Pericarditis physical examination: Difference between revisions
(New page: {{SI}} {{CMG}} '''Associate Editor-In-Chief:''' {{CZ}} {{Editor Join}} == Physical Examination == === Appearance of the Patient with Pericarditis === # Fever less than 39° C...) |
m (Bot: Removing from Primary care) |
||
| (40 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | __NOTOC__ | ||
{{Pericarditis}} | |||
{{CMG}} | {{CMG}}; {{AE}} {{CZ}}{{Homa}} | ||
==Overview== | |||
The classic [[medical sign|sign]] of pericarditis is a [[pericardial rub|pericardial friction rub]]. A careful examination must be performed to exclude the presence of [[cardiac tamponade]], a dangerous complication of pericarditis. If [[cardiac tamponade]] is present, then [[pulsus paradoxus]], [[hypotension]], an elevated [[jugular venous pressure]], and [[peripheral edema]] may be present. | |||
== | ==Overview== | ||
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3]. | |||
OR | |||
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3]. | |||
OR | |||
The presence of [finding(s)] on physical examination is diagnostic of [disease name]. | |||
== | OR | ||
The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | |||
==Physical Examination== | |||
Physical examination of patients with [disease name] is usually normal. | |||
OR | |||
Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3]. | |||
OR | |||
The presence of [finding(s)] on physical examination is diagnostic of [disease name]. | |||
OR | |||
The presence of [finding(s)] on physical examination is highly suggestive of [disease name]. | |||
===Appearance of the Patient=== | |||
*Patients with pericarditis usually appear [general appearance]. | |||
===Vital Signs=== | |||
*High-grade / low-grade fever | |||
*[[Hypothermia]] / hyperthermia may be present | |||
*[[Tachycardia]] with regular pulse or (ir)regularly irregular pulse | |||
*[[Bradycardia]] with regular pulse or (ir)regularly irregular pulse | |||
*Tachypnea / bradypnea | |||
*Kussmal respirations may be present in _____ (advanced disease state) | |||
*Weak/bounding pulse / pulsus alternans / paradoxical pulse / asymmetric pulse | |||
*High/low blood pressure with normal pulse pressure / [[wide pulse pressure]] / [[narrow pulse pressure]] | |||
===Skin=== | |||
* Skin examination of patients with pericarditis is usually normal. | |||
* [[Pallor]] may be seen in the patients that pericarditis is secondary to [[tuberculosis]], [[uremia]], [[neoplasia]], or rheumatic carditis | |||
===HEENT=== | |||
* HEENT examination of patients with pericarditis is usually normal. | |||
===Neck=== | |||
* Neck examination of patients with [disease name] is usually normal. | |||
OR | |||
*[[Jugular venous distension]] | |||
*[[Carotid bruits]] may be auscultated unilaterally/bilaterally using the bell/diaphragm of the otoscope | |||
*[[Lymphadenopathy]] (describe location, size, tenderness, mobility, and symmetry) | |||
*[[Thyromegaly]] / thyroid nodules | |||
*[[Hepatojugular reflux]] | |||
===Lungs=== | |||
* Pulmonary examination of patients with [disease name] is usually normal. | |||
OR | |||
* Asymmetric chest expansion OR decreased chest expansion | |||
*Lungs are hyporesonant OR hyperresonant | |||
*Fine/coarse [[crackles]] upon auscultation of the lung bases/apices unilaterally/bilaterally | |||
*Rhonchi | |||
*Vesicular breath sounds OR distant breath sounds | |||
*Expiratory wheezing OR inspiratory wheezing with normal OR delayed expiratory phase | |||
*[[Wheezing]] may be present | |||
*[[Egophony]] present/absent | |||
*[[Bronchophony]] present/absent | |||
*Normal/reduced [[tactile fremitus]] | |||
===Heart=== | |||
* Cardiovascular examination of patients with [disease name] is usually normal. | |||
OR | |||
*Chest tenderness upon palpation | |||
*PMI within 2 cm of the sternum (PMI) / Displaced point of maximal impulse (PMI) suggestive of ____ | |||
*[[Heave]] / [[thrill]] | |||
*[[Friction rub]] | |||
*[[Heart sounds#First heart tone S1, the "lub"(components M1 and T1)|S1]] | |||
*[[Heart sounds#Second heart tone S2 the "dub"(components A2 and P2)|S2]] | |||
*[[Heart sounds#Third heart sound S3|S3]] | |||
*[[Heart sounds#Fourth heart sound S4|S4]] | |||
