Erythema gyratum repens: Difference between revisions
Hudakarman (talk | contribs) No edit summary |
|||
| Line 8: | Line 8: | ||
==Overview== | ==Overview== | ||
Erythema gyratum repens is a rare highly specific and characteristic [[para-neoplastic]] [[syndrome]] that usually affect older people. It is characterized by [[wood]]-[[grain]] scaly skin eruption with intense [[pruritus]]. The cause of erythema gyratum repens is unknown but many theories suggest [[immunologic]] etiology or toxicologic products that are released by the associated tumor. The first case of erythema gyratum repens was described by a dermatologist named Gammel in the year 1952. For many decades after erythema gyratum repens original description, there was little progress in defining the [[pathogenesis]] of erythema gyratum repens. Erythema gyratum repens has no specific classification but we can classify it based on its association with an internal malignancy into [[para-neoplastic]] and [[non-para-neoplastic]] erythema gyratum repens. The most common malignancies associated with erythema gyratum repens are [[lung]] or [[bronchogenic]] cancer, [[esophageal]] [[cancer]], and [[breast cancer]]. Erythema gyratum repens can also be associated with non-neoplastic diseases as [[tuberculosis]], [[autoimmune]] disorders, or [[CREST syndrome]]. Erythema gyratum repens is characterized by its pathogonomic [[figurate]], [[gyrate]], or [[annular]] erythematous skin [[eruptions]]. The intense [[pruritus]] can be debilitating and usually urges the patient to go to the emergency department. The [[microscopic]] [[histopathological]] features of erythema gyratum repens consist of [[acanthosis]], [[focal parakeratotic]], and [[spongiosis]] of the epidermis with [[perivascular]] [[mononuclear]], [[lymphocytic]], and [[histiocytic]] [[infiltrate]] in the superficial plexus of the dermis. Erythema gyratum repens is very rare and it mainly affects people in their seventieth decade, the male to female ratio is 2:1. Erythema gyratum repens is diagnosed clinically by its characteristic skin eruption and an urgent thorough paraneoplastic workup should be initiated to look for internal malignancies. Patients with erythema gyratum repens presents with intensely pruritic, gradually progressive, skin lesions that crawl rather than migrate from one body region to the other. It can start in the upper trunk or upper back and extends to involve the extremities sparing the face. The mainstay of the treatment of erythema gyratum repens is finding and treating the underlying malignancy. Symptomatic treatment is not very effective in relieving the pruritus and its associated pain. The management can be [[surgica]]l removal of the tumor, [[chemotherapy]], or [[palliative]] [[conservative]] management. The skin eruptions can improve completely after the removal of the underlying tumor, or can recur especially if the tumor recurred or metastasized. Patients can live a few weeks, months or up to five years depending on when and at what stage the [[malignancy]] was discovered. | Erythema gyratum repens is a rare highly specific and characteristic [[para-neoplastic]] [[syndrome]] that usually affect older people. It is characterized by [[wood]]-[[grain]] scaly skin eruption with intense [[pruritus]]. The cause of erythema gyratum repens is unknown but many theories suggest [[immunologic]] etiology or toxicologic products that are released by the associated tumor. The first case of erythema gyratum repens was described by a dermatologist named Gammel in the year 1952. For many decades after erythema gyratum repens original description, there was little progress in defining the [[pathogenesis]] of erythema gyratum repens. Erythema gyratum repens has no specific classification but we can classify it based on its association with an internal [[malignancy]] into [[para-neoplastic]] and [[non-para-neoplastic]] erythema gyratum repens. The most common [[malignancies]] associated with erythema gyratum repens are [[lung]] or [[bronchogenic]] cancer, [[esophageal]] [[cancer]], and [[breast cancer]]. Erythema gyratum repens can also be associated with non-neoplastic diseases as [[tuberculosis]], [[autoimmune]] disorders, or [[CREST syndrome]]. Erythema gyratum repens is characterized by its pathogonomic [[figurate]], [[gyrate]], or [[annular]] erythematous skin [[eruptions]]. The intense [[pruritus]] can be debilitating and usually urges the patient to go to the emergency department. The [[microscopic]] [[histopathological]] features of erythema gyratum repens consist of [[acanthosis]], [[focal parakeratotic]], and [[spongiosis]] of the epidermis with [[perivascular]] [[mononuclear]], [[lymphocytic]], and [[histiocytic]] [[infiltrate]] in the superficial plexus of the dermis. Erythema gyratum repens is very rare and it mainly affects people in their seventieth decade, the male to female ratio is 2:1. Erythema gyratum repens is diagnosed clinically by its characteristic skin eruption and an urgent thorough paraneoplastic workup should be initiated to look for internal malignancies. Patients with erythema gyratum repens presents with intensely pruritic, gradually progressive, skin lesions that crawl rather than migrate from one body region to the other. It can start in the upper trunk or upper back and extends to involve the extremities sparing the face. The mainstay of the treatment of erythema gyratum repens is finding and treating the underlying malignancy. Symptomatic treatment is not very effective in relieving the pruritus and its associated pain. The management can be [[surgica]]l removal of the tumor, [[chemotherapy]], or [[palliative]] [[conservative]] management. The skin eruptions can improve completely after the removal of the underlying tumor, or can recur especially if the tumor recurred or metastasized. Patients can live a few weeks, months or up to five years depending on when and at what stage the [[malignancy]] was discovered. | ||
==Historical Perspective== | ==Historical Perspective== | ||
Revision as of 18:32, 1 July 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Gammel's disease.
Overview
Erythema gyratum repens is a rare highly specific and characteristic para-neoplastic syndrome that usually affect older people. It is characterized by wood-grain scaly skin eruption with intense pruritus. The cause of erythema gyratum repens is unknown but many theories suggest immunologic etiology or toxicologic products that are released by the associated tumor. The first case of erythema gyratum repens was described by a dermatologist named Gammel in the year 1952. For many decades after erythema gyratum repens original description, there was little progress in defining the pathogenesis of erythema gyratum repens. Erythema gyratum repens has no specific classification but we can classify it based on its association with an internal malignancy into para-neoplastic and non-para-neoplastic erythema gyratum repens. The most common malignancies associated with erythema gyratum repens are lung or bronchogenic cancer, esophageal cancer, and breast cancer. Erythema gyratum repens can also be associated with non-neoplastic diseases as tuberculosis, autoimmune disorders, or CREST syndrome. Erythema gyratum repens is characterized by its pathogonomic figurate, gyrate, or annular erythematous skin eruptions. The intense pruritus can be debilitating and usually urges the patient to go to the emergency department. The microscopic histopathological features of erythema gyratum repens consist of acanthosis, focal parakeratotic, and spongiosis of the epidermis with perivascular mononuclear, lymphocytic, and histiocytic infiltrate in the superficial plexus of the dermis. Erythema gyratum repens is very rare and it mainly affects people in their seventieth decade, the male to female ratio is 2:1. Erythema gyratum repens is diagnosed clinically by its characteristic skin eruption and an urgent thorough paraneoplastic workup should be initiated to look for internal malignancies. Patients with erythema gyratum repens presents with intensely pruritic, gradually progressive, skin lesions that crawl rather than migrate from one body region to the other. It can start in the upper trunk or upper back and extends to involve the extremities sparing the face. The mainstay of the treatment of erythema gyratum repens is finding and treating the underlying malignancy. Symptomatic treatment is not very effective in relieving the pruritus and its associated pain. The management can be surgical removal of the tumor, chemotherapy, or palliative conservative management. The skin eruptions can improve completely after the removal of the underlying tumor, or can recur especially if the tumor recurred or metastasized. Patients can live a few weeks, months or up to five years depending on when and at what stage the malignancy was discovered.
Historical Perspective
- The association between cutaneous manifestations and systemic malignancies was first studied in 1925 by Rothman, the Hungarian investigative dermatologist, who wrote a comprehensive review on this subject and since then, cases were added to proof for the relationship between internal neoplasm and some skin lesions.[1][2]
- Erythema gyratum repens was first described by Dr. John A Gammel, the dermatologist, who was trained to link bizarre or recalcitrant dermatoses to internal malignancy, In 1952, in a 55-year-old patient who had been complaining of pruritic scaly skin eruption and diagnosed nine months later with poorly differentiated adenocarcinoma of the breast with metastasis to axillary lymph nodes.[3][4]
- In 1950, Dr. Gammel presented his case of Erythema gyratum repens before the Cleveland Dermatological Society as Erythema gyratum migrans then he changed the term to erythema gyratum repens because the eruption does not "migrate" from one place to another but "crawls" constantly in the areas involved, like "ants on an anthill".[3]
- In 1973, 45 year old man was diagnosed with erythema gyratum repens associated with metastatic, undifferentiated adenocarcinoma which was removed following a right- sided craniotomy. The patient was misdiagnosed with erythema perstans and the malignancy was discovered after 8 months of the skin manifestations.[5]
- Up to 1992, there were only 49 cases in the literature, 41 of which (84%) were associated with a neoplasm and that is why erythema gyratum repens has been considered as a paraneoplastic syndrome.[6]
- Between 1990 and 2010, a literature review was done by collecting data from the medical records of patients form dermatology department in University of Genoa and from databases as pubmed and medline, to conclude that erythema gyratum repens is no longer considered as an obligate paraneoplastic syndrome. More than expected cases of EGR were found with no neoplasm association.[7]
Classification
- Erythema gyratum repens has no established system for the classification. However, we can classify erythema gyratum repens based on its association with systemic malignancy as:
- Paraneoplastic erythema gyratum repens
- Erythema gyratum repens is associated with internal malignancy in 82% of cases.[7]
- Non-paraneoplastic erythema gyratum repens could be:
- Idiopathic erythema gyratum repens
- Erythema gyratum repens-like eruptions (different dermatologic lesions that mimic erythema gyratum repens).[8]
- Erythema gyratum repens with concomitant disease as:
- Pityriasis rubra pilaris, psoriasis, ichthyosis, CREST (calcinosis, Raynaud phenomenon, esophageal motility disorder, sclerodactyly, and telangiectasia) syndrome, rheumatoid arthritis, tuberculosis, bullous pemphigoid, linear IgA disease, and hypereosinophilic syndrome, cryptogenic organizing pneumonia, virginal breast hypertrophy.
- Drug-induced erythema gyratum repens examples are:
- Azathioprine with type I autoimmune hepatitis.[9]
- Interferon given for hepatitis C virus–related chronic hepatitis.[10]
- Paraneoplastic erythema gyratum repens
| Types of Erythema gyratum repens | Characterestics |
|---|---|
| Paraneoplastic EGR |
|
| Non-paraneoplastic EGR |
|
| Idiopathic EGR |
|
| EGR-like eruptions |
|
| EGR with concomittant skin disease |
|
| Drug-induced EGR |
|
Pathophysiology
- The pathogenesis of erythema gyratum repens is unclear[12][13]
- Many immunologic theories have been implicated in its pathogenesis.
- The immunologic mechanism theory is evidenced by the observed immunofluorescence patterns of IgG, C3, and C4 at the basement membrane: [13]
- Theory 1: the tumor induces antibodies that cross-react with the basement membrane of skin.
- Theory 2: the tumor produces polypeptides that bind skin antigens and render them immunogenic.
- Theory 3: deposition of tumor antigen-antibody complexes onto the basement membrane causes reactive dermatitis seen in EGR.
- The gross appearance of the unique eruptions are:
- Wavy erythematous concentric bands that can be figurate, gyrate, or annular
- The bands are arranged in parallel rings and lined by a fine trailing edge of scales, a pattern often described as “wood grained”.
- The distinctive wood-grain appearance of the eruption is pathognomonic.
- The rash typically involves large areas of the body but tends to spare the face, hands, and feet and it can expand as fast as 1 cm a day.
- Bullae can also form from within the areas of erythema.
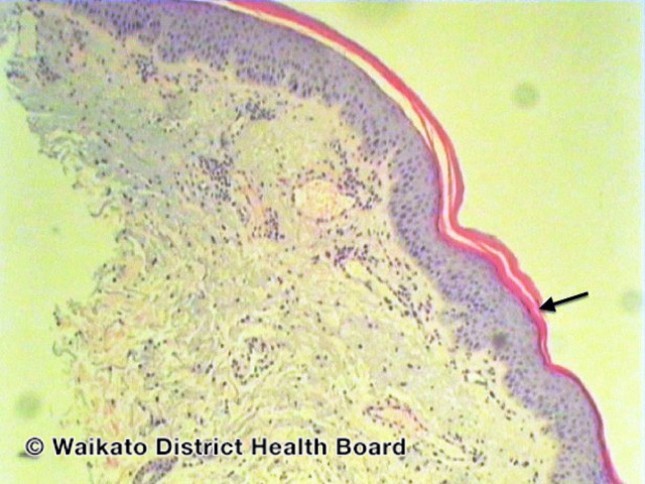
- The microscopic histologic features of erythema gyratum repens are not characteristics but the following are the biopsy specimen findings that are compatible with the diagnosis:[3][5][14]
- The epidermis has thin atrophic patches with areas of acanthosis, focal parakeratotic horny layers, and spongiosis.
