Anomalous origins of coronary arteries
|
Coronary Angiography | |
|
General Principles | |
|---|---|
|
Anatomy & Projection Angles | |
|
Normal Anatomy | |
|
Anatomic Variants | |
|
Projection Angles | |
|
Epicardial Flow & Myocardial Perfusion | |
|
Epicardial Flow | |
|
Myocardial Perfusion | |
|
Lesion Complexity | |
|
ACC/AHA Lesion-Specific Classification of the Primary Target Stenosis | |
|
Lesion Morphology | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
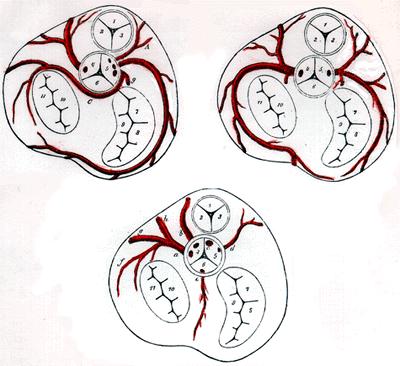
The coronary arteries are usually perpendicular to the aortic wall and they are radially arranged relative to the center of the aorta. The ostia may be rounding, oval, or elliptical, and the position of the ostium does not appear to affect the flow through it.
Classification
Anomalous origins of coronary arteries can be classified as
- Benign Coronary Anomalies
- Potentially More Serious Coronary Artery Anomalies
- Coronary Arteries Anomalies without Structural Heart Disease
- Coronary Arteries Anomalies with Structural Heart Disease
Benign Coronary Anomalies
- Separate ostia for the left anterior descending artery and the left circumflex from the left Valsalva sinus
- Absent left circumflex (with maximally dominant right coronary artery)
- Origin of left circumflex artery from right coronary artery or right sinus of Valsalva
- Ectopic origin of right coronary artery or left main trunk from posterior sinus of Valsalva
