Heart murmur pathophysiology: Difference between revisions
No edit summary |
|||
| Line 39: | Line 39: | ||
|[[mitral stenosis]] | |[[mitral stenosis]] | ||
| | | | ||
* Mitral stenosis ([[MS]]) is most commonly secondary to acute [[rheumatic fever]]. Generally, the initial [[valvulitis]] is associated with [[valvular]] [[regurgitation]] then over the years, the [[commissures]] fuse and the valves thicken and calcify.<ref name="pmid14879491">{{cite journal| author=BLAND EF, DUCKETT JONES T| title=Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood. | journal=Circulation | year= 1951 | volume= 4 | issue= 6 | pages= 836-43 | pmid=14879491 | doi= | pmc= | url= }}</ref> | *Mitral stenosis ([[MS]]) is most commonly secondary to acute [[rheumatic fever]]. Generally, the initial [[valvulitis]] is associated with [[valvular]] [[regurgitation]] then over the years, the [[commissures]] fuse and the valves thicken and calcify.<ref name="pmid14879491">{{cite journal| author=BLAND EF, DUCKETT JONES T| title=Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood. | journal=Circulation | year= 1951 | volume= 4 | issue= 6 | pages= 836-43 | pmid=14879491 | doi= | pmc= | url= }}</ref> | ||
* Usually, the rate of decrement in the valve area is about 0.1 cm<sup>2</sup>/year once mitral stenosis is present.<ref name="pmid1552121">{{cite journal| author=Gordon SP, Douglas PS, Come PC, Manning WJ| title=Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up. | journal=J Am Coll Cardiol | year= 1992 | volume= 19 | issue= 5 | pages= 968-73 | pmid=1552121 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1552121 }}</ref><ref name="pmid8800128">{{cite journal| author=Sagie A, Freitas N, Padial LR, Leavitt M, Morris E, Weyman AE et al.| title=Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease. | journal=J Am Coll Cardiol | year= 1996 | volume= 28 | issue= 2 | pages= 472-9 | pmid=8800128 | doi=10.1016/0735-1097(96)00153-2 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8800128 }}</ref> | *Usually, the rate of decrement in the valve area is about 0.1 cm<sup>2</sup>/year once mitral stenosis is present.<ref name="pmid1552121">{{cite journal| author=Gordon SP, Douglas PS, Come PC, Manning WJ| title=Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up. | journal=J Am Coll Cardiol | year= 1992 | volume= 19 | issue= 5 | pages= 968-73 | pmid=1552121 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1552121 }}</ref><ref name="pmid8800128">{{cite journal| author=Sagie A, Freitas N, Padial LR, Leavitt M, Morris E, Weyman AE et al.| title=Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease. | journal=J Am Coll Cardiol | year= 1996 | volume= 28 | issue= 2 | pages= 472-9 | pmid=8800128 | doi=10.1016/0735-1097(96)00153-2 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8800128 }}</ref> | ||
* When the cross sectional area is about 2 cm<sup>2</sup> called Mild Mitral Stenosis.<ref name="MS">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | *When the cross sectional area is about 2 cm<sup>2</sup> called Mild Mitral Stenosis.<ref name="MS">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | ||
* When the cross sectional area goes below 2 cm<sup>2</sup>: | *When the cross sectional area goes below 2 cm<sup>2</sup>: | ||
** there will be impediment to the flow of blood into the left ventricle, creating a pressure gradient that increased by increases in the [[heart rate]] or [[cardiac output]]. | **there will be impediment to the flow of blood into the left ventricle, creating a pressure gradient that increased by increases in the [[heart rate]] or [[cardiac output]]. | ||
** The [[atrial kick]] is required to fill the left ventricle with blood when the valve is so tight and the gradient is so high. | **The [[atrial kick]] is required to fill the left ventricle with blood when the valve is so tight and the gradient is so high. | ||
** When the heart rate goes above a certain point, the diastolic filling period is insufficient to fill the ventricle with blood and pressure builds up in the [[left atrium]], leading to [[pulmonary congestion]].<ref name="MS2">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | **When the heart rate goes above a certain point, the diastolic filling period is insufficient to fill the ventricle with blood and pressure builds up in the [[left atrium]], leading to [[pulmonary congestion]].<ref name="MS2">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | ||
* When the mitral valve area goes less than 1 cm<sup>2</sup>: | *When the mitral valve area goes less than 1 cm<sup>2</sup>: | ||
** the pressure gradient across the mitral valve will be 20 mm Hg and the left atrial pressure about 25 mm Hg. | **the pressure gradient across the mitral valve will be 20 mm Hg and the left atrial pressure about 25 mm Hg. | ||
** This left atrial pressure causes an elevated [[pulmonary capillary wedge pressure]], [[congestive heart failure]] and [[pulmonary edema]]. | **This left atrial pressure causes an elevated [[pulmonary capillary wedge pressure]], [[congestive heart failure]] and [[pulmonary edema]]. | ||
** The pressure overload of the [[left atrium]] will cause the left atrium to increase in size. make it more prone to develop [[atrial fibrillation]]. When atrial fibrillation develops, the [[atrial kick]] is lost.<ref name="pmid8043061">{{cite journal| author=Marcus RH, Sareli P, Pocock WA, Barlow JB| title=The spectrum of severe rheumatic mitral valve disease in a developing country. Correlations among clinical presentation, surgical pathologic findings, and hemodynamic sequelae. | journal=Ann Intern Med | year= 1994 | volume= 120 | issue= 3 | pages= 177-83 | pmid=8043061 | doi= | pmc= | url= }}</ref><ref name="MS3">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | **The pressure overload of the [[left atrium]] will cause the left atrium to increase in size. make it more prone to develop [[atrial fibrillation]]. When atrial fibrillation develops, the [[atrial kick]] is lost.<ref name="pmid8043061">{{cite journal| author=Marcus RH, Sareli P, Pocock WA, Barlow JB| title=The spectrum of severe rheumatic mitral valve disease in a developing country. Correlations among clinical presentation, surgical pathologic findings, and hemodynamic sequelae. | journal=Ann Intern Med | year= 1994 | volume= 120 | issue= 3 | pages= 177-83 | pmid=8043061 | doi= | pmc= | url= }}</ref><ref name="MS3">Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016</ref> | ||
|- | |- | ||
|[[mitral regurgitation]] | |[[mitral regurgitation]] | ||
| | | | ||
* Acute [[Mitral regurgitation|Mitral Regurgitation]] <ref name="pmid37425242">{{cite journal| author=Kusiak V, Brest AN| title=Acute mitral regurgitation: pathophysiology and management. | journal=Cardiovasc Clin | year= 1986 | volume= 16 | issue= 2 | pages= 257-80 | pmid=3742524 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3742524 }}</ref> | |||
** Develop when there is sudden disruption of one or more of the components of the [[mitral valve]], such as leaflet perforation, rupture of a [[chordae tendineae]], or rupture of the [[papillary muscle]]. | |||
** In the acute setting, the total stroke volume is increased, but the forward cardiac output into the [[aorta]] is decreased because a proportion of the blood is going backward into the [[left atrium]]. | |||
** [[Pulmonary congestion]] and [[hypoxia]] occur in acute [[Mitral regurgitation|MR]] causes a sudden volume overload of both the [[left atrium]] and the [[left ventricle]]. | |||
*Chronic Compensated [[mitral regurgitation]]: <ref name="pmid24603192">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Am Coll Cardiol | year= 2014 | volume= 63 | issue= 22 | pages= 2438-88 | pmid=24603192 | doi=10.1016/j.jacc.2014.02.537 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24603192 }}</ref> | |||
**Develops slowly and the [[left ventricle]] develops eccentric hypertrophy to reduce the wall stress associated with the rise in total [[stroke volume]]. | |||
**In the [[left atrium]], the chronic volume overload causes [[left atrial enlargement]], allowing the filling pressure in the [[left atrium]] to decrease and reduces the [[pulmonary capillary wedge pressure]]. | |||
*Chronic decompensated [[mitral regurgitation]]:<ref name="pmid246031922">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Am Coll Cardiol | year= 2014 | volume= 63 | issue= 22 | pages= 2438-88 | pmid=24603192 | doi=10.1016/j.jacc.2014.02.537 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24603192 }}</ref> | |||
