Heart murmur pathophysiology: Difference between revisions
No edit summary |
|||
| Line 27: | Line 27: | ||
|- | |- | ||
|[[aortic regurgitation]] | |[[aortic regurgitation]] | ||
| | |==Pathophysiology== | ||
Normally, the [[aortic valve]] is only open when the pressure in the [[left ventricle]] exceeds the pressure in the [[aorta]]. This allows the [[blood]] to be ejected from the [[left ventricle]] into the [[aorta]] during ventricular systole. The amount of [[blood]] that is ejected by the [[heart]] is known as the [[stroke volume]]. Under normal conditions, 50–70% of the [[blood]] in a filled [[left ventricle]] is ejected into the [[aorta]] to be used by the body (called the [[ejection fraction]]). In aortic insufficiency (AI), when the pressure in the [[left ventricle]] falls below the pressure in the [[aorta]], the [[aortic valve]] leaks, and the [[blood]] flows from the [[aorta]] into the [[left ventricle]]. As a result there is volume overload of the [[left ventricle]].<ref name="pmid24939033">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Thorac Cardiovasc Surg | year= 2014 | volume= 148 | issue= 1 | pages= e1-e132 | pmid=24939033 | doi=10.1016/j.jtcvs.2014.05.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24939033 }} </ref> <ref name="pmid24603191">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Am Coll Cardiol | year= 2014 | volume= 63 | issue= 22 | pages= e57-185 | pmid=24603191 | doi=10.1016/j.jacc.2014.02.536 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24603191 }} </ref> | |||
===Acute Pathophysiology=== | |||
In acute aortic insufficiency, there is a sudden decrease in [[stroke volume]] and subsequent increase in left ventricular end diastolic volume thereby causing decrease [[cardiac output]] with resultant reflex [[tachycardia]]. The sharply rising high left ventricular end diastolic pressure and reflex [[tachycardia]] causes profound [[hypotension]] and [[cardiogenic shock]]. Initially, the rising left ventricle end diastolic pressure causes early closure of [[mitral valve]] during [[diastole]] thereby preventing backward blood flow. But in severe cases, the rapidly rising left ventricular end diastolic pressure equalizes with the aortic end-diastolic pressure leading to backward flow of [[blood]] progressing towards development of [[pulmonary edema]].<ref name="pmid19564568">{{cite journal| author=Stout KK, Verrier ED| title=Acute valvular regurgitation. | journal=Circulation | year= 2009 | volume= 119 | issue= 25 | pages= 3232-41 | pmid=19564568 | doi=10.1161/CIRCULATIONAHA.108.782292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19564568 }} </ref><ref name="pmid21423463">{{cite journal| author=Mokadam NA, Stout KK, Verrier ED| title=Management of acute regurgitation in left-sided cardiac valves. | journal=Tex Heart Inst J | year= 2011 | volume= 38 | issue= 1 | pages= 9-19 | pmid=21423463 | doi= | pmc=3060740 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21423463 }} </ref> <ref name="pmid24603191">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Am Coll Cardiol | year= 2014 | volume= 63 | issue= 22 | pages= e57-185 | pmid=24603191 | doi=10.1016/j.jacc.2014.02.536 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24603191 }} </ref> | |||
===Chronic Pathophysiology=== | |||
In chronic aortic insufficiency, initially the [[left ventricle]] remains complaint, thereby compensates for increased left ventricular end diastolic volume by progressive left ventricular dilatation and [[left ventricular hypertrophy]], which maintains normal ratio of wall thickness to the cavity radius, thereby maintaining normal wall stress. Overtime, when the [[left ventricular hypertrophy]] fails to keep up with chronic volume overload, end systolic wall stress rises and at this point the [[left ventricle]] fails and results in [[left ventricle]] decompensation causing reduction in the left ventricular wall compliance with resultant [[congestive heart failure]].<ref name="pmid15470217">{{cite journal| author=Enriquez-Sarano M, Tajik AJ| title=Clinical practice. Aortic regurgitation. | journal=N Engl J Med | year= 2004 | volume= 351 | issue= 15 | pages= 1539-46 | pmid=15470217 | doi=10.1056/NEJMcp030912 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15470217 }} </ref><ref name="pmid10051296">{{cite journal| author=Devlin WH, Petrusha J, Briesmiester K, Montgomery D, Starling MR| title=Impact of vascular adaptation to chronic aortic regurgitation on left ventricular performance. | journal=Circulation | year= 1999 | volume= 99 | issue= 8 | pages= 1027-33 | pmid=10051296 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10051296 }} </ref> <ref name="Nishimura-2002">{{Cite journal | last1 = Nishimura | first1 = RA. | title = Cardiology patient pages. Aortic valve disease. | journal = Circulation | volume = 106 | issue = 7 | pages = 770-2 | month = Aug | year = 2002 | doi = | PMID = 12176943 }}</ref> | |||
|- | |- | ||
|[[mitral stenosis]] | |[[mitral stenosis]] | ||
Revision as of 16:41, 28 January 2021
|
Heart murmur Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Heart murmur pathophysiology On the Web |
|
American Roentgen Ray Society Images of Heart murmur pathophysiology |
|
Risk calculators and risk factors for Heart murmur pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Nuha Al-Howthi, MD[2]
Overview
Turbulent flow is responsible for most murmurs. Turbulent flow occurs when the velocity of blood flow becomes critically high because of a high volume of flow, the flow goes through an irregular or narrow area, the flow empties into a dilated vessel or chamber, or if the flow goes backward through an incompetent valve, septal defect, or patent ductus arteriosus. Frequently, a combination of these factors is operative. The sounds most commonly originate from the abnormal movement of blood across valves and between cardiac chambers. When this occurs, turbulence results, which produces vibrations in the chambers of the heart or outflow vessels that are detected as Murmurs.
summery of pathophysiology
| pathophysiology | |
|---|---|
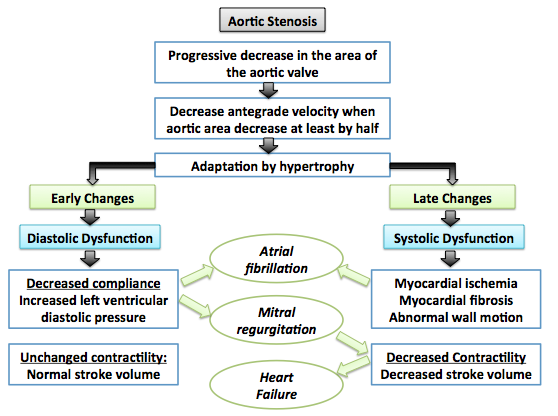
| aortic stenosis |
 |
| aortic regurgitation | ==Pathophysiology==
Normally, the aortic valve is only open when the pressure in the left ventricle exceeds the pressure in the aorta. This allows the blood to be ejected from the left ventricle into the aorta during ventricular systole. The amount of blood that is ejected by the heart is known as the stroke volume. Under normal conditions, 50–70% of the blood in a filled left ventricle is ejected into the aorta to be used by the body (called the ejection fraction). In aortic insufficiency (AI), when the pressure in the left ventricle falls below the pressure in the aorta, the aortic valve leaks, and the blood flows from the aorta into the left ventricle. As a result there is volume overload of the left ventricle.[5] [6]
Acute PathophysiologyIn acute aortic insufficiency, there is a sudden decrease in stroke volume and subsequent increase in left ventricular end diastolic volume thereby causing decrease cardiac output with resultant reflex tachycardia. The sharply rising high left ventricular end diastolic pressure and reflex tachycardia causes profound hypotension and cardiogenic shock. Initially, the rising left ventricle end diastolic pressure causes early closure of mitral valve during diastole thereby preventing backward blood flow. But in severe cases, the rapidly rising left ventricular end diastolic pressure equalizes with the aortic end-diastolic pressure leading to backward flow of blood progressing towards development of pulmonary edema.[7][8] [6] Chronic PathophysiologyIn chronic aortic insufficiency, initially the left ventricle remains complaint, thereby compensates for increased left ventricular end diastolic volume by progressive left ventricular dilatation and left ventricular hypertrophy, which maintains normal ratio of wall thickness to the cavity radius, thereby maintaining normal wall stress. Overtime, when the left ventricular hypertrophy fails to keep up with chronic volume overload, end systolic wall stress rises and at this point the left ventricle fails and results in left ventricle decompensation causing reduction in the left ventricular wall compliance with resultant congestive heart failure.[9][10] [11] |
| mitral stenosis | |
| mitral regurgitation |
References
- ↑ Galli D, Manuguerra R, Monaco R, Manotti L, Goldoni M, Becchi G; et al. (2016). "Understanding the structural features of symptomatic calcific aortic valve stenosis: A broad-spectrum clinicopathologic study in 236 consecutive surgical cases". Int J Cardiol. 228: 364–374. doi:10.1016/j.ijcard.2016.11.180. PMID 27866029.
- ↑ Joseph J, Naqvi SY, Giri J, Goldberg S (2016). "Aortic stenosis: pathophysiology, diagnosis and therapy". Am J Med. doi:10.1016/j.amjmed.2016.10.005. PMID 27810479.
- ↑ Otto CM, Prendergast B (2014). "Aortic-valve stenosis--from patients at risk to severe valve obstruction". N Engl J Med. 371 (8): 744–56. doi:10.1056/NEJMra1313875. PMID 25140960.
- ↑ 4.0 4.1 Dweck MR, Boon NA, Newby DE (2012). "Calcific aortic stenosis: a disease of the valve and the myocardium". J Am Coll Cardiol. 60 (19): 1854–63. doi:10.1016/j.jacc.2012.02.093. PMID 23062541.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Thorac Cardiovasc Surg. 148 (1): e1–e132. doi:10.1016/j.jtcvs.2014.05.014. PMID 24939033.
- ↑ 6.0 6.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): e57–185. doi:10.1016/j.jacc.2014.02.536. PMID 24603191.
- ↑ Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ Mokadam NA, Stout KK, Verrier ED (2011). "Management of acute regurgitation in left-sided cardiac valves". Tex Heart Inst J. 38 (1): 9–19. PMC 3060740. PMID 21423463.
- ↑ Enriquez-Sarano M, Tajik AJ (2004). "Clinical practice. Aortic regurgitation". N Engl J Med. 351 (15): 1539–46. doi:10.1056/NEJMcp030912. PMID 15470217.
- ↑ Devlin WH, Petrusha J, Briesmiester K, Montgomery D, Starling MR (1999). "Impact of vascular adaptation to chronic aortic regurgitation on left ventricular performance". Circulation. 99 (8): 1027–33. PMID 10051296.
- ↑ Nishimura, RA. (2002). "Cardiology patient pages. Aortic valve disease". Circulation. 106 (7): 770–2. PMID 12176943. Unknown parameter
|month=ignored (help)