- Ectopic coronary origin from the ascending aorta
- Intercoronary communication
- Small coronary artery fistula
Potentially More Serious Coronary Artery Anomalies
- Ectopic coronary origin from the pulmonary artery
- Left main trunk from pulmonary artery: Bland-White-Garland syndrome
- Left anterior descending artery from pulmonary artery
- Right coronary artery from pulmonary artery
- All coronary arteries from pulmonary artery
- Ectopic origin of the left coronary artery from the right sinus of Valsalva
- Left main trunk from right sinus of Valsalva
- Left anterior descending artery from right sinus of Valsalva
- Right coronary artery from left sinus of Valsalva
Coronary Arteries Anomalies without Structural Heart Disease
Normal Variations
These anomalies have no any clinical consequences. Separate origin of the conus branch of the right coronary artery is common. The similar anomaly on the left side is ”separate origins of the left anterior descending and left circumflex coronary arteries” occurs in about 1% of people and is more frequent with bicuspid aortic valves. [1] [2]
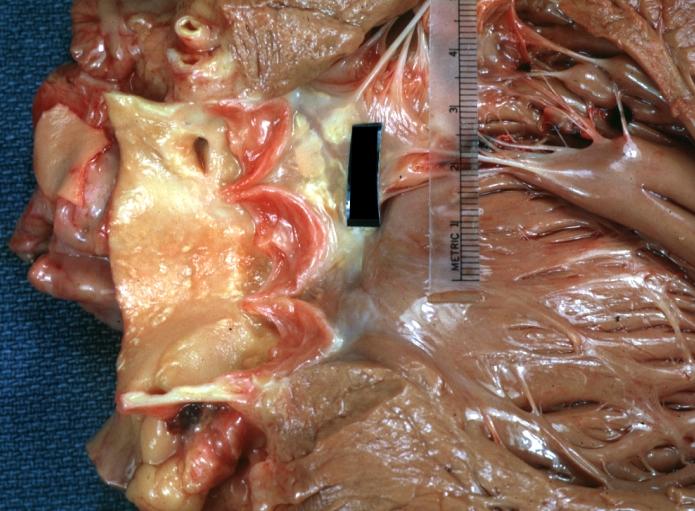
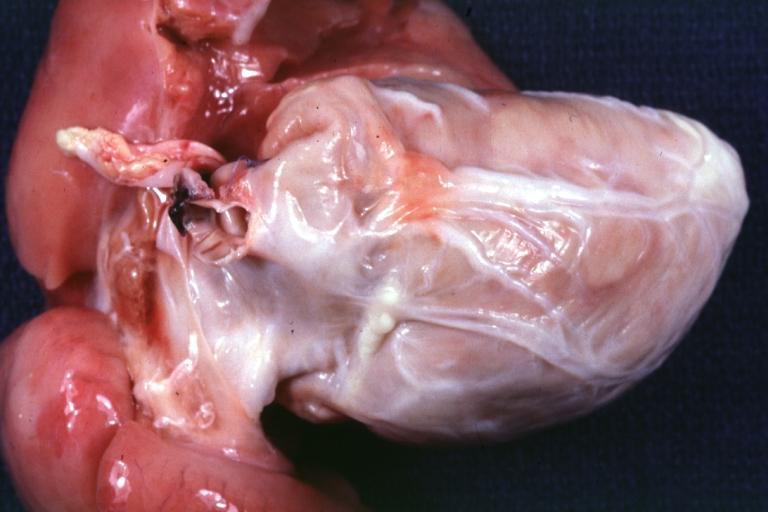
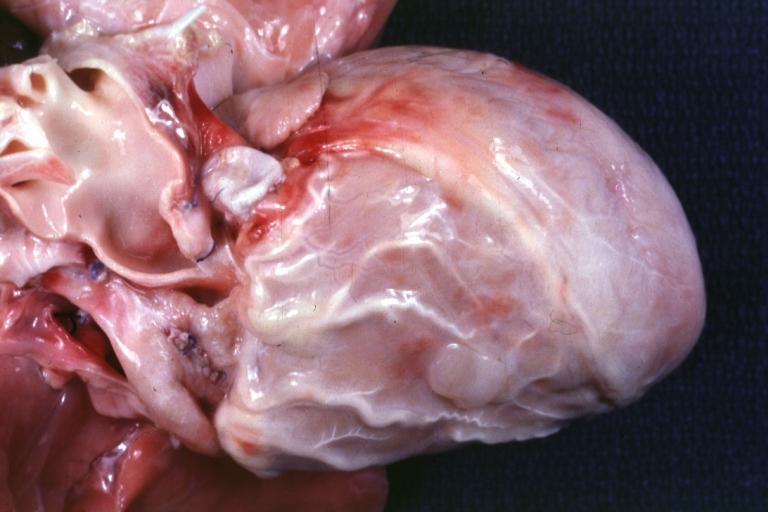
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
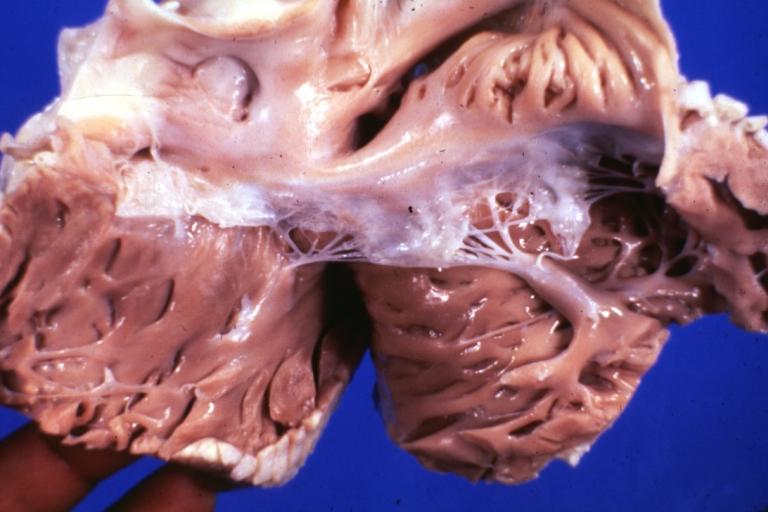
Gross natural color high origin of coronary well shown. The heart is enlarged.