*[[Heart sounds#Summation Gallop|Gallops]] | |||
*A high/low grade early/late [[systolic murmur]] / [[diastolic murmur]] best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the stethoscope | |||
===Abdomen=== | |||
* Abdominal examination of patients with [disease name] is usually normal. | |||
OR | |||
*[[Abdominal distension]] | |||
*[[Abdominal tenderness]] in the right/left upper/lower abdominal quadrant | |||
*[[Rebound tenderness]] (positive Blumberg sign) | |||
*A palpable abdominal mass in the right/left upper/lower abdominal quadrant | |||
*Guarding may be present | |||
*[[Hepatomegaly]] / [[splenomegaly]] / [[hepatosplenomegaly]] | |||
*Additional findings, such as obturator test, psoas test, McBurney point test, Murphy test | |||
===Back=== | |||
* Back examination of patients with [disease name] is usually normal. | |||
OR | |||
*Point tenderness over __ vertebrae (e.g. L3-L4) | |||
*Sacral edema | |||
*Costovertebral angle tenderness bilaterally/unilaterally | |||
*Buffalo hump | |||
===Genitourinary=== | |||
* Genitourinary examination of patients with [disease name] is usually normal. | |||
OR | |||
*A pelvic/adnexal mass may be palpated | |||
*Inflamed mucosa | |||
*Clear/(color), foul-smelling/odorless penile/vaginal discharge | |||
===Neuromuscular=== | |||
* Neuromuscular examination of patients with pericarditis is usually normal. | |||
OR | |||
*Patient is usually oriented to persons, place, and time | |||
* Altered mental status | |||
* Glasgow coma scale is ___ / 15 | |||
* Clonus may be present | |||
* Hyperreflexia / hyporeflexia / areflexia | |||
* Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally | |||
* Muscle rigidity | |||
* Proximal/distal muscle weakness unilaterally/bilaterally | |||
* ____ (finding) suggestive of cranial nerve ___ (roman numerical) deficit (e.g. Dilated pupils suggestive of CN III deficit) | |||
*Unilateral/bilateral upper/lower extremity weakness | |||
*Unilateral/bilateral sensory loss in the upper/lower extremity | |||
*Positive straight leg raise test | |||
*Abnormal gait (describe gait: e.g. ataxic (cerebellar) gait / steppage gait / waddling gait / choeiform gait / Parkinsonian gait / sensory gait) | |||
*Positive/negative Trendelenburg sign | |||
*Unilateral/bilateral tremor (describe tremor, e.g. at rest, pill-rolling) | |||
*Normal finger-to-nose test / Dysmetria | |||
*Absent/present dysdiadochokinesia (palm tapping test) | |||
===Extremities=== | |||
* Extremities examination of patients with pericarditis is usually normal. | |||
==Appearance of the Patient== | |||
*[[Fever]] less than 39°C or 102.2°F | |||
** Patients who are elderly may not exhibit [[fever]]; however, they may be [[hypothermic]], especially those with [[renal failure]]. | |||
*[[Chills]] (suppurative pericarditis and idiopathic viral pericarditis) | |||
*[[Weakness]] | |||
*[[Anxiety]] | |||
*[[Pallor]] (may also indicate [[tuberculosis]], [[uremia]], [[neoplasia]], or rheumatic carditis) | |||
==Heart== | |||
A [[pericardial rub]] or [[pericardial friction rub]] is the classic physical examination finding in pericarditis. It is usually heard in the setting of an acute pericarditis, and occasionally with either subacute or chronic pericarditis. It is best heard with the diaphragm of the stethoscope. [[Inflammation]] of the pericardial sac causes the parietal and visceral surfaces of the roughened [[pericardium]] to rub against each other. This produces an [[extra cardiac sound]] of to-and-fro character with both systolic and diastolic components. One, two, or three components of a [[pericardial friction rub]] may be audible. A three-component rub indicates the presence of [[pericarditis]] and serves to distinguish a pericardial rub from a [[pleural friction rub]], which ordinarily has two components. It resembles the sound of squeaky leather and is often described as grating, scratching, or rasping. The sound may seem louder than or may even mask the other [[heart sound]]s. Friction rubs are usually best heard between the apex and [[sternum]] but may be widespread. The sound has three components, two diastolic and one systolic.<br> | |||