**In this phase, the ventricular myocardium is no longer able to contract adequately to compensate for the volume overload of MR, and the [[stroke volume]] of the left ventricle begins to decrease. The reduced [[stroke volume]] causes a decrease in the forward [[cardiac output]] and an increase in the [[systole|end-systolic]] volume. | |||
**The increased left ventricular end-systolic volume in turn causes increased left ventricular end diastolic pressures and increased pulmonary capillary wedge pressures. | |||
**As the wedge pressure rises, the patient may develop symptoms of [[congestive heart failure]] such as [[dyspnea]], [[PND]] and [[orthopnea]] and signs of congestive heart failure including [[rales]]. | |||
|} | |} | ||
Revision as of 17:57, 28 January 2021
|
Heart murmur Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Heart murmur pathophysiology On the Web |
|
American Roentgen Ray Society Images of Heart murmur pathophysiology |
|
Risk calculators and risk factors for Heart murmur pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Nuha Al-Howthi, MD[2]
Overview
Turbulent flow is responsible for most murmurs. Turbulent flow occurs when the velocity of blood flow becomes critically high because of a high volume of flow, the flow goes through an irregular or narrow area, the flow empties into a dilated vessel or chamber, or if the flow goes backward through an incompetent valve, septal defect, or patent ductus arteriosus. Frequently, a combination of these factors is operative. The sounds most commonly originate from the abnormal movement of blood across valves and between cardiac chambers. When this occurs, turbulence results, which produces vibrations in the chambers of the heart or outflow vessels that are detected as Murmurs.
summery of pathophysiology
| pathophysiology | |
|---|---|
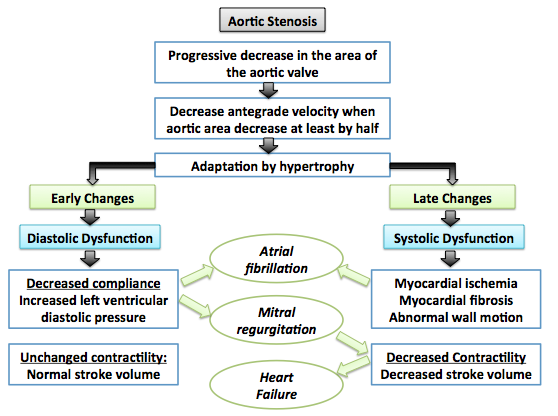
| aortic stenosis |
 |
| aortic regurgitation | ==Pathophysiology==
Normally, the aortic valve is only open when the pressure in the left ventricle exceeds the pressure in the aorta. This allows the blood to be ejected from the left ventricle into the aorta during ventricular systole. The amount of blood that is ejected by the heart is known as the stroke volume. Under normal conditions, 50–70% of the blood in a filled left ventricle is ejected into the aorta to be used by the body (called the ejection fraction). In aortic insufficiency (AI), when the pressure in the left ventricle falls below the pressure in the aorta, the aortic valve leaks, and the blood flows from the aorta into the left ventricle. As a result there is volume overload of the left ventricle.[5] [6]
Acute PathophysiologyIn acute aortic insufficiency, there is a sudden decrease in stroke volume and subsequent increase in left ventricular end diastolic volume thereby causing decrease cardiac output with resultant reflex tachycardia. The sharply rising high left ventricular end diastolic pressure and reflex tachycardia causes profound hypotension and cardiogenic shock. Initially, the rising left ventricle end diastolic pressure causes early closure of mitral valve during diastole thereby preventing backward blood flow. But in severe cases, the rapidly rising left ventricular end diastolic pressure equalizes with the aortic end-diastolic pressure leading to backward flow of blood progressing towards development of pulmonary edema.[7][8] [6] Chronic PathophysiologyIn chronic aortic insufficiency, initially the left ventricle remains complaint, thereby compensates for increased left ventricular end diastolic volume by progressive left ventricular dilatation and left ventricular hypertrophy, which maintains normal ratio of wall thickness to the cavity radius, thereby maintaining normal wall stress. Overtime, when the left ventricular hypertrophy fails to keep up with chronic volume overload, end systolic wall stress rises and at this point the left ventricle fails and results in left ventricle decompensation causing reduction in the left ventricular wall compliance with resultant congestive heart failure.[9][10] [11] |
| mitral stenosis |
|
| mitral regurgitation |
|
References
- ↑ Galli D, Manuguerra R, Monaco R, Manotti L, Goldoni M, Becchi G; et al. (2016). "Understanding the structural features of symptomatic calcific aortic valve stenosis: A broad-spectrum clinicopathologic study in 236 consecutive surgical cases". Int J Cardiol. 228: 364–374. doi:10.1016/j.ijcard.2016.11.180. PMID 27866029.
- ↑ Joseph J, Naqvi SY, Giri J, Goldberg S (2016). "Aortic stenosis: pathophysiology, diagnosis and therapy". Am J Med. doi:10.1016/j.amjmed.2016.10.005. PMID 27810479.
- ↑ Otto CM, Prendergast B (2014). "Aortic-valve stenosis--from patients at risk to severe valve obstruction". N Engl J Med. 371 (8): 744–56. doi:10.1056/NEJMra1313875. PMID 25140960.
- ↑ 4.0 4.1 Dweck MR, Boon NA, Newby DE (2012). "Calcific aortic stenosis: a disease of the valve and the myocardium". J Am Coll Cardiol. 60 (19): 1854–63. doi:10.1016/j.jacc.2012.02.093. PMID 23062541.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Thorac Cardiovasc Surg. 148 (1): e1–e132. doi:10.1016/j.jtcvs.2014.05.014. PMID 24939033.
- ↑ 6.0 6.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): e57–185. doi:10.1016/j.jacc.2014.02.536. PMID 24603191.
- ↑ Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ Mokadam NA, Stout KK, Verrier ED (2011). "Management of acute regurgitation in left-sided cardiac valves". Tex Heart Inst J. 38 (1): 9–19. PMC 3060740. PMID 21423463.
- ↑ Enriquez-Sarano M, Tajik AJ (2004). "Clinical practice. Aortic regurgitation". N Engl J Med. 351 (15): 1539–46. doi:10.1056/NEJMcp030912. PMID 15470217.
- ↑ Devlin WH, Petrusha J, Briesmiester K, Montgomery D, Starling MR (1999). "Impact of vascular adaptation to chronic aortic regurgitation on left ventricular performance". Circulation. 99 (8): 1027–33. PMID 10051296.
- ↑ Nishimura, RA. (2002). "Cardiology patient pages. Aortic valve disease". Circulation. 106 (7): 770–2. PMID 12176943. Unknown parameter
|month=ignored (help) - ↑ BLAND EF, DUCKETT JONES T (1951). "Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood". Circulation. 4 (6): 836–43. PMID 14879491.
- ↑ Gordon SP, Douglas PS, Come PC, Manning WJ (1992). "Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up". J Am Coll Cardiol. 19 (5): 968–73. PMID 1552121.
- ↑ Sagie A, Freitas N, Padial LR, Leavitt M, Morris E, Weyman AE; et al. (1996). "Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease". J Am Coll Cardiol. 28 (2): 472–9. doi:10.1016/0735-1097(96)00153-2. PMID 8800128.
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Marcus RH, Sareli P, Pocock WA, Barlow JB (1994). "The spectrum of severe rheumatic mitral valve disease in a developing country. Correlations among clinical presentation, surgical pathologic findings, and hemodynamic sequelae". Ann Intern Med. 120 (3): 177–83. PMID 8043061.
- ↑ Circulation http://circ.ahajournals.org/content/112/3/43November (2016) Accessed on November 22, 2016
- ↑ Kusiak V, Brest AN (1986). "Acute mitral regurgitation: pathophysiology and management". Cardiovasc Clin. 16 (2): 257–80. PMID 3742524.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): 2438–88. doi:10.1016/j.jacc.2014.02.537. PMID 24603192.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): 2438–88. doi:10.1016/j.jacc.2014.02.537. PMID 24603192.