|
|
| (36 intermediate revisions by 9 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = Hypoplastic left heart syndrome | | | Name = Hypoplastic left heart syndrome | |
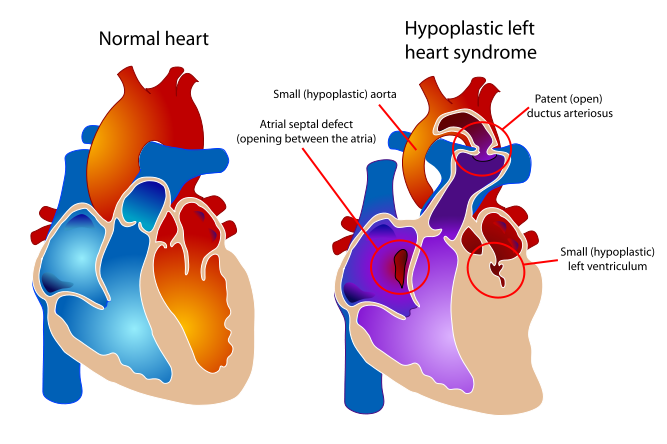
| Image = Hypoplastic left heart syndrome.svg | | | Image = Hypoplastic left heart syndrome.svg | |
| Caption = Diagram of a healthy heart and one suffering from Hypoplastic left heart syndrome | | | Caption = Diagram of a healthy heart and one suffering from Hypoplastic left heart syndrome | |
| Width = 248 |
| |
| DiseasesDB = 31507 |
| |
| ICD10 = {{ICD10|Q|23|4|q|20}} |
| |
| ICD9 = {{ICD9|746.7}} |
| |
| ICDO = |
| |
| OMIM = 241550 |
| |
| MedlinePlus = 001106 |
| |
| eMedicineSubj = ped |
| |
| eMedicineTopic = 1131 |
| |
| MeshName = Hypoplastic+Left+Heart+Syndrome |
| |
| MeshNumber = C14.240.400.625 |
| |
| }} | | }} |
| {{Search infobox}} | | {{Hypoplastic left heart syndrome}} |
| {{CMG}}
| | '''For patient information click [[Hypoplastic left heart syndrome (patient information)|here]]''' |
|
| |
|
| '''Associate Editors-In-Chief:''' {{CZ}}; [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu] | | {{CMG}}; '''Associate Editor(s)-In-Chief:''' [[Priyamvada Singh|Priyamvada Singh, M.B.B.S.]][mailto:psingh13579@gmail.com], {{CZ}}, [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu]; '''Assistant Editor(s)-In-Chief:''' [[Kristin Feeney|Kristin Feeney, B.S.]][mailto:kfeeney@elon.edu] |
|
| |
|
| {{Editor Join}} | | {{SK}} HLHS |
|
| |
|
| ==Overview== | | ==[[Hypoplastic left heart syndrome overview|Overview]]== |
|
| |
|
| [[Hypoplastic left heart syndrome]] (also known as HLHS), is a rare [[congenital heart defect]] in which the left side of the [[heart]] is severely underdeveloped. In babies with HLHS, the [[aorta]] and [[left ventricle]] are very small, and the [[aortic valve|aortic]] and [[mitral valve]]s are either too small to allow sufficient blood flow or are atretic (closed) altogether. As [[blood]] returns from the [[lung]]s to the [[left atrium]], it must pass through an [[atrial septal defect]] to the right side of the heart. | | ==[[Hypoplastic left heart syndrome historical perspective|Historical Perspective]]== |
|
| |
|
| ==Etiology== | | ==[[Hypoplastic left heart syndrome pathophysiology|Pathophysiology]]== |
|
| |
|
| While many authorities believe the cause of HLHS is unknown,<ref name="titleHypoplastic Left Heart Syndrome Causes - Mayo Clinic">{{cite web |url=http://www.mayoclinic.org/hlhs/causes.html |title=Hypoplastic Left Heart Syndrome Causes - Mayo Clinic |accessdate=2008-01-09 |format= |work=}}</ref>
| | ==[[Hypoplastic left heart syndrome causes|Causes]]== |
| <ref>{{eMedicine|ped|1131|Hypoplastic Left Heart Syndrome : Article by P Syamasundar Rao, MD}}</ref><ref>{{MedlinePlus|001106|Hypoplastic left heart}}</ref> recent research indicates that HLHS may be due to genetic factors. <ref name="titleHypoplastic left heart syndrome likely caused by genetic factors">{{cite web |url=http://www.news-medical.net/?id=31066 |title=Hypoplastic left heart syndrome likely caused by genetic factors |accessdate=2008-01-09 |format= |work=}}</ref><ref name="pmid11470490">{{cite journal |author=Dasgupta C, Martinez AM, Zuppan CW, Shah MM, Bailey LL, Fletcher WH |title=Identification of connexin43 (alpha1) gap junction gene mutations in patients with hypoplastic left heart syndrome by denaturing gradient gel electrophoresis (DGGE) |journal=[[Mutat. Res.]] |volume=479 |issue=1-2 |pages=173–86 |year=2001 |pmid=11470490 |doi= 10.1016/S0027-5107(01)00160-9|url=http://linkinghub.elsevier.com/retrieve/pii/S0027510701001609}}</ref>
| |
|
| |
|
| There is evidence associating it with [[Gap junction protein, alpha 1]].<ref>{{OMIM|241550|HYPOPLASTIC LEFT HEART SYNDROME}}</ref>
| | ==[[Hypoplastic left heart syndrome differential diagnosis|Differentiating Hypoplastic left heart syndrome from other Diseases]]== |
|
| |
|
| ==Clinical Presentation== | | ==[[Hypoplastic left heart syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| In babies with HLHS, the [[aorta]] and [[left ventricle]] are very small, and the [[aortic valve|aortic]] and [[mitral valve]]s are either too small to allow sufficient blood flow or are atretic (closed) altogether. As [[blood]] returns from the [[lung]]s to the [[left atrium]], it must pass through an [[atrial septal defect]] to the right side of the heart.
| | ==[[Hypoplastic left heart syndrome natural history|Natural History, Complications, and Prognosis]]== |
|
| |
|
| In a healthy human, the left side of the heart receives [[oxygen]]-rich blood from the lungs and pumps it out to the rest of the body; with these structures underdeveloped, they cannot circulate blood to other organs, and the right ventricle must pump blood to both the lungs, as it would normally, and to the rest of the body, a situation which cannot be sustained for long.
| | ==Diagnosis== |
| | | [[Hypoplastic left heart syndrome history and symptoms|History and Symptoms]] | [[Hypoplastic left heart syndrome physical examination|Physical Examination]] | [[Hypoplastic left heart syndrome laboratory tests|Laboratory Findings]] | [[Hypoplastic left heart syndrome electrocardiogram | Electrocardiogram]] | [[Hypoplastic left heart syndrome chest x ray|Chest X Ray]] | [[Hypoplastic left heart syndrome echocardiography or ultrasound|Echocardiography]] | [[Hypoplastic left heart syndrome other imaging findings|Other Imaging Findings]] |
| In cases of HLHS, the right side of the heart often must pump blood to the body through a [[patent ductus arteriosus|patent]] [[ductus arteriosus]]. As the ductus arteriosus usually closes within eleven days after birth, blood flow is severely restricted and eventually cut off, leading to dangerously low circulation and eventually to shock.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Hypoplastic left heart syndrome medical therapy|Medical Therapy]] | [[Hypoplastic left heart syndrome surgery|Surgery]] | [[Hypoplastic left heart syndrome primary prevention|Primary Prevention]] | [[Hypoplastic left heart syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Hypoplastic left heart syndrome future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| Without treatment, HLHS is fatal, but with intervention, an infant may survive. A [[pediatric]] [[heart surgeon|cardiothoracic surgeon]] may perform a series of operations or a full [[heart transplant]]. In the meantime, the ductus may be kept open to allow bloodflow using medication containing [[prostaglandin]]. Because these operations are complex and need to be individualized for each patient, a cardiologist must assess all medical and surgical options on a case-by-case basis.
| | ==Case Studies== |
| After assessment the child's parents are given a percentage chance of survival and the choice of surgery or to take the child home to pass away.
| | [[Hypoplastic left heart syndrome case study one|Case #1]] |
|
| |
|
| The two methods for treatment of HLHS are transplantation and a three-stage surgical procedure. Each of these are open heart surgeries (meaning the chest is open and the [[sternum]] has to be separated), requiring the child to be on a heart bypass machine for at least five hours. The heart is stopped and the heart bypass machine pumps blood to the body. After successful surgery is performed there can be added complications of restarting the heart and getting the child off the heart bypass machine.
| | ==Related Chapters== |
| | *[[Congenital heart disease]] |
| | *[[Norwood procedure]] |
| | *[[Tetralogy of fallot]] |
| | *[[Edward Bove]] |
| | *[[Hypoplastic right heart syndrome]] |
|
| |
|
| The three-stage procedure is a [[Palliative care|palliative]] procedure (not a cure), as the child's circulation is made to work with only two of the heart's four chambers.
| | {{WikiDoc Help Menu}} |
| | | {{WikiDoc Sources}} |
| * The first step is the [[Norwood procedure]]. In this procedure, the right ventricle is used to pump blood into the systemic circulation. Since the right ventricle is no longer directly pumping blood to the lungs, a shunt is required in order to pass deoxygenated blood through the lungs. Either the subclavian artery can be connected to the pulmonary circulation (Blalock-Taussig shunt), or a shunt is made directly from the right ventricle to the pulmonary circulation (Sano shunt). The narrow aorta is enlarged using a patch to improve bloodflow to the body.
| |
| | |
| During this time the baby may be medically fragile and have feeding problems because the heart is working very hard. There is a considerable degree of venous mixing in the right ventricle, leading to lower oxygenation saturations. In addition, the Blalock-Taussig shunt and the Sano shunt both expose the lungs to systemic arterial pressures, leading in the long term to pulmonary hypertension and eventually to heart failure.
| |
| | |
| * The second stage, the bi-directional Glenn procedure or Hemi-Fontan (see also [[Kawashima procedure]]) relieves some of the above problems. In this operation, the superior vena cava is ligated from the heart and connected to the pulmonary circulation. At this time, the Blalock-Taussig or Sano shunt is taken down. At this point, the lungs are no longer exposed to systemic arterial pressures, but much lower venous pressures. Although venous blood from the upper half of the body is no longer mixing with oxygenated blood in the right ventricle, there is still venous mixing from the lower half of the body, leading to some degree of oxygen desaturation.
| |
| | |
| During this time the child may have improved quality of life as the heart does not have to work as hard.
| |
|
| |
| * The final procedure, the Fontan ([[Fontan procedure]]) completes the repair of the hypoplastic left heart. Although there are several variations, the functional effect is to redirect venous blood from the lower body (through the inferior vena cava) away from the right atrium to the pulmonary artery. Now, there should not be any mixing of oxygenated and deoxygenated blood in the right ventricle. The right ventricle performs the traditional job of the left, supplying the body with oxygenated blood, while the passive systemic venous pressure performs the traditional job of the right, passing deoxygenated blood to the lungs.
| |
| | |
| The Norwood Procedure is generally performed within a week of birth, the second stage at 3–6 months of age, and the Fontan at 18 months to four years of age. There are two types of Fontan: the Lateral Tunnel Fontan, and the Extracardiac Fontan. When the Fontan Procedure was first being done for children with HLHS, the only Fontan was the Lateral Tunnel Fontan. This requires actual cutting in the heart itself to create a "tunnel" by which the blood can travel passively to the lungs. Within the last decade, doctors have created an Extracardiac Fontan. This operation creates a tunnel outside the heart itself which reduces the chances of Fontan patients developing scar tissue on the heart which might later cause arrythmias.
| |
| | |
| ==Prognosis==
| |
| | |
| While infants successfully treated for HLHS have a good chance of survival, they may experience chronic health problems for the rest of their lives. The 3-stage surgeries were developed in the early 1980's with no survivors prior to that time. Therefore, the earliest survivors are in their early 20's and the long term prognosis is unknown. However, the advances in surgical and medical techniques have helped increase the survival rate dramatically since the surgeries were first developed.
| |
| | |
| As is true for patients with other types of heart defects involving malformed valves [http://www.mayoclinic.com/health/endocarditis/DS00409/DSECTION=4], HLHS patients run a high risk of [[endocarditis]], and must be monitored by a cardiologist for the rest of their lives to check on their heart function.
| |
| | |
| ==Pathological Findings==
| |
| | |
| [http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology]
| |
| | |
| [[Image:Hypoplastic left ventricle 1.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| [[Image:Hypoplastic left ventricle 2.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| [[Image:Hypoplastic left ventricle 3.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| [[Image:Hypoplastic left ventricle 4.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| [[Image:Hypoplastic left ventricle 5.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| [[Image:Hypoplastic left ventricle.jpg|left|thumb|300px|Hypoplastic left ventricle]]
| |
| <br clear="left"/>
| |
| | |
| ==External links==
| |
| | |
| * [http://heartcenter.seattlechildrens.org/conditions_treated/hypoplastic_left_heart.asp Hypoplastic Left Heart Syndrome information] from Seattle Children's Hospital Heart Center
| |
| * [http://www.tchin.org/ Congenital Heart Information Network]
| |
| * [http://www.hlhsinfo.homestead.com/ HLHS Information Page] - created for parents expecting a child with HLHS. Includes questions to ask the physicians and insurance company.
| |
| * [http://www.caheartconnection.org/ California Heart Connection] - support network for those with congenital heart defects including Hypoplastic Left Heart Syndrome (HLHS.) Free online support group
| |
| | |
| ==Sources==
| |
| *[http://www.card-ag.org Card-AG], The Cardiologycal Working Group of the University Pediatric Clinic Munster
| |
| *[http://www.americanheart.org/presenter.jhtml?identifier=1353 Hypoplastic Left Heart Syndrome], American Heart Association
| |
| *Information on HLHS from the [http://www.cincinnatichildrens.org/health/heart-encyclopedia/anomalies/hlhs.htm Cincinnati Children's Hospital Medical Center], accessed 9 July, 2006
| |
|
| |
|
| | [[Category:Cardiology]] |
| | [[Category:Disease]] |
| | [[Category:Neonatology]] |
| [[Category:Congenital heart disease]] | | [[Category:Congenital heart disease]] |
| | | [[Category:Pediatrics]] |
| *Hypoplastic Left Heart Syndrome - [http://www.med.umich.edu/cvc/mchc/parhyp.htm University of Michigan Congenital Heart Center]
| | [[Category:Mature chapter]] |
| | |
| {{Congenital malformations and deformations of circulatory system}}
| |
| {{SIB}}
| |
| [[de:Hypoplastisches Linksherz-Syndrom]] | |
| [[nn:Hypoplastisk venstre hjarte-syndrom]]
| |
| [[uk:Синдром гіпоплазії лівих відділів серця]]
| |
| | |
| [[Category:Cardiology]] | |
| | |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |