Osteoporosis natural history, complications and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Osteoporosis]] can | With appropriate and timely usage of [[medications]] along with [[calcium]] and/or [[vitamin D]] supplementation, the outcome of [[osteoporosis]] is usually good. The only way, through which [[Osteoporosis]] can become complicated, is by the development of [[fractures]]. Apart from risk of death and other complications, osteoporotic [[fractures]] are associated with a reduced [[quality of life]] due to [[immobility]]; [[emotional]] problems may also raised as a consequence. As studies suggested, the impact of [[osteoporosis]] and also osteoporotic [[fractures]] on public life would be worse than lots of life threatening diseases; especially with aging. | ||
{| align="right" | {| align="right" | ||
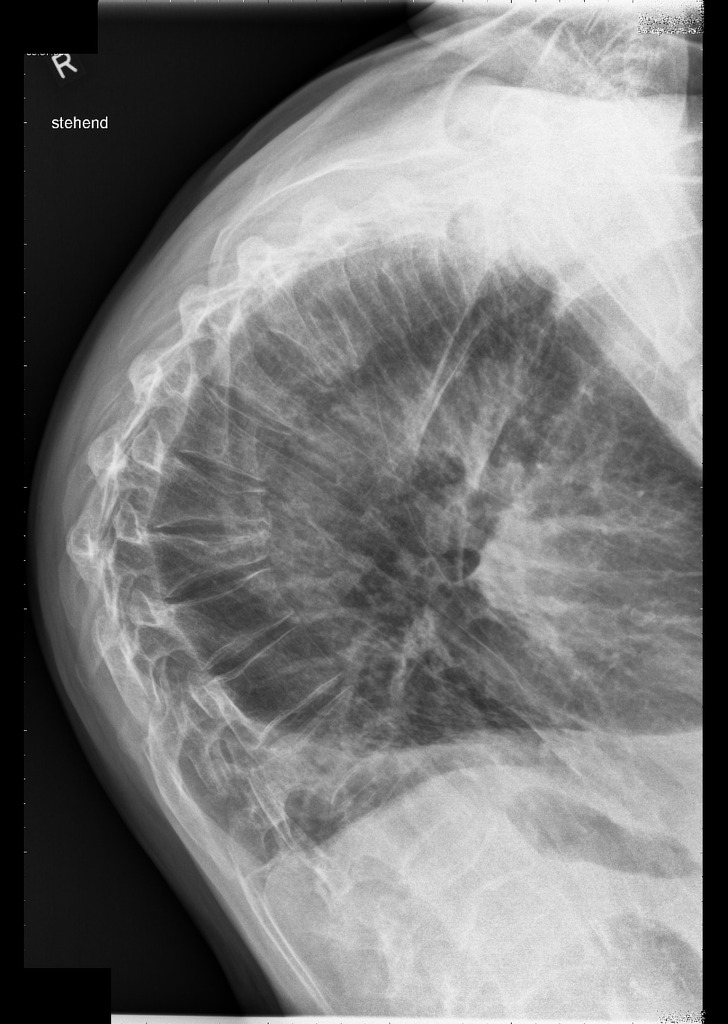
| [[Image:Vertebral-insufficiency-fractures-in-severe-osteoporosis.jpg|200px|thumb | | [[Image:Vertebral-insufficiency-fractures-in-severe-osteoporosis.jpg|200px|thumb| Radiopaedia.org">{{cite web |url=https://radiopaedia.org/cases/vertebral-insufficiency-fractures-in-severe-osteoporosis |title=Vertebral insufficiency fractures in severe osteoporosis | Radiology Case | Radiopaedia.org |format= |work= |accessdate=}}<nowiki></ref></nowiki>]] | ||
|-| | |- | | ||
| [[Image:Vertebral-insufficiency-fractures-in-severe-osteoporosis(4).jpg|200px|thumb | | [[Image:Vertebral-insufficiency-fractures-in-severe-osteoporosis(4).jpg|200px|thumb| Radiopaedia.org">{{cite web |url=https://radiopaedia.org/cases/vertebral-insufficiency-fractures-in-severe-osteoporosis |title=Vertebral insufficiency fractures in severe osteoporosis | Radiology Case | Radiopaedia.org |format= |work= |accessdate=}}<nowiki></ref></nowiki>]] | ||
|-| | |- | | ||
| [[Image:Efdfc0355363446eac868f3bf93ea0 jumbo.jpeg|200px|thumb | | [[Image:Efdfc0355363446eac868f3bf93ea0 jumbo.jpeg|200px|thumb| Radiopaedia.org">{{cite web |url=https://radiopaedia.org/cases/dowagers-hump |title=Dowager's hump | Radiology Case | Radiopaedia.org |format= |work= |accessdate=}}<nowiki></ref></nowiki>]] | ||
|} | |} | ||
==Natural history== | ==Natural history== | ||
* Typically, symptoms of [[osteoporosis]] are developed in the sixth decade of life. The risk of getting [[osteoporosis]] is increased proportionately with age. | * Typically, symptoms of [[osteoporosis]] are developed in the sixth decade of life. The risk of getting [[osteoporosis]] is increased proportionately with age. | ||
* Researchers have shown that relationship between lowering bone density of spine and age is not linear, but quadratic; in which bone loss tailing off when age raised. During the first years of post-menopausal period, women would have a fast decrease in bone density of spine by rate of 3.12% annually; then the rate slowed down to 0.02% per square age increased.<ref name="pmid18305885">{{cite journal| author=Zhai G, Hart DJ, Valdes AM, Kato BS, Richards JB, Hakim A et al.| title=Natural history and risk factors for bone loss in postmenopausal Caucasian women: a 15-year follow-up population-based study. | journal=Osteoporos Int | year= 2008 | volume= 19 | issue= 8 | pages= 1211-7 | pmid=18305885 | doi=10.1007/s00198-008-0562-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18305885 }}</ref> | * Researchers have shown that relationship between lowering [[bone density]] of [[Spine (journal)|spine]] and age is not linear, but quadratic; in which bone loss tailing off when age raised. During the first years of [[Postmenopausal|post-menopausal]] period, women would have a fast decrease in [[bone]] density of [[spine]] by rate of 3.12% annually; then the rate slowed down to 0.02% per square age increased.<ref name="pmid18305885">{{cite journal| author=Zhai G, Hart DJ, Valdes AM, Kato BS, Richards JB, Hakim A et al.| title=Natural history and risk factors for bone loss in postmenopausal Caucasian women: a 15-year follow-up population-based study. | journal=Osteoporos Int | year= 2008 | volume= 19 | issue= 8 | pages= 1211-7 | pmid=18305885 | doi=10.1007/s00198-008-0562-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18305885 }}</ref> | ||