-
Gross fixed tissue horizontal section of ventricle with intramural right coronary artery also lateral wall scar case of aortic valve prosthesis for aortic stenosis two years problem was arrhythmias
-
Anomalous Origin Coronary Artery: Gross natural color close-up view of right coronary artery cusp with two ostia
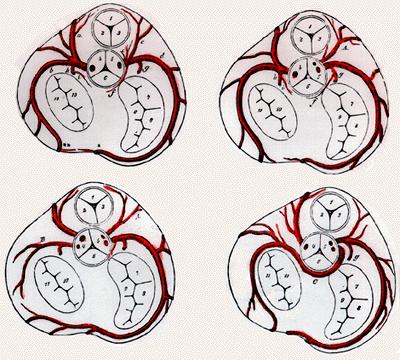
Abnormal Origin of Right or Left Coronary Artery from Inappropriate Sinus
Anomalous Origin of Left Coronary Arterial Branches from Right Sinus of Valsalva
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
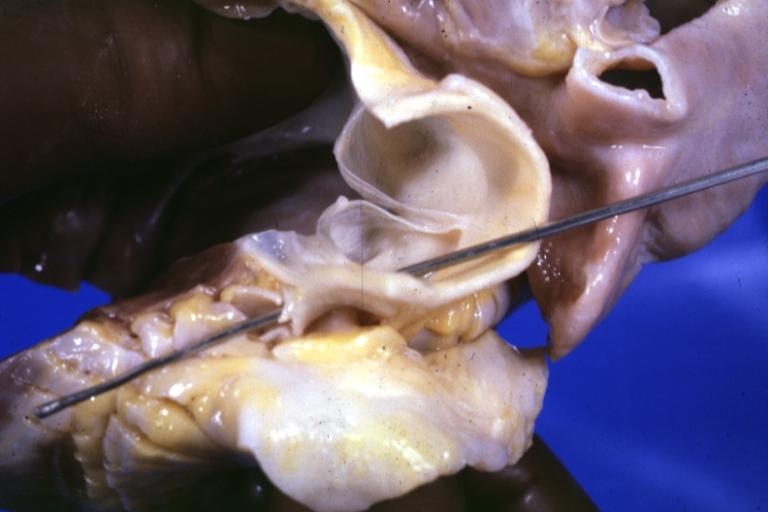
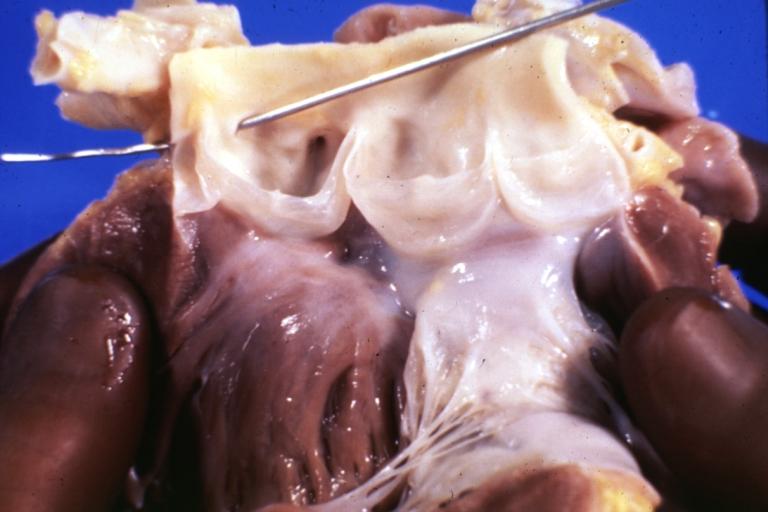
Gross aortic valve origin of left coronary artery from right sinus of Valsalva sudden unexpected death
-
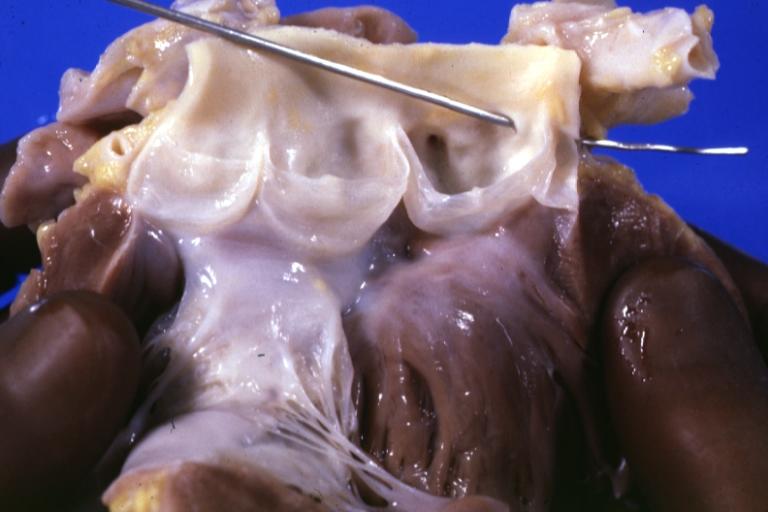
Gross left coronary artery originates from right sinus of Valsalva sudden unexpected death
-
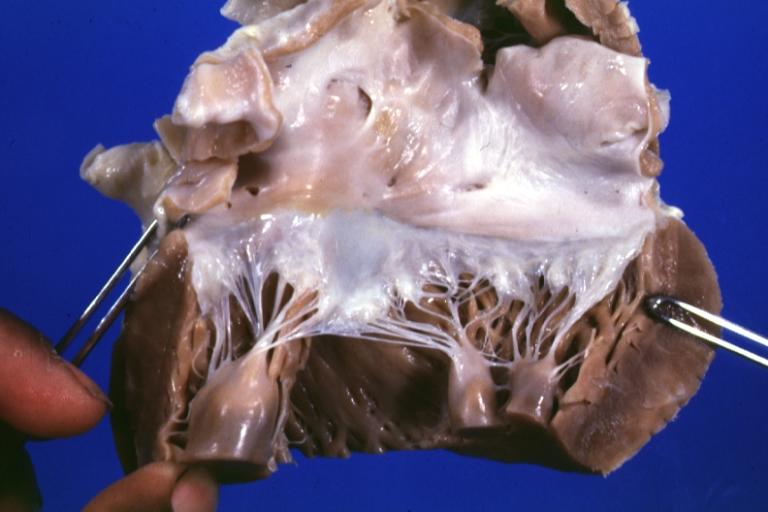
Anomalous Origin Coronary Artery: Gross left atrium and mitral valve normal
-
Gross view of aorta from above with probes in coronary artery to illustrate origin of left coronary from right sinus and to a degree at least the relation of the main left coronary with the aorta and pulmonary artery
-
Gross natural color close-up of aortic valve opened with probe in origin of left coronary artery which is in right cusp
-
Tricuspid valve normal: Gross natural color (a good view) 18 year old African-American male died due to anomalous origin left coronary artery from right cusp
Anomalous Origin of Right Coronary Arterial Branches from the Left Sinus of Valsalva
Single Coronary Artery
- From right coronary sinus
- Right coronary artery continues as left circumflex artery and Left anterior descending artery.
- Right coronary artery gives off left main coronary artery
- Right coronary artery gives off left anterior descending artery and left circumflex artery
- From left coronary sinus
- Left main coronary artery gives off left anterior descending artery, left circumflex artery, and right coronary artery
- Left circumflex artery continues as right coronary artery
- Left circumflex artery gives off right coronary artery
- Left anterior descending artery gives off right coronary artery
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
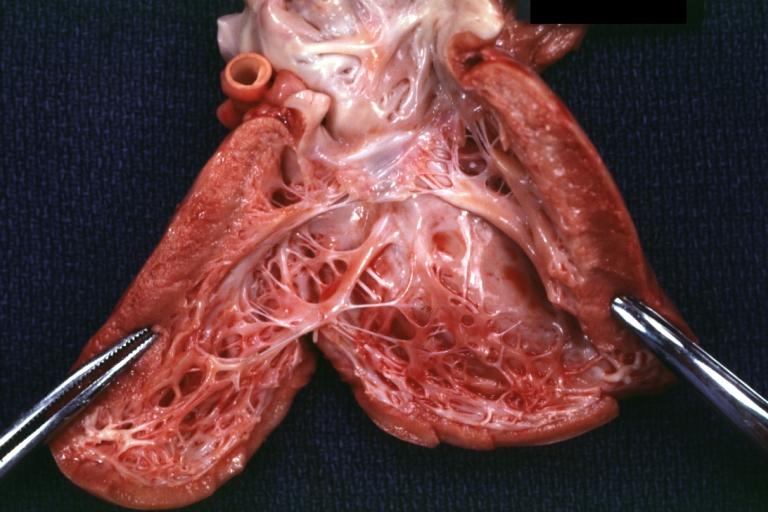
Gross shows common origin of right and left coronary arteries from right coronary cusp
-
Gross natural color opened right coronary sinus showing single origin of both coronaries
Rare Coronary Anomalies
Coronary Atresia
Total absence of the epicardial (extramural) coronary arteries is rare and occurs most often with pulmonary atresia and aortic atresia.
In these congenital anomalies, pressure in the small but hypertrophied right or left ventricle is similar or higher than aortic pressure, and enlarged sinusoids carry blood from the ventricle to be distributed in the distal coronary arteries. [3] [4]
Stenosis or Atresia of a Coronary Ostium
- Stenosis or atresia of the ostium or first few millimeters of the left main coronary artery is one of the rarest of the congenital coronary artery anomalies.
- The more distal branches are normal and develop multiple collaterals from the right coronary artery.
- According to published literature, presentation range is 3 months to 60 years of age. Usual presentation with;
All Coronary Arteries from Pulmonary Artery
- Both right and left coronary arteries, or a single coronary artery, may come from the pulmonary trunk.
