Pericarditis CT: Difference between revisions
No edit summary |
(Mahshid) |
||
| (17 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Pericarditis}} | {{Pericarditis}} | ||
{{CMG}} | |||
==Overview== | ==Overview== | ||
On CT | On [[CT]], pericardial fluid adds to the thickness of [[pericardium]] as both have the similar signal intensities. In [[pericarditis]], [[pericardium]] can generate an intermediate signal intensity and may enhance after [[gadolinium]] administration. In [[pericardial effusion]], hemorrhagic effusions can be differentiated from a [[transudate]] or an [[exudate]] based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). [[CT]] is superior to [[MRI]] in the visualization of [[pericardial calcification]] which is often seen in the patient with [[pericardial constriction]]. CT imaging also helps in detecting the presence of [[tumor]]s and the extent of [[metastasis]] of the [[neoplasm]]. | ||
== | ==Normal Pericardium on CT== | ||
There is normally 15 to 50 mL of fluid in the [[pericardial sac]] which may contribute to the apparent thickness of the [[pericardium]] since they both have the same signal intensity. | There is normally 15 to 50 mL of fluid in the [[pericardial sac]] which may contribute to the apparent thickness of the [[pericardium]] since they both have the same signal intensity. | ||
== | ==Pericarditis on CT== | ||
In the presence of acute [[pericarditis]], the [[pericardium]] can generate an intermediate signal intensity and may enhance after [[gadolinium]] administration. | In the presence of acute [[pericarditis]], the [[pericardium]] can generate an intermediate signal intensity and may enhance after [[gadolinium]] administration. | ||
== | ==Pericardial Effusion on CT== | ||
If the fluid is free-flowing and not loculated, it will first accumulate at the posterior lateral aspect of the all sleepleft ventricle in the supine position. It can be hard to differentiate a small pericardial effusion from pericardial thickening of about 4 mm | If the fluid is free-flowing and not loculated, it will first accumulate at the posterior lateral aspect of the all sleepleft ventricle in the supine position. It can be hard to differentiate a small [[pericardial effusion]] from pericardial thickening of about 4 mm, since both entities generate a similar signal. In the presence of [[acute pericarditis]], the [[pericardium]] can generate an intermediate signal intensity and may enhance after [[gadolinium]] administration. | ||
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion. | Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Hemorrhagic effusions can be differentiated from a [[transudate]] or an [[exudate]] based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion. | ||
[http://www.radswiki.net Images courtesy of RadsWiki] | [http://www.radswiki.net Images courtesy of RadsWiki] | ||
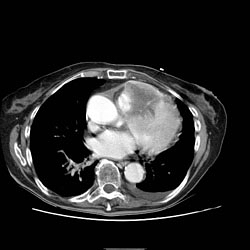
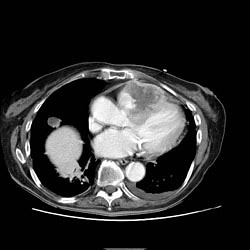
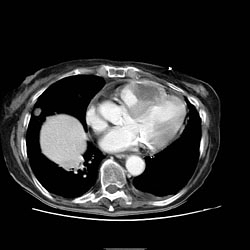
[[Image:Pericard-effusion-03.jpg|left|thumb|350px|Cardiac MSCT: Pericardial effusion]] | [[Image:Pericard-effusion-03.jpg|left|thumb|350px|Cardiac MSCT: Pericardial effusion]] | ||
<br clear="left"/> | <br clear="left"/> | ||
===Pericardial Effusion as an Incidentoloma on | ===Pericardial Effusion as an Incidentoloma on CT=== | ||
A pericardial effusion is often incidentally noted on CT scans obtained for other indications. | A [[pericardial effusion]] is often incidentally noted on [[CT]] scans obtained for other indications. | ||
===Advantages of CT over Echocardiography in the Assessment of Pericardial Effusion=== | |||
Both [[MRI]] and [[CT]] have an advantage over [[echocardiography]] insofar as they can detect loculated effusions as well as generalized effusions.<ref>Chotas HG, Dobbins JT, Ravin CE (1999) Principles of digital radiography with large-area, electronically readable detectors: a review of the basics. Radiology 210:595-599</ref><ref>Ohnesorge BM, Becker CR, Flohr TG, Reiser MF (2001) Multislice CT in cardiac imaging. Springer-Verlag</ref> [[CT]] is superior to [[MRI]] in the assessment of [[pericardial calcification]]. | |||
== | ==Constrictive Pericarditis on CT== | ||
The signs of [[constrictive pericarditis]] on CT include: | |||
*Thickened [[pericardium]] | |||
The signs of constrictive pericarditis on CT include: | |||
* | |||
*Impaired [[right ventricular]] function | *Impaired [[right ventricular]] function | ||
* | *Abrupt reduction in ventricular filling | ||
*[[ | *Reduced [[stroke volume]] | ||
* | *Curving of [[intraventricular septum]] to the left which may reduce left ventricular filling, [[stroke volume]] and [[cardiac output]]. | ||
* | *Dilatation of the [[superior vena cava]], the [[inferior vena cava]], the [[azygous veins]] and [[hepatic veins]] due to elevated back pressures from the right heart. | ||
*Enlargement of the [[right atrium]] | *Enlargement of the [[right atrium]] | ||
*The [[right ventricle]] itself may be normal or even reduced in size and may assume a tubular or sigmoid shape due to compression. | *The [[right ventricle]] itself may be normal or even reduced in size and may assume a tubular or sigmoid shape due to compression. | ||
*Localized pericardial thickening may also cause functional impairment a condition known as localized constrictive pericarditis. | *Localized pericardial thickening may also cause functional impairment, a condition known as localized constrictive pericarditis. | ||
* | *[[CT]] is superior to [[MRI]] in the visualization of [[pericardial calcification]] which is often seen in the patient with [[pericardial constriction]]. | ||
==Pericardial Tumor on CT== | |||
A pericardial cyst is most commonly located at the right cardiophrenic angle. On T1, it appears either as a low signal or an intermediate signal due to high [[protein]] content, or with a characteristic ''light-bulb'' appearance on T2. | |||
