Pericarditis CT: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
===Advantages of Computed Tomography Over Echocardiography in the Assessment of Pericardial Effusion=== | ===Advantages of Computed Tomography Over Echocardiography in the Assessment of Pericardial Effusion=== | ||
Both MRI and CT have an advantage over echocardiography insofar as they can detect loculated effusions as well as generalized effusions | Both MRI and CT have an advantage over echocardiography insofar as they can detect loculated effusions as well as generalized effusions<ref>Chotas HG, Dobbins JT, Ravin CE (1999) Principles of digital radiography with large-area, electronically readable detectors: a review of the basics. Radiology 210:595-599</ref> <ref>Ohnesorge BM, Becker CR, Flohr TG, Reiser MF (2001) Multislice CT in cardiac imaging. Springer-Verlag</ref>. Computed tomography superior to MRI in the assessment of pericardial calcification. | ||
==Computed Tomography in the Assessment of Constrictive Pericarditis== | ==Computed Tomography in the Assessment of Constrictive Pericarditis== | ||
Revision as of 19:06, 31 July 2011
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis CT On the Web |
|
American Roentgen Ray Society Images of Pericarditis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
On CT image, pericardial fluid adds to the thickness of pericardium as both have the similar signal intensities. In pericarditis, pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration. In pericardial effusion, hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). CT is superior to MRI in the visualization of pericardial calcification which is often seen in the patient with pericardial constriction. CT imaging also helps in detecting the presence of tumors and the extent of metastasis of the neoplasm.
Computed Tomography of the Normal Pericardium
There is normally 15 to 50 mL of fluid in the pericardial sac which may contribute to the apparent thickness of the pericardium since they both have the same signal intensity.
Computed Tomography in the Patient with Pericarditis
In the presence of acute pericarditis, the pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration.
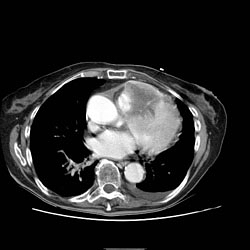
Computed Tomography in the Patient with Pericardial Effusion
If the fluid is free-flowing and not loculated, it will first accumulate at the posterior lateral aspect of the all sleepleft ventricle in the supine position. It can be hard to differentiate a small pericardial effusion from pericardial thickening of about 4 mm Since both entities generate a similar signal. In the presence of acute pericarditis, the pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration.
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion.

Pericardial Effusion as an Incidentoloma on Computed Tomography
A pericardial effusion is often incidentally noted on CT scans obtained for other indications.
Advantages of Computed Tomography Over Echocardiography in the Assessment of Pericardial Effusion
Both MRI and CT have an advantage over echocardiography insofar as they can detect loculated effusions as well as generalized effusions[1] [2]. Computed tomography superior to MRI in the assessment of pericardial calcification.
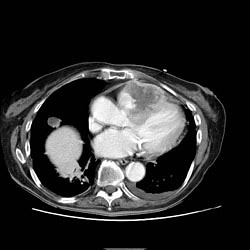
Computed Tomography in the Assessment of Constrictive Pericarditis
The signs of constrictive pericarditis on CT include:
- A thickened perciardium
- Impaired right ventricular function
- There is an abrupt reduction in ventricular filling
- Stroke volume is reduced
- The intraventricular septum curves to the left which may reduce left ventricular filling, stroke volume and cardiac output.
- There may be dilatation of the superior vena cava, the inferior vena cava, the azygous veins and hepatic veins due to elevated back pressures from the right heart.
- Enlargement of the right atrium
- The right ventricle itself may be normal or even reduced in size and may assume a tubular or sigmoid shape due to compression.
- Localized pericardial thickening may also cause functional impairment a condition known as localized constrictive pericarditis.
- Computed tomography is superior to MRI in the visualization of pericardial calcification which is often seen in the patient with pericardial constriction.
Computed Tomography in the Assessment of the Patient with Pericardial Tumor
A pericardial cyst is most commonly located at the right cardiophrenic angle. On T1, it appears either as a low signal or an intermediate signal due to high protein content, or with a characteristic light-bulb appearance on T2.
Unusual tumors may arise from the pericardium (mesothelioma, angiosarcoma, etc.). Malignant primary tumors have many overlapping imaging features and generally cannot be differentiated. The role of cross-sectional imaging is to establish a diagnosis and to define the extent of the lesion (invasion of cardiac structures, veins, pericardium, etc.). Sometimes lesions may have helpful signal characteristics to suggest a specific diagnosis, e.g., high-signal fat on T1 or low-density fat on CT in lipoma / liposarcoma.
Secondary tumors are much more common than primary tumors. Lung cancer may invade the mediastinal and cardiac structures directly or indirectly.
The most common secondary tumors affecting the heart are lung cancer, breast cancer, and lymphoma. Metastatic pericardial disease commonly presents as hemorrhagic effusion. Tumor nodules may enhance after intravenous gadolinium administration.
Computed Tomography in the Assessment of Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases