High density lipoprotein future or investigational therapies: Difference between revisions
No edit summary |
|||
| Line 33: | Line 33: | ||
==Cholesterol Ester Transfer Protein (CETP) Inhibition== | ==Cholesterol Ester Transfer Protein (CETP) Inhibition== | ||
The goal of this therapy is to prevent the transfer of esterified cholesterol from HDL to triglyceride-rich lipoproteins in exchange for triglycerides. This method not only increases the cholesterol content per HDL particle, but also affects the compositions and serum levels of VLDL, VLDL remnants, and LDLs. The cardiovascular benefits of this therapy is unclear due to the failures observed with earlier trials - [[torcetrapib]] ([[ILLUMINATE Trial]]) and [[dalcetrapib]] ([[Dal-OUTCOMES Trial]]). The [[ILLUMINATE Trial]] failed due to | The goal of this therapy is to prevent the transfer of esterified [[cholesterol]] from HDL to triglyceride-rich lipoproteins in exchange for [[triglycerides]]. This method not only increases the cholesterol content per HDL particle, but also affects the compositions and serum levels of VLDL, VLDL remnants, and LDLs. The cardiovascular benefits of this therapy is unclear due to the failures observed with earlier trials - [[torcetrapib]] ([[ILLUMINATE Trial]]) and [[dalcetrapib]] ([[Dal-OUTCOMES Trial]]). The [[ILLUMINATE Trial]] failed due to observed off-target effects on blood pressure which increased mortality in subjects.<ref name="pmid17984165">{{cite journal| author=Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M et al.| title=Effects of torcetrapib in patients at high risk for coronary events. | journal=N Engl J Med | year= 2007 | volume= 357 | issue= 21 | pages= 2109-22 | pmid=17984165 | doi=10.1056/NEJMoa0706628 | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17984165 }} </ref> Despite a 31–40% elevation in HDL-C observed with [[dalcetrapib]], it failed to show a positive cardiovascular outcome in patients with ACS.<ref name="pmid23126252">{{cite journal| author=Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J et al.| title=Effects of dalcetrapib in patients with a recent acute coronary syndrome. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 22 | pages= 2089-99 | pmid=23126252 |doi=10.1056/NEJMoa1206797 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23126252 }} </ref> Two other new CETP inhibitors ([[anacetrapib]] and [[evacetrapib]]) are in phase 3 clinical trials with promising results. Both anacetrapib (MK-0859) and evacetrapib (LY248595) raise HDL levels without affecting the blood pressure.<ref name="Krishna-2007">{{Cite journal | last1 = Krishna | first1 = R. | last2 = Anderson | first2 = MS. | last3 = Bergman | first3 = AJ. | last4 = Jin | first4 = B. | last5 = Fallon | first5 = M. | last6 = Cote | first6 = J. | last7 = Rosko | first7 = K. | last8 = Chavez-Eng | first8 = C. | last9 = Lutz | first9 = R. | title = Effect of the cholesteryl ester transfer protein inhibitor, anacetrapib, on lipoproteins in patients with dyslipidaemia and on 24-h ambulatory blood pressure in healthy individuals: two double-blind, randomised placebo-controlled phase I studies. | journal = Lancet | volume = 370 | issue = 9603 | pages = 1907-14 | month = Dec | year = 2007 | doi = 10.1016/S0140-6736(07)61813-3 | PMID = 18068514 }}</ref><ref name="Nicholls-2011">{{Cite journal | last1 = Nicholls | first1 = SJ. | last2 = Brewer | first2 = HB. | last3 = Kastelein | first3 = JJ. | last4 = Krueger | first4 = KA. | last5 = Wang | first5 = MD. | last6 = Shao | first6 = M. | last7 = Hu | first7 = B. | last8 = McErlean | first8 = E. | last9 = Nissen | first9 = SE. | title = Effects of the CETP inhibitor evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial. | journal = JAMA | volume = 306 | issue = 19 | pages = 2099-109 | month = Nov | year = 2011 | doi = 10.1001/jama.2011.1649 | PMID = 22089718 }}</ref> The effects of evacetrapib on cardiovascular outcomes are being examined in the Assessment of Clinical Effects of Cholesteryl Ester Transfer Protein Inhibition with Evacetrapib in Patients at a High-Risk for Vascular Outcomes ([[ACCELERATE Trial]]) by Eli Lilly and Company, currently enrolling 11,000 patients after ACS.<ref name="clinicaltrials.gov">{{Cite web | last = | first = | title = A Study of Evacetrapib in High-Risk Vascular Disease - Full Text View - ClinicalTrials.gov | url = http://clinicaltrials.gov/ct2/show/NCT01687998?term=NCT01687998&rank=1 | publisher = | date = | accessdate = 20 September 2013 }}</ref> The expected date of completion is January, 2016. The REVEAL HPS-3/TIMI-55 trial will assess whether lipid modification with [[anacetrapib]] 100mg daily reduces the risk of coronary death, myocardial infarction or coronary revascularization (collectively known as major coronary events) in 30,000 patients with circulatory problems who have their Low-density Lipoprotein (LDL) cholesterol level treated with a statin. The expected date of completion is January, 2017.<ref name="clinicaltrials.gov">{{Cite web | last = | first = | title = REVEAL: Randomized EValuation of the Effects of Anacetrapib Through Lipid-modification - Full Text View - ClinicalTrials.gov | url = http://clinicaltrials.gov/ct2/show/NCT01252953?term=NCT01252953&rank=1 | publisher = | date = | accessdate = 20 September 2013 }}</ref> | ||
===CETi-1 Vaccine=== | ===CETi-1 Vaccine=== | ||
Revision as of 13:50, 23 September 2013
|
High Density Lipoprotein Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Clinical Trials |
|
Case Studies |
|
High density lipoprotein future or investigational therapies On the Web |
|
American Roentgen Ray Society Images of High density lipoprotein future or investigational therapies |
|
FDA on High density lipoprotein future or investigational therapies |
|
CDC on High density lipoprotein future or investigational therapies |
|
High density lipoprotein future or investigational therapies in the news |
|
Blogs on High density lipoprotein future or investigational therapies |
|
Risk calculators and risk factors for High density lipoprotein future or investigational therapies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The association between HDL level and cardiovascular disease has been widely reported in the literature. In fact, 1 out of every 7 statin treated patients has residual cardiovascular disease,[1] which sheds light to the importance of developing new therapies targeting HDL quantity and quality in high risk patients.[2]
The Need
The importance of increasing the serum levels and functionality of HDL in lowering residual cardiovascular risks in patients with acute coronary syndromes cannot be over-emphasized. First of all, some recent studies reported failures of orally active medications that increase serum levels of HDL-C to potentially improve cardiovascular outcomes, such as niacin in the AIM-HIGH Trial. This has shifted the scope of HDL therapy towards increasing the qualitative functionality of HDL i.e., cellular cholesterol efflux, HDL-mediated reverse cholesterol transport mechanism, associated enzymatic activities, particle size and electrophoretic mobility, anti-inflammatory, and anti-oxidant properties, rather than the quantitative elevation of serum HDL-C which was the previous target. Secondly, since the available oral medications elevate HDL over weeks to months, there is the need for medications which rapidly improve outcomes during acute vascular events.
Shown below is an image depicting the different drug targets to increase HDL level.
Adopted from Nature Reviews Drug Discovery. ABCA1= ATP-binding cassette transporter A1; ABCG1: ATP-binding cassette transporter G1; ABCG4: ATP-binding cassette transporter G4; ApoA-I= Apolipoprotein A-I; CETP: Cholesteryl transfer protein; LCAT: Lecithin cholesterol acyltransferase; LXR: Liver X receptors; PPARγ: Peroxisome proliferator-activated receptor gamma; RXR: Retinoid X recptor; SRBI: Scavenger receptor, class B, type I. [3]
Direct Infusion of Apo A-1
These methods aim at directly increasing the serum levels of HDL through the infusion of reconstituted and recombinant preparations of HDLs (rHDLs). Recombinant HDLs are made from apo A-1 derived from cellular expression systems while recombinant HDLs are apo A-1 derived from human plasma. Both preparations have been complexed with phospholipids. The reconstituted forms are relatively cheaper and easier to produce.
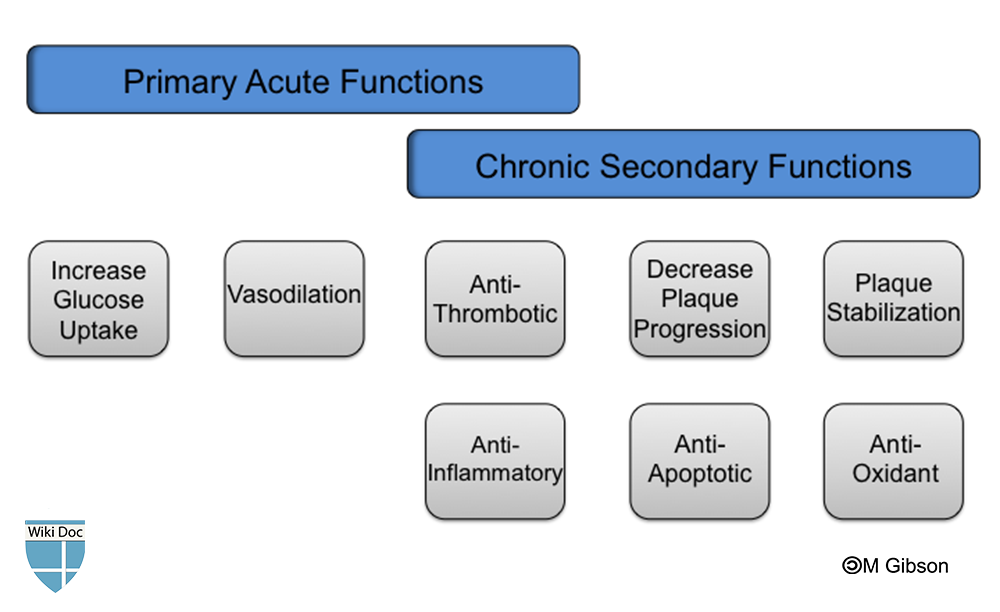
Shown below is an image depicting the suggested acute and chronic functions of HDL infusions in the setting of cardiovascular disease.
ApoA-1 Milano
Some individuals in rural Italy were identified with a genetic variant of apo A-1 which conferred some protection against atherosclerosis despite the presence of very low HDL levels (10-30 mg/dl), elevated plasma LDL, and moderate hypertriglyceridemia.[4] Studies indicated that intravenous infusion of recombinant apoA-I Milano (ETC-216, now MDCO-216 since 2009) promoted regression of atherosclerotic lesions to a greater extent than wild type apo A-I as measured by intravascular ultrasound within 5 weeks of treatment.[5] However, further studies regarding these agents have been halted by procedural and manufactural difficulties.
CSL-112
CSL-112 (CSL Behring), a reformulated version of CSL-111, is a reconstituted HDL complexed with soybean phosphatidylcholine, and has been reported to cause up to 20-fold elevation in serum pre-Beta-1-HDL following a single infusion according to the phase 1 trial.[6] Currently, there are pending results regarding phase 2a which was recently completed. ERASE Trial which examined the effect and tolerability of CSL-111, a precursor to CSL-112, showed regression of coronary atherosclerotic lesions in ACS patients but was discontinued due to abnormal liver transaminase elevations observed with the high-dosed group. However, there was no significant change in atheroma volume (measured by IVUS) despite a 64% increase in HDL and a 23% reduction in LDL.[7]
CER-001
Two ongoing trials from Cerenis Therapeutics are assessing the effects of CER-001, an engineered pre-beta-like HDL particle, on total coronary plaque volume (measured by IVUS) in patients with acute coronary syndrome - CHI-SQUARE Study, and on total carotid plaque volume in patients with homozygous familial hypercholesterolemia (measured by MRI) - MODE Study.
Cholesterol Ester Transfer Protein (CETP) Inhibition
The goal of this therapy is to prevent the transfer of esterified cholesterol from HDL to triglyceride-rich lipoproteins in exchange for triglycerides. This method not only increases the cholesterol content per HDL particle, but also affects the compositions and serum levels of VLDL, VLDL remnants, and LDLs. The cardiovascular benefits of this therapy is unclear due to the failures observed with earlier trials - torcetrapib (ILLUMINATE Trial) and dalcetrapib (Dal-OUTCOMES Trial). The ILLUMINATE Trial failed due to observed off-target effects on blood pressure which increased mortality in subjects.[8] Despite a 31–40% elevation in HDL-C observed with dalcetrapib, it failed to show a positive cardiovascular outcome in patients with ACS.[9] Two other new CETP inhibitors (anacetrapib and evacetrapib) are in phase 3 clinical trials with promising results. Both anacetrapib (MK-0859) and evacetrapib (LY248595) raise HDL levels without affecting the blood pressure.[10][11] The effects of evacetrapib on cardiovascular outcomes are being examined in the Assessment of Clinical Effects of Cholesteryl Ester Transfer Protein Inhibition with Evacetrapib in Patients at a High-Risk for Vascular Outcomes (ACCELERATE Trial) by Eli Lilly and Company, currently enrolling 11,000 patients after ACS.[12] The expected date of completion is January, 2016. The REVEAL HPS-3/TIMI-55 trial will assess whether lipid modification with anacetrapib 100mg daily reduces the risk of coronary death, myocardial infarction or coronary revascularization (collectively known as major coronary events) in 30,000 patients with circulatory problems who have their Low-density Lipoprotein (LDL) cholesterol level treated with a statin. The expected date of completion is January, 2017.[12]
CETi-1 Vaccine
The CETi-1 vaccine (developed by AVANT Immunotherapeutics) induces antibodies specific for a portion of the cholesteryl ester transfer protein (CETP). Only one patient out of a total of 36 patients who received a single injection of the vaccine developed anti-CETP antibodies. After the study was extended, out of a total of 23 patients, 53% (8/15) developed anti-CETP antibodies following a second injection of the active vaccine compared with 0% (0/8) in the placebo group. The vaccine was well tolerated and no adverse event was reported. Despite a significant 8.4% increase in HDL among patients not on statins, more human studies are needed to determine whether repeated vaccinations will induce more antibodies which may translate to greater elevations in HDL.[13]
JTT-705
JTT-705, a partial inhibitor of CETP, was first tested in human subjects by Japan Tobacco Inc. in 2002. In a 4-week study to assess the efficacy and safety of ascending doses of JTT-705 in 198 healthy subjects with mild hyperlipidemia, results revealed a 37% decrease in CETP activity (P<0.0001), 34% increase in HDL cholesterol (P<0.0001), 7% decrease in LDL cholesterol (P=0.017), an increase in total HDL, HDL2, HDL3, and apolipoprotein A-I. Although minor gastrointestinal side effects were observed, the long-term effect on coronary artery disease needs to be assessed.[14] Better results were observed when JTT-705 was combined with statins including the preservation of HDL's anti-oxidant properties observed with CETP inhibition.[15]
De-lipidated HDL Infusions
This is a relatively new approach which involves autologous infusion of de-lipidated HDL using the Plasma De-lipidation System-2 (PDS-2) produced by Lipid Sciences.[16] The process involves the selective removal of apoA-I HDL particles, and the delipidation (converting alphaHDL to pre-beta-like HDL) reinfusion of the cholesterol-depleted functional pre-β HDL - the active form of HDL. In the first human trial, 28 patients with ACS undergoing cardiac catheterization received 5 weekly infusions of de-lipidated HDL or placebo. This led to a 73.5% increase in pre-beta-like HDL and 71.9% decrease in the alphaHDL contents of the de-lipidated plasma which was responsible for the 5.2% decreased in the total atheroma volume (measured by IVUS) observed. A third of the patients experienced hypotension due to apheresis.
HDL Mimetics
ApoA-1 Mimetic Peptides
These are short synthetic peptides that mimic the amphipathic α-helix of apoA-I. APP018 by Novartis (formerly developed as D-4F by Bruin Pharma), synthesized from D-amino acids, is resistant to degradation by gastric enzymes, thus, it can be administered orally. In animal models, D-4F has been demonstrated to exerts similar effects as native apoA-1 such as : cholesterol efflux from macrophages via ABCA1,[17] delivery of cholesterol to hepatocytes via the SCARB1,[18] anti-inflammatory properties,[19][20] anti-oxidant properties which exceeds native apoA-1 - shows more affinity for oxidized phospholipids and fatty acids,[21] retains the ability to inhibit the production of chemokines,[22] and its anti-platelet properties.[23] All these properties have been shown to translate to atheroprotective effects. Studies in humans have been limited by its limited bioavailability, partially due to gender variability and reports of adverse events independent of the dose.[24] The effect of D-4F on atherosclerosis has not been demonstrated in humans. Other apoA-1 mimetic drugs include: 2F, 3F, 5F, 6F, and 7F.
ATI-5261 Synthetic Peptide
This is a synthetic peptide that stimulates ABCA1 cholesterol efflux with similar potency with apoA-I. Studies in mice demonstrated a 45% reduction of aortic atherosclerosis following daily intraperitoneal injections for 6 weeks, and also increased reverse cholesterol transport from macrophage foam-cells to feces over 24-48 hours.[25] This novel approach currently awaits early phase clinical trials.
Endothelial Lipase Inhibitors
Endothelial lipases, synthesized by vascular endothelial cells, represent a potential target to reduce HDL catabolism thereby increasing the serum levels of HDLs and apoA-1. Some human studies have hypothesized an atherogenic role for endothelial lipase especially in overweight individuals and in those with metabolic syndrome, with a positive association between plasma levels of this enzyme and coronary artery calcification.[26] Carriers of endothelial lipase variants associated with HDL-C levels demonstrated a decreased risk of coronary artery disease.[27] Although the inactivation of endothelial lipases was expected to reduce atherosclerosis by raising serum HDL-C levels, the results have been the opposite - resulting into accumulation of small, dense, atherogenic LDLs, despite elevations in serum HDLs. Similar result was also reported in hepatic lipase deficiency. Despite all these negative results, inhibiting EL still remains an object of interest of future therapeutic value. In a study, it was demonstrated that targeted inactivation of EL increased plasma HDL-C level and inhibited atherosclerosis.[28] Examples of drugs include boronic acid inhibitors and selective sulfonylfuran urea.
LCAT Modulators
Lecithin-cholesterol acyltransferase catalyses the esterification of free cholesterol as well as the maturation of HDLs. Therefore, a reduction of its activity will lead to reduced serum levels of HDL-C. Conversely, the effect of LCAT on reverse cholesterol transport and the development of atherosclerosis is controvertial. Some studies have demonstrated a negative cardiovascular outcome with a high LCAT activity, for example, in the Prevention of Renal and Vascular Endstage Disease (PREVEND) study, a high LCAT activity independently predicted an increased risk of cardiovascular events.[29] Despite all these results, a human recombinant LCAT (rLCAT) by AlphaCore Pharma, injected into LCAT-deficient mice was observed to increase HDL-C to near normal levels for several days. Also, the intravenous infusion of human rLCAT in rabbits was found to increase HDL-C, increase fecal secretion of cholesterol, and reduce atherosclerosis.[30] Phase 1 trial results for ETC-642 (RLT Peptide) by Esperion Therapeutics revealed a rapid dose-related cholesterol mobilisation, as well as evidence of increases in HDL-cholesterol levels.
Endocannabinoid Receptor Blockers
Cannabis is a recreational drug which has been in existence for over 4,500 years. Although the plant contains various other cannabinoids, its main active substance is tetrahydrocannabinol (THC) which has been used for the management of post-chemotherapy emesis, as well as HIV-associated anorexia. The endocannabinoids exerts their pharmacological actions by binding to G-protein coupled receptors - CB1 present in the brain, autonomic nervous system, liver, muscle, gastrointestinal tract, and adipose tissue; CB2 are primarily in the lymphoid tissue and peripheral macrophages. Activation of CB1 receptors in the brain diminishes satiety and in the adipose tissue causes lipogenesis and production of adiponectin, which promotes insulin sensitivity. Rimonobant (SR141716), manufactured by Sanofi Aventis, is the first selective CB1 receptor blocker to be approved as an appetite suppression and for treating obesity.[31] According to The Rimonabant in Obesity-Lipids (RIO-Lipids) study which evaluated the lipid effects of rimonabant in 1036 overweight or obese patients with untreated dyslipidemia, there was a 23% increase in HDL-C levels, 15% decrease in triglyceride levels, and a 57.7% increase in adiponectin levels observed in the high-dosed group.[32] However, adverse psychiatric and neurological effects (e.g., depression or anxiety) were reported which prevented its approval by the FDA in the United States as a weight control medication.[33] These positive effects have also been demonstrated in other trials - The RIO-Europe Trial,[34] RIO-North America,[35] as well as its beneficial effect on smoking cessation.[36]
ApoA-1 Upregulators
The goal of this therapy is to up-regulate the endogenous synthesis of the major protein on HDL particles and apoA-1.
RVX-208
RVX-208 a.k.a RVX000222, manufactured by Resverlogix Corp, is a small synthetic molecule belonging to the quinazoline family (anti-malarial). Oral administration of RVX-208 was demonstrated in increase plasma levels of both apoA-I and HDL-C up to 60% and 97% respectively, in a dose-dependent manner and promotes cholesterol efflux in african green monkeys.[37] These effects have also been demonstrated in humans subjects according to the ASSERT Study - Phase 2a.[11] Currently, two phase 2b trials have just been completed where its lipid efficacy, safety and tolerability (SUSTAIN Study) and effect on plaque burden (ASSURE Study) were independently assessed.[38] The result from these trials are still pending.
Synthetic Liver X Receptor (LXR) Agonists
Liver X receptors (LXRs), a member of the nuclear receptor super-family, have an important role in lipid metabolism. There are two isoforms - LXRα and LXRβ. LXRα is present in the liver, macrophages, intestine, kidney, and adipose tissue, while LXRβ is ubiquitously distributed.[39] Activating LXRs have been demonstrated to induce intracellular cholesterol mobilization,[40]increase cholesterol efflux from macrophages via ABCA1 and ABCG1,[41] and increase intestinal HDL production.[42] Unfortunately, further development of these agents have been halted by the induction of hepatic steatosis and increased plasma triglyceride concentration in the liver.[43] Fortunately, further research has identified solutions to these limitations:
- Selective activation of LXRβ - Activation of LXRα has been linked to the development of fatty liver and increase in triglyceride levels. Therefore, selective LXRβ agonist might increase reverse cholesterol transport without inducing either hypertriglyceridemia or fatty liver.[44]
- Selective activation of intestinal LXRs - Activation of hepatic LXRs promotes lipogenesis and elevation of triglyceride levels by upregulation of SREBP1c. An intestine-specific LXRα/β agonist, GW6340, induced macrophage-specific reverse cholesterol transport and increased intestinal HDL production.[45]
Other LXR agonists include:
| LXR AGONIST | EFFECT |
| T091317 | Widely used in LXR research to decreases atherosclerosis in mice by inducing NCP1 and NCP2 genes in macrophages. |
| LXR-623 | Increases ABCA1 and ABCG1 expression in cells. CNS adverse effects.[46] Reduction in plaque progression in combination with statins. |
| AZ876 | Reduces atherosclerosis[47] |
| GW3965 | Reduces atherosclerosis[47] |
| GW6340 | Intestine-specific LXRα/β agonist, induces cholesterol efflux and increases intestinal excretion of HDL-derived cholesterol[45] |
| AT1-111 | New agent. Inhibits atherosclerosis and plaque formation in mice.[48] More potent than T091317 |
| SR9238 | Newest agent. Inhibits hepatic steatosis in the treatment of non-alcoholic fatty liver[49] |
Synthetic FXR Agonists
Farnesoid X receptor is a metabolic nuclear receptor activated by bile acids, and plays an important role in cholesterol metabolism.[50] Its activation leads to both pro- and anti-atherosclerosis. Although FXR was shown to reduce plasma HDL in earlier studies,[50] it was demonstrated that FXR agonists promote HDL-derived cholesterol excretion into feces in mice and monkeys.[51] This has prompted growing interests in this field. Examples of FXR agonists include GW4064, 6-ECDCA, FXR-450, and PX20606.
Gene Therapy
Although gene therapy had been attempted in the past with little success, there are evidences which suggest that gene therapy may be a potential target in combating cardiovascular and metabolic disorders. Some of them include:
- Human ApoA-1 transgene experiments yielded a two-fold elevation in HDL cholesterol and inhibited progression of atherosclerosis in animals.[52]
- Alipogene tiparvovec (AAV1-LPLS447X) therapy in 20 patients with lipoprotein lipase deficiency and recurrent pancreatitis yielded a 40% reduction in the serum triglyceride levels in half of the patients between 3 and 12 weeks.[53] Unfortunately, serum HDL cholesterol was not measured in these patients.
- Injection of an anti-miR-33 oligonucleotide in mice showed an increase in ABCA1 mRNA expression and HDL levels[54] proving that HDL cholesterol can be increased by increasing ABCA1 and ABCG1 expression through the microRNA.
All these evidences emphasize the genetic basis for the development of cardiovascular and metabolic disorders, and also explains the importance of gene therapy or somatic gene transfer as a potential therapeutic target.
References
- ↑ Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C; et al. (2005). "Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins". Lancet. 366 (9493): 1267–78. doi:10.1016/S0140-6736(05)67394-1. PMID 16214597. Review in: ACP J Club. 2006 May-Jun;144(3):62
- ↑ Mora S, Glynn RJ, Ridker PM (2013). "High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy". Circulation. 128 (11): 1189–97. doi:10.1161/CIRCULATIONAHA.113.002671. PMID 24002795.
- ↑ Linsel-Nitschke P, Tall AR (2005). "HDL as a target in the treatment of atherosclerotic cardiovascular disease". Nat Rev Drug Discov. 4 (3): 193–205. doi:10.1038/nrd1658. PMID 15738977.
- ↑ Sirtori, CR.; Calabresi, L.; Franceschini, G.; Baldassarre, D.; Amato, M.; Johansson, J.; Salvetti, M.; Monteduro, C.; Zulli, R. (2001). "Cardiovascular status of carriers of the apolipoprotein A-I(Milano) mutant: the Limone sul Garda study". Circulation. 103 (15): 1949–54. PMID 11306522. Unknown parameter
|month=ignored (help) - ↑ Nissen, SE.; Tsunoda, T.; Tuzcu, EM.; Schoenhagen, P.; Cooper, CJ.; Yasin, M.; Eaton, GM.; Lauer, MA.; Sheldon, WS. (2003). "Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial". JAMA. 290 (17): 2292–300. doi:10.1001/jama.290.17.2292. PMID 14600188. Unknown parameter
|month=ignored (help) - ↑ "http://circ.ahajournals.org/cgi/content/meeting_abstract/126/21_MeetingAbstracts/A11851". Retrieved 16 September 2013. External link in
|title=(help) - ↑ Tardif JC, Grégoire J, L'Allier PL; et al. (2007). "Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial". JAMA : the Journal of the American Medical Association. 297 (15): 1675–82. doi:10.1001/jama.297.15.jpc70004. PMID 17387133. Unknown parameter
|month=ignored (help) - ↑ Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M; et al. (2007). "Effects of torcetrapib in patients at high risk for coronary events". N Engl J Med. 357 (21): 2109–22. doi:10.1056/NEJMoa0706628. PMID 17984165.
- ↑ Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J; et al. (2012). "Effects of dalcetrapib in patients with a recent acute coronary syndrome". N Engl J Med. 367 (22): 2089–99. doi:10.1056/NEJMoa1206797. PMID 23126252.
- ↑ Krishna, R.; Anderson, MS.; Bergman, AJ.; Jin, B.; Fallon, M.; Cote, J.; Rosko, K.; Chavez-Eng, C.; Lutz, R. (2007). "Effect of the cholesteryl ester transfer protein inhibitor, anacetrapib, on lipoproteins in patients with dyslipidaemia and on 24-h ambulatory blood pressure in healthy individuals: two double-blind, randomised placebo-controlled phase I studies". Lancet. 370 (9603): 1907–14. doi:10.1016/S0140-6736(07)61813-3. PMID 18068514. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1 Nicholls, SJ.; Brewer, HB.; Kastelein, JJ.; Krueger, KA.; Wang, MD.; Shao, M.; Hu, B.; McErlean, E.; Nissen, SE. (2011). "Effects of the CETP inhibitor evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial". JAMA. 306 (19): 2099–109. doi:10.1001/jama.2011.1649. PMID 22089718. Unknown parameter
|month=ignored (help) - ↑ 12.0 12.1 "A Study of Evacetrapib in High-Risk Vascular Disease - Full Text View - ClinicalTrials.gov". Retrieved 20 September 2013.
- ↑ Davidson, MH.; Maki, K.; Umporowicz, D.; Wheeler, A.; Rittershaus, C.; Ryan, U. (2003). "The safety and immunogenicity of a CETP vaccine in healthy adults". Atherosclerosis. 169 (1): 113–20. PMID 12860257. Unknown parameter
|month=ignored (help) - ↑ de Grooth, GJ.; Kuivenhoven, JA.; Stalenhoef, AF.; de Graaf, J.; Zwinderman, AH.; Posma, JL.; van Tol, A.; Kastelein, JJ. (2002). "Efficacy and safety of a novel cholesteryl ester transfer protein inhibitor, JTT-705, in humans: a randomized phase II dose-response study". Circulation. 105 (18): 2159–65. PMID 11994249. Unknown parameter
|month=ignored (help) - ↑ Bisoendial, RJ.; Hovingh, GK.; El Harchaoui, K.; Levels, JH.; Tsimikas, S.; Pu, K.; Zwinderman, AE.; Kuivenhoven, JA.; Kastelein, JJ. (2005). "Consequences of cholesteryl ester transfer protein inhibition in patients with familial hypoalphalipoproteinemia". Arterioscler Thromb Vasc Biol. 25 (9): e133–4. doi:10.1161/01.ATV.0000179009.60612.28. PMID 16127020. Unknown parameter
|month=ignored (help) - ↑ Waksman, R.; Torguson, R.; Kent, KM.; Pichard, AD.; Suddath, WO.; Satler, LF.; Martin, BD.; Perlman, TJ.; Maltais, JA. (2010). "A first-in-man, randomized, placebo-controlled study to evaluate the safety and feasibility of autologous delipidated high-density lipoprotein plasma infusions in patients with acute coronary syndrome". J Am Coll Cardiol. 55 (24): 2727–35. doi:10.1016/j.jacc.2009.12.067. PMID 20538165. Unknown parameter
|month=ignored (help) - ↑ Song, X.; Fischer, P.; Chen, X.; Burton, C.; Wang, J. (2009). "An apoA-I mimetic peptide facilitates off-loading cholesterol from HDL to liver cells through scavenger receptor BI". Int J Biol Sci. 5 (7): 637–46. PMID 19847320.
- ↑ Smythies, LE.; White, CR.; Maheshwari, A.; Palgunachari, MN.; Anantharamaiah, GM.; Chaddha, M.; Kurundkar, AR.; Datta, G. (2010). "Apolipoprotein A-I mimetic 4F alters the function of human monocyte-derived macrophages". Am J Physiol Cell Physiol. 298 (6): C1538–48. doi:10.1152/ajpcell.00467.2009. PMID 20219948. Unknown parameter
|month=ignored (help) - ↑ Van Lenten, BJ.; Wagner, AC.; Jung, CL.; Ruchala, P.; Waring, AJ.; Lehrer, RI.; Watson, AD.; Hama, S.; Navab, M. (2008). "Anti-inflammatory apoA-I-mimetic peptides bind oxidized lipids with much higher affinity than human apoA-I". J Lipid Res. 49 (11): 2302–11. doi:10.1194/jlr.M800075-JLR200. PMID 18621920. Unknown parameter
|month=ignored (help) - ↑ Datta, G.; Chaddha, M.; Hama, S.; Navab, M.; Fogelman, AM.; Garber, DW.; Mishra, VK.; Epand, RM.; Epand, RF. (2001). "Effects of increasing hydrophobicity on the physical-chemical and biological properties of a class A amphipathic helical peptide". J Lipid Res. 42 (7): 1096–104. PMID 11441137. Unknown parameter
|month=ignored (help) - ↑ Buga, GM.; Navab, M.; Imaizumi, S.; Reddy, ST.; Yekta, B.; Hough, G.; Chanslor, S.; Anantharamaiah, GM.; Fogelman, AM. (2010). "L-4F alters hyperlipidemic (but not healthy) mouse plasma to reduce platelet aggregation". Arterioscler Thromb Vasc Biol. 30 (2): 283–9. doi:10.1161/ATVBAHA.109.200162. PMID 19965777. Unknown parameter
|month=ignored (help) - ↑ Bloedon, LT.; Dunbar, R.; Duffy, D.; Pinell-Salles, P.; Norris, R.; DeGroot, BJ.; Movva, R.; Navab, M.; Fogelman, AM. (2008). "Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients". J Lipid Res. 49 (6): 1344–52. doi:10.1194/jlr.P800003-JLR200. PMID 18323573. Unknown parameter
|month=ignored (help) - ↑ Bielicki, JK.; Zhang, H.; Cortez, Y.; Zheng, Y.; Narayanaswami, V.; Patel, A.; Johansson, J.; Azhar, S. (2010). "A new HDL mimetic peptide that stimulates cellular cholesterol efflux with high efficiency greatly reduces atherosclerosis in mice". J Lipid Res. 51 (6): 1496–503. doi:10.1194/jlr.M003665. PMID 20075422. Unknown parameter
|month=ignored (help) - ↑ Badellino, KO.; Wolfe, ML.; Reilly, MP.; Rader, DJ. (2006). "Endothelial lipase concentrations are increased in metabolic syndrome and associated with coronary atherosclerosis". PLoS Med. 3 (2): e22. doi:10.1371/journal.pmed.0030022. PMID 16354105. Unknown parameter
|month=ignored (help) - ↑ Tang, NP.; Wang, LS.; Yang, L.; Zhou, B.; Gu, HJ.; Sun, QM.; Cong, RH.; Zhu, HJ.; Wang, B. (2008). "Protective effect of an endothelial lipase gene variant on coronary artery disease in a Chinese population". J Lipid Res. 49 (2): 369–75. doi:10.1194/jlr.M700399-JLR200. PMID 17986713. Unknown parameter
|month=ignored (help) - ↑ Brown, RJ.; Lagor, WR.; Sankaranaravanan, S.; Yasuda, T.; Quertermous, T.; Rothblat, GH.; Rader, DJ. (2010). "Impact of combined deficiency of hepatic lipase and endothelial lipase on the metabolism of both high-density lipoproteins and apolipoprotein B-containing lipoproteins". Circ Res. 107 (3): 357–64. doi:10.1161/CIRCRESAHA.110.219188. PMID 20558822. Unknown parameter
|month=ignored (help) - ↑ Dullaart, RP.; Perton, F.; van der Klauw, MM.; Hillege, HL.; Sluiter, WJ. (2010). "High plasma lecithin:cholesterol acyltransferase activity does not predict low incidence of cardiovascular events: possible attenuation of cardioprotection associated with high HDL cholesterol". Atherosclerosis. 208 (2): 537–42. doi:10.1016/j.atherosclerosis.2009.07.042. PMID 19698944. Unknown parameter
|month=ignored (help) - ↑ Rousset, X.; Shamburek, R.; Vaisman, B.; Amar, M.; Remaley, AT. (2011). "Lecithin cholesterol acyltransferase: an anti- or pro-atherogenic factor?". Curr Atheroscler Rep. 13 (3): 249–56. doi:10.1007/s11883-011-0171-6. PMID 21331766. Unknown parameter
|month=ignored (help) - ↑ Rinaldi-Carmona, M.; Barth, F.; Héaulme, M.; Shire, D.; Calandra, B.; Congy, C.; Martinez, S.; Maruani, J.; Néliat, G. (1994). "SR141716A, a potent and selective antagonist of the brain cannabinoid receptor". FEBS Lett. 350 (2–3): 240–4. PMID 8070571. Unknown parameter
|month=ignored (help) - ↑ Després, JP.; Golay, A.; Sjöström, L. (2005). "Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia". N Engl J Med. 353 (20): 2121–34. doi:10.1056/NEJMoa044537. PMID 16291982. Unknown parameter
|month=ignored (help) - ↑ Leite, CE.; Mocelin, CA.; Petersen, GO.; Leal, MB.; Thiesen, FV. "Rimonabant: an antagonist drug of the endocannabinoid system for the treatment of obesity". Pharmacol Rep. 61 (2): 217–24. PMID 19443932.
- ↑ Van Gaal, LF.; Rissanen, AM.; Scheen, AJ.; Ziegler, O.; Rössner, S. "Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study". Lancet. 365 (9468): 1389–97. doi:10.1016/S0140-6736(05)66374-X. PMID 15836887.
- ↑ Pi-Sunyer, FX.; Aronne, LJ.; Heshmati, HM.; Devin, J.; Rosenstock, J. (2006). "Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial". JAMA. 295 (7): 761–75. doi:10.1001/jama.295.7.761. PMID 16478899. Unknown parameter
|month=ignored (help) - ↑ Cox, SL. (2005). "Rimonabant hydrochloride: an investigational agent for the management of cardiovascular risk factors". Drugs Today (Barc). 41 (8): 499–508. doi:10.1358/dot.2005.41.8.893709. PMID 16234873. Unknown parameter
|month=ignored (help) - ↑ Bailey, D.; Jahagirdar, R.; Gordon, A.; Hafiane, A.; Campbell, S.; Chatur, S.; Wagner, GS.; Hansen, HC.; Chiacchia, FS. (2010). "RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo". J Am Coll Cardiol. 55 (23): 2580–9. doi:10.1016/j.jacc.2010.02.035. PMID 20513599. Unknown parameter
|month=ignored (help) - ↑ Nicholls, SJ.; Gordon, A.; Johannson, J.; Ballantyne, CM.; Barter, PJ.; Brewer, HB.; Kastelein, JJ.; Wong, NC.; Borgman, MR. (2012). "ApoA-I induction as a potential cardioprotective strategy: rationale for the SUSTAIN and ASSURE studies". Cardiovasc Drugs Ther. 26 (2): 181–7. doi:10.1007/s10557-012-6373-5. PMID 22349989. Unknown parameter
|month=ignored (help) - ↑ Alberti, S.; Steffensen, KR.; Gustafsson, JA. (2000). "Structural characterisation of the mouse nuclear oxysterol receptor genes LXRalpha and LXRbeta". Gene. 243 (1–2): 93–103. PMID 10675617. Unknown parameter
|month=ignored (help) - ↑ Rigamonti, E.; Helin, L.; Lestavel, S.; Mutka, AL.; Lepore, M.; Fontaine, C.; Bouhlel, MA.; Bultel, S.; Fruchart, JC. (2005). "Liver X receptor activation controls intracellular cholesterol trafficking and esterification in human macrophages". Circ Res. 97 (7): 682–9. doi:10.1161/01.RES.0000184678.43488.9f. PMID 16141411. Unknown parameter
|month=ignored (help) - ↑ Costet, P.; Luo, Y.; Wang, N.; Tall, AR. (2000). "Sterol-dependent transactivation of the ABC1 promoter by the liver X receptor/retinoid X receptor". J Biol Chem. 275 (36): 28240–5. doi:10.1074/jbc.M003337200. PMID 10858438. Unknown parameter
|month=ignored (help) - ↑ Brunham, LR.; Kruit, JK.; Iqbal, J.; Fievet, C.; Timmins, JM.; Pape, TD.; Coburn, BA.; Bissada, N.; Staels, B. (2006). "Intestinal ABCA1 directly contributes to HDL biogenesis in vivo". J Clin Invest. 116 (4): 1052–62. doi:10.1172/JCI27352. PMID 16543947. Unknown parameter
|month=ignored (help) - ↑ Repa, JJ.; Liang, G.; Ou, J.; Bashmakov, Y.; Lobaccaro, JM.; Shimomura, I.; Shan, B.; Brown, MS.; Goldstein, JL. (2000). "Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRalpha and LXRbeta". Genes Dev. 14 (22): 2819–30. PMID 11090130. Unknown parameter
|month=ignored (help) - ↑ Quinet, EM.; Savio, DA.; Halpern, AR.; Chen, L.; Schuster, GU.; Gustafsson, JA.; Basso, MD.; Nambi, P. (2006). "Liver X receptor (LXR)-beta regulation in LXRalpha-deficient mice: implications for therapeutic targeting". Mol Pharmacol. 70 (4): 1340–9. doi:10.1124/mol.106.022608. PMID 16825483. Unknown parameter
|month=ignored (help) - ↑ 45.0 45.1 Yasuda, T.; Grillot, D.; Billheimer, JT.; Briand, F.; Delerive, P.; Huet, S.; Rader, DJ. (2010). "Tissue-specific liver X receptor activation promotes macrophage reverse cholesterol transport in vivo". Arterioscler Thromb Vasc Biol. 30 (4): 781–6. doi:10.1161/ATVBAHA.109.195693. PMID 20110577. Unknown parameter
|month=ignored (help) - ↑ Katz, A.; Udata, C.; Ott, E.; Hickey, L.; Burczynski, ME.; Burghart, P.; Vesterqvist, O.; Meng, X. (2009). "Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants". J Clin Pharmacol. 49 (6): 643–9. doi:10.1177/0091270009335768. PMID 19398602. Unknown parameter
|month=ignored (help) - ↑ 47.0 47.1 Bradley, MN.; Hong, C.; Chen, M.; Joseph, SB.; Wilpitz, DC.; Wang, X.; Lusis, AJ.; Collins, A.; Hseuh, WA. (2007). "Ligand activation of LXR beta reverses atherosclerosis and cellular cholesterol overload in mice lacking LXR alpha and apoE". J Clin Invest. 117 (8): 2337–46. doi:10.1172/JCI31909. PMID 17657314. Unknown parameter
|month=ignored (help) - ↑ Peng, D.; Hiipakka, RA.; Xie, JT.; Dai, Q.; Kokontis, JM.; Reardon, CA.; Getz, GS.; Liao, S. (2011). "A novel potent synthetic steroidal liver X receptor agonist lowers plasma cholesterol and triglycerides and reduces atherosclerosis in LDLR(-/-) mice". Br J Pharmacol. 162 (8): 1792–804. doi:10.1111/j.1476-5381.2011.01202.x. PMID 21232031. Unknown parameter
|month=ignored (help) - ↑ Griffett, K.; Solt, LA.; El-Gendy, Bel-D.; Kamenecka, TM.; Burris, TP. (2013). "A liver-selective LXR inverse agonist that suppresses hepatic steatosis". ACS Chem Biol. 8 (3): 559–67. doi:10.1021/cb300541g. PMID 23237488. Unknown parameter
|month=ignored (help) - ↑ 50.0 50.1 Mencarelli, A.; Fiorucci, S. (2010). "FXR an emerging therapeutic target for the treatment of atherosclerosis". J Cell Mol Med. 14 (1–2): 79–92. doi:10.1111/j.1582-4934.2009.00997.x. PMID 20041971. Unknown parameter
|month=ignored (help) - ↑ Hambruch, E.; Miyazaki-Anzai, S.; Hahn, U.; Matysik, S.; Boettcher, A.; Perović-Ottstadt, S.; Schlüter, T.; Kinzel, O.; Krol, HD. (2012). "Synthetic farnesoid X receptor agonists induce high-density lipoprotein-mediated transhepatic cholesterol efflux in mice and monkeys and prevent atherosclerosis in cholesteryl ester transfer protein transgenic low-density lipoprotein receptor (-/-) mice". J Pharmacol Exp Ther. 343 (3): 556–67. doi:10.1124/jpet.112.196519. PMID 22918042. Unknown parameter
|month=ignored (help) - ↑ Plump, AS.; Scott, CJ.; Breslow, JL. (1994). "Human apolipoprotein A-I gene expression increases high density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse". Proc Natl Acad Sci U S A. 91 (20): 9607–11. PMID 7937814. Unknown parameter
|month=ignored (help) - ↑ Gaudet, D.; Méthot, J.; Déry, S.; Brisson, D.; Essiembre, C.; Tremblay, G.; Tremblay, K.; de Wal, J.; Twisk, J. (2013). "Efficacy and long-term safety of alipogene tiparvovec (AAV1-LPLS447X) gene therapy for lipoprotein lipase deficiency: an open-label trial". Gene Ther. 20 (4): 361–9. doi:10.1038/gt.2012.43. PMID 22717743. Unknown parameter
|month=ignored (help) - ↑ Marquart, TJ.; Allen, RM.; Ory, DS.; Baldán, A. (2010). "miR-33 links SREBP-2 induction to repression of sterol transporters". Proc Natl Acad Sci U S A. 107 (27): 12228–32. doi:10.1073/pnas.1005191107. PMID 20566875. Unknown parameter
|month=ignored (help)