There are several different [[pericardial rub]]s that can be auscultated: | |||
===Endopericardial Rub=== | |||
This rub occurs as the result of inflamed, scarred or tumor-invaded serosal surfaces of [[pericardium]]. | |||
===Exopericardial Rub=== | |||
This rub occurs after [[sclerotherapy]] of effusions, and is due to friction between the parietal [[pericardium]] and the [[pleura]] (or occasionally the chest wall). | |||
===Endo-exopericardial Rub=== | |||
This rub occurs with both of the above. | |||
===Pleuropericardial Rub=== | |||
This rub occurs as a result of both pleural and pericardial [[inflammation]]. | |||
==Signs of Significant Pericardial Effusion or Cardiac Tamponade== | |||
Classical [[cardiac tamponade]] presents three signs, known as [[Beck's triad]].<ref>Gwinnutt, C., Driscoll, P. (Eds) (2003) (2nd Ed.) Trauma Resuscitation: The Team Approach. Oxford: BIOS Scientific Publishers Ltd. ISBN 978-1859960097 </ref> Beck's triad consists of [[hypotension]] due to a decreased [[stroke volume]], [[jugular venous distension]] due to impaired venous return to the heart, and muffled [[heart sounds]] due to fluid inside the pericardium.<ref>Dolan, B., Holt, L. (2000). Accident & Emergency: Theory into practice. London: Bailliere Tindall ISBN 978-0702022395</ref> Another sign of tamponade on physical examination includes [[pulsus paradoxus]] (a drop of at least 10 mmHg in arterial [[blood pressure]] on [[inspiration]]).<ref>Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886 </ref> There may also be general signs and symptoms of cardiogenic [[shock]] (such as [[tachycardia]], [[breathlessness]], poor perfusion of the extremities, and decreasing [[Glasgow coma scale|level of consciousness]]). [[Peripheral edema]] may be present. Hemodynamic changes diminish S<sub>1</sub> and S<sub>2</sub>. As ventricular volume shrinks disproportionately, there may be psuedoprolapse/true prolapse of mitral and/or tricuspid valvular structures that results in clicking sounds. | |||
[[Image:150072-1332319-156951-1951463.jpg|thumb|left|Recording of aortic pressure showing [[pulsus paradoxus]]. Systolic pressure declines 20 mmHg on [[inspiration]].]] | |||
Copyleft image obtained courtesy of Zhi Zhou, MD. | |||
==Signs of Pericardial Constriction== | |||
*Elevation of the [[JVP]] ([[jugular venous pulse]]): The waveform of [[pericardial constriction]] is characteristic with a prominent 'x' and 'y' descent. | |||
*[[Kussmaul’s sign]]: It may be found in about 10% of patients. It occurs because the fall in intrathoracic pressure during [[inspiration]] is not transmitted to the cardiac chambers and pericardial space. | |||
*[[Pulsus paradoxus]]: Though more typical in [[cardiac tamponade]], it can be seen in 20% of patients with [[pericardial constriction]]. | |||
*Widely split [[S2]] and a pericardial knock: They can be present in approximately 50% of patients. | |||
*Pulsatile liver, [[ascites]], and scrotal [[edema]] | |||
*[[Peripheral edema]] | |||
==References== | |||
{{Reflist|2}} | |||
[[de:Perikarditis]] | [[de:Perikarditis]] | ||
[[es:Pericarditis]] | [[es:Pericarditis]] | ||
| Line 144: | Line 198: | ||
[[tr:Perikard hastalıkları]] | [[tr:Perikard hastalıkları]] | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Medicine]] | |||
[[Category:Cardiology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Intensive care medicine]] | |||
Latest revision as of 23:39, 29 July 2020
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis physical examination On the Web |
|
American Roentgen Ray Society Images of Pericarditis physical examination |
|
Risk calculators and risk factors for Pericarditis physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] Homa Najafi, M.D.[3]
Overview
The classic sign of pericarditis is a pericardial friction rub. A careful examination must be performed to exclude the presence of cardiac tamponade, a dangerous complication of pericarditis. If cardiac tamponade is present, then pulsus paradoxus, hypotension, an elevated jugular venous pressure, and peripheral edema may be present.
Overview
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Physical Examination
Physical examination of patients with [disease name] is usually normal.
OR
Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Appearance of the Patient
- Patients with pericarditis usually appear [general appearance].
Vital Signs
- High-grade / low-grade fever
- Hypothermia / hyperthermia may be present
- Tachycardia with regular pulse or (ir)regularly irregular pulse
- Bradycardia with regular pulse or (ir)regularly irregular pulse
- Tachypnea / bradypnea
- Kussmal respirations may be present in _____ (advanced disease state)
- Weak/bounding pulse / pulsus alternans / paradoxical pulse / asymmetric pulse
- High/low blood pressure with normal pulse pressure / wide pulse pressure / narrow pulse pressure
Skin
- Skin examination of patients with pericarditis is usually normal.
- Pallor may be seen in the patients that pericarditis is secondary to tuberculosis, uremia, neoplasia, or rheumatic carditis
HEENT
- HEENT examination of patients with pericarditis is usually normal.
Neck
- Neck examination of patients with [disease name] is usually normal.
OR
- Jugular venous distension
- Carotid bruits may be auscultated unilaterally/bilaterally using the bell/diaphragm of the otoscope
- Lymphadenopathy (describe location, size, tenderness, mobility, and symmetry)
- Thyromegaly / thyroid nodules
- Hepatojugular reflux
Lungs
- Pulmonary examination of patients with [disease name] is usually normal.
OR
- Asymmetric chest expansion OR decreased chest expansion
- Lungs are hyporesonant OR hyperresonant
- Fine/coarse crackles upon auscultation of the lung bases/apices unilaterally/bilaterally
- Rhonchi
- Vesicular breath sounds OR distant breath sounds
- Expiratory wheezing OR inspiratory wheezing with normal OR delayed expiratory phase
- Wheezing may be present
- Egophony present/absent
- Bronchophony present/absent
- Normal/reduced tactile fremitus
Heart
- Cardiovascular examination of patients with [disease name] is usually normal.
OR
- Chest tenderness upon palpation
- PMI within 2 cm of the sternum (PMI) / Displaced point of maximal impulse (PMI) suggestive of ____
- Heave / thrill
- Friction rub
- S1
- S2
- S3
- S4
- Gallops
- A high/low grade early/late systolic murmur / diastolic murmur best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the stethoscope
Abdomen
- Abdominal examination of patients with [disease name] is usually normal.
OR
- Abdominal distension
- Abdominal tenderness in the right/left upper/lower abdominal quadrant
- Rebound tenderness (positive Blumberg sign)
- A palpable abdominal mass in the right/left upper/lower abdominal quadrant
- Guarding may be present
- Hepatomegaly / splenomegaly / hepatosplenomegaly
- Additional findings, such as obturator test, psoas test, McBurney point test, Murphy test
Back
- Back examination of patients with [disease name] is usually normal.
OR
- Point tenderness over __ vertebrae (e.g. L3-L4)
- Sacral edema
- Costovertebral angle tenderness bilaterally/unilaterally
- Buffalo hump
Genitourinary
- Genitourinary examination of patients with [disease name] is usually normal.
OR
- A pelvic/adnexal mass may be palpated
- Inflamed mucosa
- Clear/(color), foul-smelling/odorless penile/vaginal discharge
Neuromuscular
- Neuromuscular examination of patients with pericarditis is usually normal.
OR
- Patient is usually oriented to persons, place, and time
- Altered mental status
- Glasgow coma scale is ___ / 15
- Clonus may be present
- Hyperreflexia / hyporeflexia / areflexia
- Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally
- Muscle rigidity
- Proximal/distal muscle weakness unilaterally/bilaterally
- ____ (finding) suggestive of cranial nerve ___ (roman numerical) deficit (e.g. Dilated pupils suggestive of CN III deficit)
- Unilateral/bilateral upper/lower extremity weakness
- Unilateral/bilateral sensory loss in the upper/lower extremity
- Positive straight leg raise test
- Abnormal gait (describe gait: e.g. ataxic (cerebellar) gait / steppage gait / waddling gait / choeiform gait / Parkinsonian gait / sensory gait)
- Positive/negative Trendelenburg sign
- Unilateral/bilateral tremor (describe tremor, e.g. at rest, pill-rolling)
- Normal finger-to-nose test / Dysmetria
- Absent/present dysdiadochokinesia (palm tapping test)
Extremities
- Extremities examination of patients with pericarditis is usually normal.
Appearance of the Patient
- Fever less than 39°C or 102.2°F
- Patients who are elderly may not exhibit fever; however, they may be hypothermic, especially those with renal failure.
- Chills (suppurative pericarditis and idiopathic viral pericarditis)
- Weakness
- Anxiety
- Pallor (may also indicate tuberculosis, uremia, neoplasia, or rheumatic carditis)
Heart
A pericardial rub or pericardial friction rub is the classic physical examination finding in pericarditis. It is usually heard in the setting of an acute pericarditis, and occasionally with either subacute or chronic pericarditis. It is best heard with the diaphragm of the stethoscope. Inflammation of the pericardial sac causes the parietal and visceral surfaces of the roughened pericardium to rub against each other. This produces an extra cardiac sound of to-and-fro character with both systolic and diastolic components. One, two, or three components of a pericardial friction rub may be audible. A three-component rub indicates the presence of pericarditis and serves to distinguish a pericardial rub from a pleural friction rub, which ordinarily has two components. It resembles the sound of squeaky leather and is often described as grating, scratching, or rasping. The sound may seem louder than or may even mask the other heart sounds. Friction rubs are usually best heard between the apex and sternum but may be widespread. The sound has three components, two diastolic and one systolic.
There are several different pericardial rubs that can be auscultated:
Endopericardial Rub
This rub occurs as the result of inflamed, scarred or tumor-invaded serosal surfaces of pericardium.
Exopericardial Rub
This rub occurs after sclerotherapy of effusions, and is due to friction between the parietal pericardium and the pleura (or occasionally the chest wall).
Endo-exopericardial Rub
This rub occurs with both of the above.
Pleuropericardial Rub
This rub occurs as a result of both pleural and pericardial inflammation.
Signs of Significant Pericardial Effusion or Cardiac Tamponade
Classical cardiac tamponade presents three signs, known as Beck's triad.[1] Beck's triad consists of hypotension due to a decreased stroke volume, jugular venous distension due to impaired venous return to the heart, and muffled heart sounds due to fluid inside the pericardium.[2] Another sign of tamponade on physical examination includes pulsus paradoxus (a drop of at least 10 mmHg in arterial blood pressure on inspiration).[3] There may also be general signs and symptoms of cardiogenic shock (such as tachycardia, breathlessness, poor perfusion of the extremities, and decreasing level of consciousness). Peripheral edema may be present. Hemodynamic changes diminish S1 and S2. As ventricular volume shrinks disproportionately, there may be psuedoprolapse/true prolapse of mitral and/or tricuspid valvular structures that results in clicking sounds.
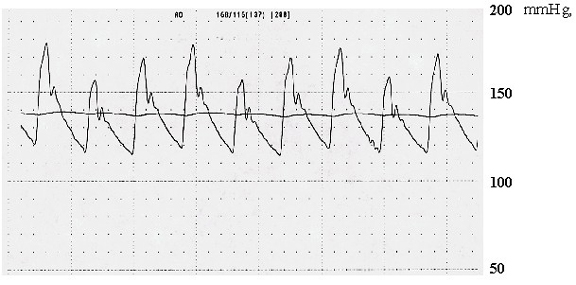
Copyleft image obtained courtesy of Zhi Zhou, MD.
Signs of Pericardial Constriction
- Elevation of the JVP (jugular venous pulse): The waveform of pericardial constriction is characteristic with a prominent 'x' and 'y' descent.
- Kussmaul’s sign: It may be found in about 10% of patients. It occurs because the fall in intrathoracic pressure during inspiration is not transmitted to the cardiac chambers and pericardial space.
- Pulsus paradoxus: Though more typical in cardiac tamponade, it can be seen in 20% of patients with pericardial constriction.
- Widely split S2 and a pericardial knock: They can be present in approximately 50% of patients.
- Pulsatile liver, ascites, and scrotal edema
- Peripheral edema
References
- ↑ Gwinnutt, C., Driscoll, P. (Eds) (2003) (2nd Ed.) Trauma Resuscitation: The Team Approach. Oxford: BIOS Scientific Publishers Ltd. ISBN 978-1859960097
- ↑ Dolan, B., Holt, L. (2000). Accident & Emergency: Theory into practice. London: Bailliere Tindall ISBN 978-0702022395
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886