* However, Guthrie also mentioned that in first 3 years after menopause, the rate of decreasing bone density increased annually; then with years past from menopause, the rate of bone loss will slow down.<ref name="pmid9797914">{{cite journal |vauthors=Guthrie JR, Ebeling PR, Hopper JL, Barrett-Connor E, Dennerstein L, Dudley EC, Burger HG, Wark JD |title=A prospective study of bone loss in menopausal Australian-born women |journal=Osteoporos Int |volume=8 |issue=3 |pages=282–90 |year=1998 |pmid=9797914 |doi=10.1007/s001980050066 |url=}}</ref> | * However, Guthrie also mentioned that in first 3 years after [[menopause]], the rate of decreasing [[bone density]] increased annually; then with years past from [[menopause]], the rate of bone loss will slow down.<ref name="pmid9797914">{{cite journal |vauthors=Guthrie JR, Ebeling PR, Hopper JL, Barrett-Connor E, Dennerstein L, Dudley EC, Burger HG, Wark JD |title=A prospective study of bone loss in menopausal Australian-born women |journal=Osteoporos Int |volume=8 |issue=3 |pages=282–90 |year=1998 |pmid=9797914 |doi=10.1007/s001980050066 |url=}}</ref> | ||
* One another major factor that directly impact on changing BMD is body weight; women with heavier weight and also higher body mass index (BMI) may have more change in their BMD in both hip and lumbar spine, during the time. | * One another major factor that directly impact on changing [[Bone mineral density|BMD]] is [[body weight]]; women with heavier weight and also higher [[Body mass index|body mass index (BMI)]] may have more change in their [[Bone mineral density|BMD]] in both hip and lumbar spine, during the time. | ||
* Surprisingly, the bone site is an important factor to determine the measure of bone loss. The studies have found that magnitude of bone density loss is higher at spine (-3.12% annually) compared to femoral neck (1.67% annually). The main proposed theory for the phenomenon is "different effect of estrogen deficiency on different bone sites". On the other hand it may show the preventive effect of weight bearing on hip osteoporosis.<ref name="pmid18305885" /> | * Surprisingly, the [[bone]] site is an important factor to determine the measure of [[bone]] loss. The studies have found that magnitude of [[bone density]] loss is higher at spine (-3.12% annually) compared to [[femoral neck]] (1.67% annually). The main proposed theory for the phenomenon is "different effect of [[estrogen]] deficiency on different [[bone]] sites". On the other hand, it may show the preventive effect of weight bearing on [[hip]] [[osteoporosis]].<ref name="pmid18305885" /> | ||
* With appropriate and timely usage of medications along with [[calcium]] and/or [[vitamin D]] supplementation, the outcome of osteoporosis is usually good. But if the disease left untreated, or not favorably treated, the clinical consequence would be fracture and the morbidity that happen thereafter. The main type of fracture that influence the quality of life more and happened earlier, is vertebral fracture.<ref name="pmid9102060">{{cite journal |vauthors=Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Liberman U, Minne H, Reeve J, Reginster JY, de Vernejoul MC, Wiklund I |title=Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis |journal=Osteoporos Int |volume=7 |issue=1 |pages=36–8 |year=1997 |pmid=9102060 |doi= |url=}}</ref> | * With appropriate and timely usage of [[medications]] along with [[calcium]] and/or [[vitamin D]] supplementation, the outcome of [[osteoporosis]] is usually good. But if the disease left untreated, or not favorably treated, the clinical consequence would be [[Fractures|fracture]] and the [[morbidity]] that happen thereafter. The main type of [[fracture]] that influence the [[quality of life]] more and happened earlier, is [[vertebral]] [[fracture]].<ref name="pmid9102060">{{cite journal |vauthors=Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Liberman U, Minne H, Reeve J, Reginster JY, de Vernejoul MC, Wiklund I |title=Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis |journal=Osteoporos Int |volume=7 |issue=1 |pages=36–8 |year=1997 |pmid=9102060 |doi= |url=}}</ref> | ||
==Complications== | ==Complications== | ||
* The major probable complications of osteoporosis include: | * The major probable complications of [[osteoporosis]] include: | ||
** [[Fractures]]: hip and lumbar spine are among the most frequent sites of fracture. | ** [[Fractures]]: [[hip]] and [[lumbar]] spine are among the most frequent sites of [[fracture]]. | ||
** [[DVT|Deep venous thrombosis (DVT)]]: it can be caused by prolonged immobility. | ** [[DVT|Deep venous thrombosis (DVT)]]: it can be caused by prolonged [[immobility]]. | ||
** [[Kyphosis]] (Dowager's hump): the main reason could be decreasing the height of anterior aspect of cervical vertebrae body (wedge shape). | ** [[Kyphosis]] (Dowager's hump): the main reason could be decreasing the height of anterior aspect of [[cervical]] [[vertebrae]] body (wedge shape). | ||
** [[Restrictive lung disease]]: because of decreasing thoracic space, due to vertebrae body compression. | ** [[Restrictive lung disease]]: because of decreasing [[thoracic]] space, due to [[vertebrae]] body compression. | ||
* Apart from risk of death and other complications, osteoporotic fractures are associated with a reduced quality of life due to immobility; emotional problems may also | * Apart from risk of death and other complications, osteoporotic [[Bone fracture|fractures]] are associated with a reduced [[quality of life]] due to [[immobility]]; emotional problems may also raised as a consequence.<ref>{{cite journal |author=Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES |title=Impact of recent fracture on health-related quality of life in postmenopausal women |journal=J. Bone Miner. Res. |volume=21 |issue=6 |pages=809–16 |year=2006 |pmid=16753011 |doi=10.1359/jbmr.060301}}</ref> | ||
==Prognosis== | ==Prognosis== | ||
* If the bone mass density loss is identified early and the appropriate medicine begin as soon as possible, the prognosis of osteoporosis would be good. | * If the [[Bone mineral density|bone mass density]] loss is identified early and the appropriate medicine begin as soon as possible, the prognosis of [[osteoporosis]] would be good. | ||
* The most important issue to identify the osteoporosis prognosis is fractures; mainly affected by two factors include advancing age and low BMD. The relation is consist of having about 2-fold increase in risk of various fractures following every SD lowering of BMD or 5 years age advance.<ref name="pmid8093403">{{cite journal |vauthors=Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM |title=Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group |journal=Lancet |volume=341 |issue=8837 |pages=72–5 |year=1993 |pmid=8093403 |doi= |url=}}</ref> | * The most important issue to identify the [[osteoporosis]] prognosis is [[Bone fracture|fractures]]; mainly affected by two factors include advancing age and low [[Bone mineral density|BMD]]. The relation is consist of having about 2-fold increase in risk of various [[fractures]] following every SD lowering of [[Bone mineral density|BMD]] or 5 years age advance.<ref name="pmid8093403">{{cite journal |vauthors=Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM |title=Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group |journal=Lancet |volume=341 |issue=8837 |pages=72–5 |year=1993 |pmid=8093403 |doi= |url=}}</ref> | ||
