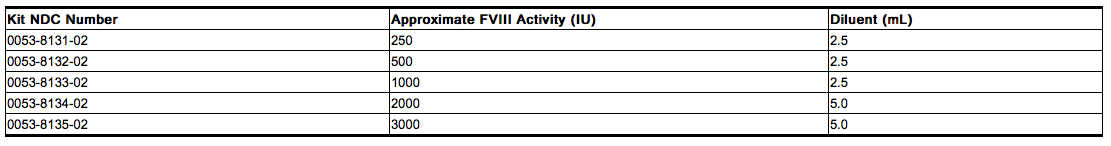
Actual factor VIII activity in IU is stated on the label of each Antihemophilic factor vial.
Storage
The product vial and diluent vial are not made with natural rubber latex.
Product as Packaged for Sale
Store Antihemophilic factor at +2°C to +8°C (36°F to 46°F) for up to 30 months from the date of manufacture. Within this period, Antihemophilic factor may be stored for a period of up to 12 months at temperatures up to +25°C or 77°F.
Record the starting date of room temperature storage on the unopened product carton. Once stored at room temperature, do not return the product to the refrigerator. The shelf-life then expires after storage at room temperature, or after the expiration date on the product vial, whichever is earlier.
Do not use Antihemophilic factor after the expiration date indicated on the vial.
Do not freeze.
Protect from extreme exposure to light and store the lyophilized powder in the carton prior to use.
Product After Reconstitution
After reconstitution, store the Antihemophilic factor solution at room temperature and administer within 3 hours.
Images
Drug Images
{{#ask: Page Name::Antihemophilic factor |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Antihemophilic factor |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
- Advise patients to report any adverse reactions or problems following Antihemophilic factor administration to their physician or healthcare provider.
- Allergic-type hypersensitivity reactions have been reported with Antihemophilic factor. Warn patients of the early signs of hypersensitivity reactions [including hives (rash with itching), generalized urticaria, tightness of the chest, wheezing, hypotension] and anaphylaxis. Advise patients to discontinue use of the product if these symptoms occur and seek immediate emergency treatment with resuscitative measures such as the administration of epinephrine and oxygen.
- Inhibitor formation may occur at any time in the treatment of a patient with hemophilia A. Advise patients to contact their physician or treatment center for further treatment and/or assessment, if they experience a lack of clinical response to factor VIII replacement therapy, as this may be a manifestation of an inhibitor.
- Advise patients to consult with their healthcare provider prior to travel. While traveling advise patients to bring an adequate supply of Antihemophilic factor based on their current regimen of treatment.
Precautions with Alcohol
Alcohol-Antihemophilic factor interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- HELIXATE FS ®[1]
- Koate DVI
- Monoclate-P
- antihemophilic factor
Look-Alike Drug Names
FDA Package Insert for Antihemophilic factor contains no information regarding Adverse Reactions.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Antihemophilic factor |Label Name=Antihemophilic factor_label_01.jpg
}}
{{#subobject:
|Label Page=Antihemophilic factor |Label Name=Antihemophilic factor_label_02.jpg
}}
{{#subobject:
|Label Page=Antihemophilic factor |Label Name=Antihemophilic factor_label_03.jpg
}}
{{#subobject:
|Label Page=Antihemophilic factor |Label Name=Antihemophilic factor_label_04.jpg
}}
{{#subobject:
|Label Page=Antihemophilic factor |Label Name=Antihemophilic factor_label_05.jpg
}}