- These children do not survive infancy without surgical intervention unless there is a cardiac lesion causing pulmonary hypertension. [5]
Left Anterior Descending Coronary Artery from the Pulmonary Artery
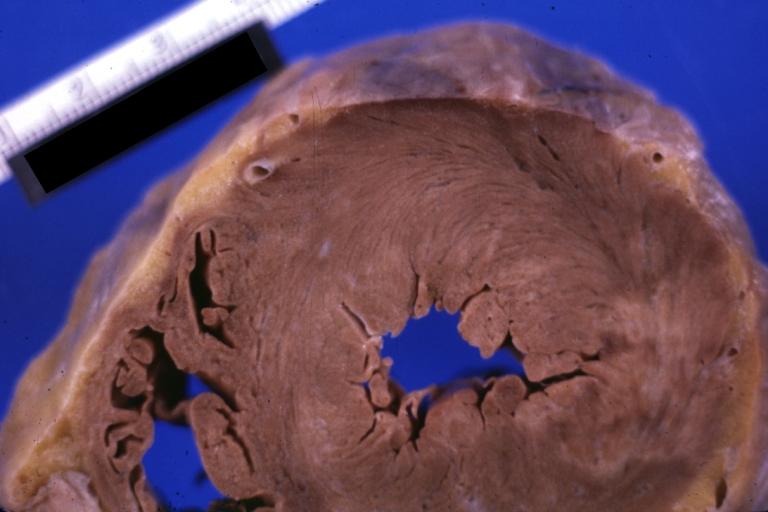
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Endocardial Fibroelastosis: Gross fair example LV endocardial thickening associated with anomalous origin of left coronary artery from pulmonary artery
-
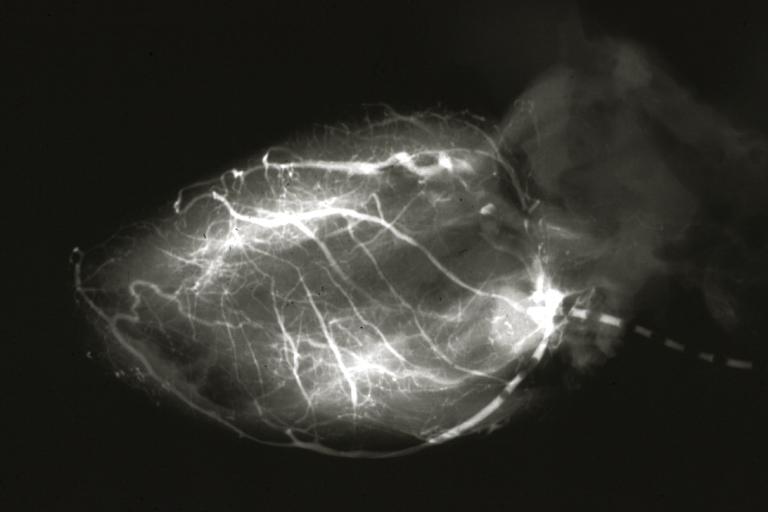
Left Coronary Artery Anomalous Origin from Pulmonary artery: Angiogram postmortem after switch of left coronary to aorta
Left Circumflex Coronary Artery from the Pulmonary Artery or Branches
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
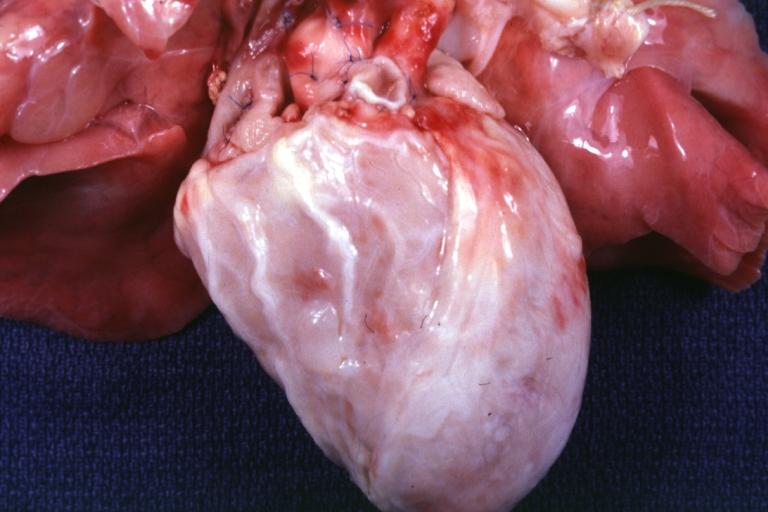
Coronary Artery Anomalous Origin Left from Pulmonary artery: Gross natural color anterior view of heart. Large marginal type coronary branches over anterior aspect of right ventricle.
-
Coronary Artery Anomalous Origin Left from Pulmonary artery: Gross natural color anterior view of heart. Large marginal type coronary branches over anterior aspect of right ventricle.
-
Coronary Artery Anomalous Origin Left from Pulmonary artery: Gross natural color anterior view of hear showing large marginal type branches over anterior right ventricle 5 month old infant died after operation switching artery to aorta
-
Coronary Artery Anomalous Origin Left from Pulmonary artery: Gross fixed tissue. Horizontal sections of ventricles showing thinning in anterior left ventricle due to scar there are some peculiar spots on the ventricles in this photo that probably are artifacts.
Right Coronary Artery from the Pulmonary Artery
- Rare, only about 10% of left main coronary artery originated from the pulmonary artery. [6] [7] [8] [9] [10] [11]
- Almost always found as an incidental autopsy finding of sudden death, and if diagnosed before death it has been associated with:
- Symptoms of myocardial ischemia
- Syncope
- Cardiomyopathy
2008 ACC/AHA Guidelines for the Management of Adults With Congenital Heart Disease (DO NOT EDIT)[12]
Evaluation and Surgical Intervention (DO NOT EDIT)[12]
| Class I |
| "1. Any patient with CHD who has had coronary artery manipulation should be evaluated for coronary artery patency, function, and anatomic integrity at least once in adulthood. (Level of Evidence: C)" |
| ”2. Surgeons with training and expertise in CHD should perform operations for the treatment of coronary artery anomalies. (Level of Evidence: C)" |
Coronary Anomalies Associated With Supravalvular Aortic Stenosis (DO NOT EDIT)[12]
| Class I |
| "1. Adults with a history or presence of SupraAS should be screened every 1 or 2 years for myocardial ischemia. (Level of Evidence: C)" |
| "2. Interventions for coronary artery obstruction in patients with SupraAS should be performed in ACHD centers with demonstrated expertise in the interventional management of these patients. (Level of Evidence: C)" |
Coronary Anomalies Associated With Tetralogy of Fallot (DO NOT EDIT)[12]
| Class I |
| "1. Coronary artery anatomy should be determined before any intervention for RV outflow. (Level of Evidence: C)" |
Coronary Anomalies Associated With Dextro-Transposition of the Great Arteries After Arterial Switch Operation (DO NOT EDIT)[12]
| Class I |
| "1. Adult survivors with dextro-TGA (d-TGA) after arterial switch operation (ASO) should have noninvasive ischemia testing every 3 to 5 years. (Level of Evidence: C)" |
Congenital Coronary Anomalies of Ectopic Arterial Origin (DO NOT EDIT)[12]
| Class I |
| "1. The evaluation of individuals who have survived unexplained aborted sudden cardiac death or with unexplained life-threatening arrhythmia, coronary ischemic symptoms, or LV dysfunction should include assessment of coronary artery origins and course. (Level of Evidence: B)" |
| ”2. CT or magnetic resonance angiography is useful as the initial screening method in centers with expertise in such imaging. (Level of Evidence: B)" |
| ”3. Surgical coronary revascularization should be performed in patients with any of the following: |
| a. Anomalous left main coronary artery coursing between the aorta and pulmonary artery. (Level of Evidence: B) |
| b. Documented coronary ischemia due to coronary compression (when coursing between the great arteries or in intramural fashion). (Level of Evidence: B) |
| c. Anomalous origin of the right coronary artery between aorta and pulmonary artery with evidence of ischemia. (Level of Evidence: B)" |
| Class IIa |
| "1. Surgical coronary revascularization can be beneficial in the setting of documented vascular wall hypoplasia, coronary compression, or documented obstruction to coronary flow, regardless of inability to document coronary ischemia. (Level of Evidence: C)" |
| ”2. Delineation of potential mechanisms of flow restriction via intravascular ultrasound can be beneficial in patients with documented anomalous coronary artery origin from the opposite sinus. (Level of Evidence: C)" |
| Class IIb |
| "1. Surgical coronary revascularization may be reasonable in patients with anomalous left anterior descending coronary artery coursing between the aorta and pulmonary artery. (Level of Evidence: C)" |
Anomalous Left Coronary Artery From the Pulmonary Artery (DO NOT EDIT)[12]
| Class I |
| "1. In patients with an anomalous left coronary artery from the pulmonary artery (ALCAPA), reconstruction of a dual coronary artery supply should be performed. The surgery should be performed by surgeons with training and expertise in CHD at centers with expertise in the management of anomalous coronary artery origins. (Level of Evidence: C)" |