The | There are several rare tumors that may arise within the pericardium including [[mesothelioma]] and [[angiosarcoma]]. Malignant primary tumors have many overlapping imaging features and generally cannot be differentiated from one another. The role of cross-sectional imaging is to establish a diagnosis and to define the extent of the lesion (invasion of cardiac structures, veins, pericardium, etc.). Sometimes lesions may have helpful signal characteristics to suggest a specific diagnosis, e.g., high-signal fat on T1 or low-density fat on [[CT]] in [[lipoma]] or [[liposarcoma]]. | ||
== | ==Pericardial Metastases on CT== | ||
Secondary tumors are much more common than primary tumors. [[Lung cancer]] may invade the mediastinal and cardiac structures directly or indirectly. The most common secondary tumors affecting the heart are: | |||
*[[Lung cancer]] | |||
*[[Breast cancer]] | |||
*[[Lymphoma]]<br> | |||
Metastatic pericardial disease commonly presents as hemorrhagic effusion. Tumor nodules may enhance after intravenous [[gadolinium]] administration. | |||
[http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
| Line 63: | Line 61: | ||
</gallery> | </gallery> | ||
<br clear="left"/> | <br clear="left"/> | ||
==Limitations of CT== | |||
*Need for contrast administration. | |||
*Exposure to ionizing [[radiation]]. | |||
*Difficulty in differentiating fluid from thickened pericardium. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
[[ | [[Category:Radiology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:CT]] | [[Category:CT]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Disease]] | |||
[[Category:Best pages]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Cardiology]] | |||
[[Category:Surgery]] | |||
Latest revision as of 15:05, 27 November 2017
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Pericarditis CT On the Web |
|
American Roentgen Ray Society Images of Pericarditis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
On CT, pericardial fluid adds to the thickness of pericardium as both have the similar signal intensities. In pericarditis, pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration. In pericardial effusion, hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). CT is superior to MRI in the visualization of pericardial calcification which is often seen in the patient with pericardial constriction. CT imaging also helps in detecting the presence of tumors and the extent of metastasis of the neoplasm.
Normal Pericardium on CT
There is normally 15 to 50 mL of fluid in the pericardial sac which may contribute to the apparent thickness of the pericardium since they both have the same signal intensity.
Pericarditis on CT
In the presence of acute pericarditis, the pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration.
Pericardial Effusion on CT
If the fluid is free-flowing and not loculated, it will first accumulate at the posterior lateral aspect of the all sleepleft ventricle in the supine position. It can be hard to differentiate a small pericardial effusion from pericardial thickening of about 4 mm, since both entities generate a similar signal. In the presence of acute pericarditis, the pericardium can generate an intermediate signal intensity and may enhance after gadolinium administration.
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion.

Pericardial Effusion as an Incidentoloma on CT
A pericardial effusion is often incidentally noted on CT scans obtained for other indications.
Advantages of CT over Echocardiography in the Assessment of Pericardial Effusion
Both MRI and CT have an advantage over echocardiography insofar as they can detect loculated effusions as well as generalized effusions.[1][2] CT is superior to MRI in the assessment of pericardial calcification.
Constrictive Pericarditis on CT
The signs of constrictive pericarditis on CT include:
- Thickened pericardium
- Impaired right ventricular function
- Abrupt reduction in ventricular filling
- Reduced stroke volume
- Curving of intraventricular septum to the left which may reduce left ventricular filling, stroke volume and cardiac output.
- Dilatation of the superior vena cava, the inferior vena cava, the azygous veins and hepatic veins due to elevated back pressures from the right heart.
- Enlargement of the right atrium
- The right ventricle itself may be normal or even reduced in size and may assume a tubular or sigmoid shape due to compression.
- Localized pericardial thickening may also cause functional impairment, a condition known as localized constrictive pericarditis.
- CT is superior to MRI in the visualization of pericardial calcification which is often seen in the patient with pericardial constriction.
Pericardial Tumor on CT
A pericardial cyst is most commonly located at the right cardiophrenic angle. On T1, it appears either as a low signal or an intermediate signal due to high protein content, or with a characteristic light-bulb appearance on T2.
There are several rare tumors that may arise within the pericardium including mesothelioma and angiosarcoma. Malignant primary tumors have many overlapping imaging features and generally cannot be differentiated from one another. The role of cross-sectional imaging is to establish a diagnosis and to define the extent of the lesion (invasion of cardiac structures, veins, pericardium, etc.). Sometimes lesions may have helpful signal characteristics to suggest a specific diagnosis, e.g., high-signal fat on T1 or low-density fat on CT in lipoma or liposarcoma.
Pericardial Metastases on CT
Secondary tumors are much more common than primary tumors. Lung cancer may invade the mediastinal and cardiac structures directly or indirectly. The most common secondary tumors affecting the heart are:
Metastatic pericardial disease commonly presents as hemorrhagic effusion. Tumor nodules may enhance after intravenous gadolinium administration.
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
-
Pericardial Metastases
Limitations of CT
- Need for contrast administration.
- Exposure to ionizing radiation.
- Difficulty in differentiating fluid from thickened pericardium.