* When the fracture risk of lifetime at age 60 become adjusted upon death rate, it may be 44% for woman and 25% for men. The lifetime fracture risk for hip is 9% in women and 4% in men. The researchers suggest that lifetime fracture risk of hip in 60 years old women is 1 in 7 (15%); which is higher than estimated lifetime risk of breast cancer (9.3%). Similarly, fracture risk of hip and vertebrae in men (15%) is totally noticeable along with their prostate cancer risk. This means that the impact of osteoporosis and also osteoporotic fractures on public life would be worse than lots of life threatening diseases; especially with aging.<ref name="pmid17352657">{{cite journal| author=Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV| title=Residual lifetime risk of fractures in women and men. | journal=J Bone Miner Res | year= 2007 | volume= 22 | issue= 6 | pages= 781-8 | pmid=17352657 | doi=10.1359/jbmr.070315 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17352657 }}</ref> | * When the [[Bone fracture|fracture]] risk of lifetime at age 60 become adjusted upon death rate, it may be 44% for woman and 25% for men. The lifetime [[fracture]] risk for hip is 9% in women and 4% in men. The researchers suggest that lifetime [[fracture]] risk of [[hip]] in 60 years old women is 1 in 7 (15%); which is higher than estimated lifetime risk of [[breast cancer]] (9.3%). Similarly, [[fracture]] risk of [[hip]] and [[vertebrae]] in men (15%) is totally noticeable along with their [[prostate cancer]] risk. This means that the impact of [[osteoporosis]] and also osteoporotic [[fractures]] on public life would be worse than lots of life threatening [[diseases]]; especially with aging.<ref name="pmid17352657">{{cite journal| author=Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV| title=Residual lifetime risk of fractures in women and men. | journal=J Bone Miner Res | year= 2007 | volume= 22 | issue= 6 | pages= 781-8 | pmid=17352657 | doi=10.1359/jbmr.070315 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17352657 }}</ref> | ||
==References== | ==References== | ||
Revision as of 21:39, 3 August 2017
|
Osteoporosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Osteoporosis natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Osteoporosis natural history, complications and prognosis |
|
FDA on Osteoporosis natural history, complications and prognosis |
|
CDC on Osteoporosis natural history, complications and prognosis |
|
Osteoporosis natural history, complications and prognosis in the news |
|
Blogs on Osteoporosis natural history, complications and prognosis |
|
Risk calculators and risk factors for Osteoporosis natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Overview
With appropriate and timely usage of medications along with calcium and/or vitamin D supplementation, the outcome of osteoporosis is usually good. The only way, through which Osteoporosis can become complicated, is by the development of fractures. Apart from risk of death and other complications, osteoporotic fractures are associated with a reduced quality of life due to immobility; emotional problems may also raised as a consequence. As studies suggested, the impact of osteoporosis and also osteoporotic fractures on public life would be worse than lots of life threatening diseases; especially with aging.
 |
 |
 |
Natural history
- Typically, symptoms of osteoporosis are developed in the sixth decade of life. The risk of getting osteoporosis is increased proportionately with age.
- Researchers have shown that relationship between lowering bone density of spine and age is not linear, but quadratic; in which bone loss tailing off when age raised. During the first years of post-menopausal period, women would have a fast decrease in bone density of spine by rate of 3.12% annually; then the rate slowed down to 0.02% per square age increased.[1]
- However, Guthrie also mentioned that in first 3 years after menopause, the rate of decreasing bone density increased annually; then with years past from menopause, the rate of bone loss will slow down.[2]
- One another major factor that directly impact on changing BMD is body weight; women with heavier weight and also higher body mass index (BMI) may have more change in their BMD in both hip and lumbar spine, during the time.
- Surprisingly, the bone site is an important factor to determine the measure of bone loss. The studies have found that magnitude of bone density loss is higher at spine (-3.12% annually) compared to femoral neck (1.67% annually). The main proposed theory for the phenomenon is "different effect of estrogen deficiency on different bone sites". On the other hand, it may show the preventive effect of weight bearing on hip osteoporosis.[1]
- With appropriate and timely usage of medications along with calcium and/or vitamin D supplementation, the outcome of osteoporosis is usually good. But if the disease left untreated, or not favorably treated, the clinical consequence would be fracture and the morbidity that happen thereafter. The main type of fracture that influence the quality of life more and happened earlier, is vertebral fracture.[3]
Complications
- The major probable complications of osteoporosis include:
- Fractures: hip and lumbar spine are among the most frequent sites of fracture.
- Deep venous thrombosis (DVT): it can be caused by prolonged immobility.
- Kyphosis (Dowager's hump): the main reason could be decreasing the height of anterior aspect of cervical vertebrae body (wedge shape).
- Restrictive lung disease: because of decreasing thoracic space, due to vertebrae body compression.
- Apart from risk of death and other complications, osteoporotic fractures are associated with a reduced quality of life due to immobility; emotional problems may also raised as a consequence.[4]
Prognosis
- If the bone mass density loss is identified early and the appropriate medicine begin as soon as possible, the prognosis of osteoporosis would be good.
- The most important issue to identify the osteoporosis prognosis is fractures; mainly affected by two factors include advancing age and low BMD. The relation is consist of having about 2-fold increase in risk of various fractures following every SD lowering of BMD or 5 years age advance.[5]
- When the fracture risk of lifetime at age 60 become adjusted upon death rate, it may be 44% for woman and 25% for men. The lifetime fracture risk for hip is 9% in women and 4% in men. The researchers suggest that lifetime fracture risk of hip in 60 years old women is 1 in 7 (15%); which is higher than estimated lifetime risk of breast cancer (9.3%). Similarly, fracture risk of hip and vertebrae in men (15%) is totally noticeable along with their prostate cancer risk. This means that the impact of osteoporosis and also osteoporotic fractures on public life would be worse than lots of life threatening diseases; especially with aging.[6]
References
- ↑ 1.0 1.1 Zhai G, Hart DJ, Valdes AM, Kato BS, Richards JB, Hakim A; et al. (2008). "Natural history and risk factors for bone loss in postmenopausal Caucasian women: a 15-year follow-up population-based study". Osteoporos Int. 19 (8): 1211–7. doi:10.1007/s00198-008-0562-x. PMID 18305885.
- ↑ Guthrie JR, Ebeling PR, Hopper JL, Barrett-Connor E, Dennerstein L, Dudley EC, Burger HG, Wark JD (1998). "A prospective study of bone loss in menopausal Australian-born women". Osteoporos Int. 8 (3): 282–90. doi:10.1007/s001980050066. PMID 9797914.
- ↑ Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, Kanis JA, Liberman U, Minne H, Reeve J, Reginster JY, de Vernejoul MC, Wiklund I (1997). "Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis". Osteoporos Int. 7 (1): 36–8. PMID 9102060.
- ↑ Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006). "Impact of recent fracture on health-related quality of life in postmenopausal women". J. Bone Miner. Res. 21 (6): 809–16. doi:10.1359/jbmr.060301. PMID 16753011.
- ↑ Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM (1993). "Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group". Lancet. 341 (8837): 72–5. PMID 8093403.
- ↑ Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV (2007). "Residual lifetime risk of fractures in women and men". J Bone Miner Res. 22 (6): 781–8. doi:10.1359/jbmr.070315. PMID 17352657.