| ”2. For adult survivors of ALCAPA repair, clinical evaluation with echocardiography and noninvasive stress testing is indicated every 3 to 5 years. (Level of Evidence: C)" |
Coronary Arteriovenous Fistula (DO NOT EDIT)[12]
| Class I |
| "1. If a continuous murmur is present, its origin should be defined either by echocardiography, MRI, CT angiography, or cardiac catheterization. (Level of Evidence: C)" |
| ”2. A large coronary arteriovenous fistula (CAVF), regardless of symptomatology, should be closed via either a transcatheter or surgical route after delineation of its course and its potential to fully obliterate the fistula. (Level of Evidence: C)" |
| ”3. A small to moderate CAVF in the presence of documented myocardial ischemia, arrhythmia, otherwise unexplained ventricular systolic or diastolic dysfunction or enlargement, or endarteritis should be closed via either a transcatheter or surgical approach after delineation of its course and its potential to fully obliterate the fistula. (Level of Evidence: C)" |
| Class III |
| "1. Patients with small, asymptomatic CAVF should not undergo closure of CAVF. (Level of Evidence: C)" |
| Class IIa |
| "1. Clinical follow-up with echocardiography every 3 to 5 years can be useful for patients with small, asymptomatic CAVF to exclude development of symptoms or arrhythmias or progression of size or chamber enlargement that might alter management. (Level of Evidence: C)" |
Management Strategies for CAVF(DO NOT EDIT)[12]
| Class I |
| "1. Surgeons with training and expertise in CHD should perform operations for management of patients with CAVF. (Level of Evidence: C)" |
| ”2. Transcatheter closure of CAVF should be performed only in centers with expertise in such procedures. (Level of Evidence: C)" |
| ”3. Transcatheter delineation of CAVF course and access to distal drainage should be performed in all patients with audible continuous murmur and recognition of CAVF. (Level of Evidence: C)" |
References
- ↑ Baroldi G, Scomazzoni G. Coronary circulation in the normal and the pathologic heart. Washington, DC: Office of the Surgeon General, 1967
- ↑ Datta J, White CS, Gilkeson RC, Meyer CA, Kansal S, Jani ML, Arildsen RC, Read K Anomalous Coronary Arteries in Adults: Depiction at Multi–Detector Row CT Angiography. Radiology 2005 235: 812-818.
- ↑ Musiani A, Cernigliaro C, Sansa M, Maselli D, De Gasperis C. Left main coronary artery atresia: literature review and therapeutical considerations. Eur J Cardiothorac Surg. 1997 Mar; 11(3):505-14. PMID 9105816
- ↑ Elian D, Hegesh J, Agranat O, Guetta V, Har-Zahav Y, Rath S, Chouraqui P, Di Segni E. Left main coronary artery atresia: extremely rare coronary anomaly in an asymptomatic adult and an adolescent soccer player. Cardiol Rev. 2003 May-Jun;11(3):160-2. PMID 12705847
- ↑ Ochoa-Ramirez E, Valdez-Garza HE, Reyes-Gonzalez R, et al. Double anomalous coronary origin from the pulmonary artery: Successful surgical correction in an infant. Tex Heart Inst J 2005;32:348-50.
- ↑ Coe JY, Radley-Smith R, Yacoub M. Clinical and hemodynamic significance of anomalous origin of the right coronary artery from the pulmonary artery. Thorac Cardiovasc Surg 1982;30:84-7.
- ↑ Fontana RS, Edwards JE. Congenital Cardiac Disease: A Review of 357 Cases Studied Pathologically. Philadelphia: WB Saunders, 1962.
- ↑ Ogden JA. Congenital anomalies of the coronary arteries. Am J Cardiol 1970;25:474-79.
- ↑ Neufeld HN, Schneeweiss A. Coronary Artery Disease in Infants and Children. Philadelphia: Lea & Febiger, 1983.
- ↑ Roberts WC. Major anomalies of coronary arterial origin seen in adulthood. Am Heart J 1986; 111: 941-63.
- ↑ Yao CT, Wang JN, Yeh CN, et al. Isolated anomalous origin of right coronary artery from the main pulmonary artery. J Card Surg 2005;20:487-89.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA; et al. (2008). "ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (23): e1–121. doi:10.1016/j.jacc.2008.10.001. PMID 19038677.