Li-Fraumeni syndrome
| Li-Fraumeni syndrome | |
| ICD-9 | 758.3 |
|---|---|
| OMIM | 151623 |
| DiseasesDB | 7450 |
| eMedicine | ped/1305 |
| MeSH | D016864 |
Li-Fraumeni syndrome is a rare autosomal dominant hereditary disorder. It is named after Frederick Pei Li and Joseph F. Fraumeni, American physicians who originally described the syndrome. It increases greatly the susceptibility to cancer. The syndrome is a mutation in the p53 tumor suppressor gene, which normally helps control cell growth.
Tumor types
The classic tumors that have been seen in Li-Fraumeni syndrome are:
- Breast cancer
- osteosarcoma
- Soft tissue sarcoma
- Adrenal cortical tumors
- Leukemia
- Astrocytoma
- Meningioma
Other malignancies that have been associated with the syndrome include:
- Gastric cancer
- Pharyngeal cancer
- Choroid plexus carcinoma
- Pancreatic Cancer
- Melanoma
- Germ cell tumors
- Wilm's tumor
- Colorectal Cancer
- Phyllodes tumor
- Ovarian Cancer
- Thyroid Cancer
- Endometrial cancer
- Prostate cancer
- Cervical cancer
Characteristics
What makes Li-Fraumeni Syndrome unusual is that
- several kinds of cancer are involved,
- cancer often strikes at a young age, and
- cancer often strikes several times throughout the life of an affected person.
DIfferentiating Li-Fraumeni syndrome from other diseases
| Disease | Gene | Chromosome | Differentiating Features | Components of MEN | Diagnosis | ||
|---|---|---|---|---|---|---|---|
| Parathyroid | Pitutary | Pancreas | |||||
| von Hippel-Lindau syndrome | Von Hippel–Lindau tumor suppressor | 3p25.3 |
|
- | - | + |
|
| Carney complex | PRKAR1A | 17q23-q24 |
|
- | - | - |
|
| Neurofibromatosis type 1 | RAS | 17 | - | - | - | Prenatal
Postnatal Cardinal Clinical Features" are required for positive diagnosis.
| |
| Li-Fraumeni syndrome | TP53 | 17 | Early onset of diverse amount of cancers such as | - | - | - |
Criteria
|
| Gardner's syndrome | APC | 5q21 |
|
- | - | - |
|
| Multiple endocrine neoplasia type 2 | RET | - |
|
+ | - | - |
Criteria Two or more specific endocrine tumors
|
| Cowden syndrome | PTEN | - | Hamartomas | - | - | - |
|
| Acromegaly/gigantism | - | - |
|
- | + | - |
|
| Pituitary adenoma | - | - |
|
- | + | - |
|
| Hyperparathyroidism | - | - | - | + | - | - |
|
| Pheochromocytoma/paraganglioma |
VHL RET NF1 SDHB SDHD |
- | Characterized by | - | - | - |
|
| Adrenocortical carcinoma |
|
17p, 13q |
|
- | - | - |
|
| Adapted from Toledo SP, Lourenço DM, Toledo RA. A differential diagnosis of inherited endocrine tumors and their tumor counterparts, journal=Clinics (Sao Paulo), volume= 68, issue= 7, 07/24/2013[1] | |||||||
Diagnosis and treatment
Li-Fraumeni Syndrome is diagnosed if the following three criteria are met:
- the patient has been diagnosed with a sarcoma at a young age (below 45),
- a first-degree relative has been diagnosed with any cancer at a young age (below 45),
- and another first-degree or a second-degree relative has been diagnosed with any cancer at a young age (below 45) or with a sarcoma at any age.
Genetic counseling and genetic testing are used to confirm that somebody has this gene mutation. Once such a person is identified, early and regular screenings for cancer are recommended for him or her. If caught early the cancers can often be successfully treated. Unfortunately, people with Li-Fraumeni are likely to develop another primary malignancy at a future time.
Genetic etiology
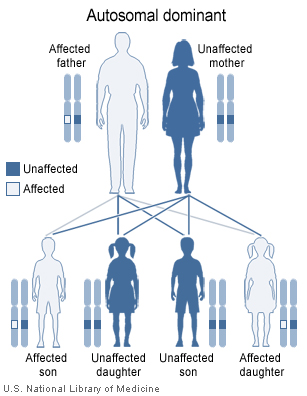
Li-Fraumeni Syndrome is caused by mutations in p53, a tumor suppressor gene. Sufferers inherit one defective copy of the p53 gene retaining one normal copy. This significantly increases the chance that a carrier of a defective gene will develop cancer. This tendency is described in Knudson's two-hit hypothesis, originally devised to explain the incidence of tumours in retinoblastoma patients. In this model, usually in a healthy individual, two spontaneous mutation events must occur in the same gene (such as p53), in the same cell, for cancer to develop. If, however, one defective copy is inherited, only one further mutational event is required to 'knock out' normal p53 function. It is this feature that results in the early age of tumour development and the persistent recurrence of further tumours that are not produced through metastasis, this being a common feature of all the cancer syndromes. Loss of function mutations in a tumor suppressor gene act in a recessive manner, meaning that a mutation for each allele must occur so that the function of that gene is eliminated. For tumor suppressors related cancers, individuals unusually inherit one mutant copy of the p53 tumor suppressor gene and the second mutation occurs sometime during life in a target cell. A clone of cells derived from the target cell can lead to tumor formation. The likelihood that the second mutation will occur is very high, so, as indicated by many pedigree analyses of families with Li-Fraumeni syndrome, there appears to be an autosomal dominant inheritance pattern.
p53 is a transcription factor that tetramerizes before binding to DNA to transactivate genes involved in inducing, cell cycle arrest, and apoptosis. In most cases, individuals with Li-Fraumeni Syndrome have p53 mutations within the DNA-binding domain. p53 is activated by ATM and ATR.
Reference
- Li FP, Fraumeni Jr JF. Soft-tissue sarcomas, breast cancer and other neoplasms: a familial syndrome? Ann Intern Med 1969;71:747-52. PMID 5360287.
External links
- li-fraumeni at NIH/UW GeneTests
de:Li-Fraumeni-Syndrom et:Li-Fraumeni sündroom
Template:WikiDoc Sources
Template:Jb1
- ↑ Toledo SP, Lourenço DM, Toledo RA (2013). "A differential diagnosis of inherited endocrine tumors and their tumor counterparts". Clinics (Sao Paulo). 68 (7): 1039–56. doi:10.6061/clinics/2013(07)24. PMC 3715026. PMID 23917672.