- The dermis contains a moderate perivascular mononuclear, lymphocytic, and histiocytic infiltrate in the superficial plexus as well as mild focal spongiosis and parakeratosis.
- Eosinophils and melanophages have also been reported in the dermal infiltrate.
- Diffuse to moderate edema of the connective tissue can be seen.
Causes
- The exact cause of erythema gyratum repens is unknown.
- Various immunologic mechanisms suggest that erythema gyratum repens etiology is stemmed from an immunologic reaction.
- The association between erythema gyratum repens and systemic malignancy is evidenced by the disappearance of the pruritic eruptions after the treatment of the underlying neoplasm.
- The association doesn't necessarily mean causation.
Differentiating Erythema Gyratum Repens from Other Diseases
- EGR has a narrow differential diagnosis. It has to be differentiated from Reactive gyrate erythematous eruptions, such as:
| Disease | Erythema Characteristics | Signs and Symptoms | Associated Conditions | Histopathology | Lab finding
& Other evaluation |
prognosis |
|---|---|---|---|---|---|---|
| Erythema gyratum repens (EGR) |
|
|
(Calcinosis, Raynaud’s phenomenon, Esophageal Cysmotility, Sclerodactyly, and Telangiectasia) |
|
|
|
| Erythema annulare centrifugum (EAC) [14] |
or polycyclic lesions
|
|
|
|
|
|
| Necrolytic migratory erythema (NME) |
|
|
|
|
|
|
Epidemiology and Demographics
- Erythema gyratum repens is a rare, characteristic, and paraneoplastic syndrome with the following demographics:[13]
Age
- The average age of onset of erythema gyratum repens i is in the seventh decade of life (65 years old).
Gender
- The male to female ratio is 2:1.
Race
- EGR commonly affects Caucasians.
Risk Factors
- There are no established risk factors for erythyma gyratum repens.
- Many patients with erythyma gyratum repens and malignancy had a history of tobacco smoking.
- Some patients with erythyma gyratum repens and malignancy have a family history of neoplasm.
Screening
- There are no screening tests for EGR.
- Screening for internal malignancy should be done immediately after EGR is diagnosed.
Natural History, Complications, and Prognosis
- The majority of patients with EGR presents with severely pruritic erythematous skin lesions that appear several months prior to the malignancy diagnosis[13]
- If the underlying malignancy left untreated, the debilitating pruritus could persist until the patient dies[13]
- Prognosis depends on the type of the underlying tumor and the probability of its treatment. It depends on the time of the EGR onset and the neoplasm discovery. The course and prognosis of EGR can be one of the following:
- Complete cure of the skin eruption and pruritus after removal and treatment of the internal neoplasm.
- Temporary improvement then recurrence of the eruption (specially in cases of metastasis).
- No effect of the tumor treatment on the course of EGR.
- Death can occur few weeks after the discovery of the malignancy, few months, or four years as in Gammel's patient.
Diagnosis
Diagnostic Study of Choice
- Erythyma gyratum repens is mainly diagnosed clinically by its characteristic skin lesions.
- It is considered as a cutaneous marker of malignancy with high specificity so physicians shouldn't miss its unique clinical skin presentation.
History and Symptoms
- The universal symptoms of erythema gyratum repens are:
- Skin eruptions
- Intense pruritus
- Other symptoms related to the associated internal malignancy may include:
Physical Examination
- Patients with erythyma gyratum repens usually are ill-appearing and lethargic
- Physical examination may be remarkable for:
- Wood-grain erythematous scaly skin eruption.
- Bullae can also form within the areas of erythema.
- Typically involves large areas of the body but tends to spare the face, hands, and feet and it can expand as fast as 1 cm a day.[13]
- Signs of malignancy can be seen based on the neoplasm location such as:
Laboratory Findings
- There are no diagnostic laboratory findings associated with erythema gyratum repens.
- Eosinophilia is observed in 60% of cases.[13]
- Decreased T lymphocytes and increased B lymphocytes observed in an erythema gyratum repens patient with increased luteinizing hormone and follicle-stimulating hormone.[14]
- Decreased serum levels of C3.[14]
- Normal percentages of B and T lymphocytes and normal T-cell function were reported in an erythema gyratum repens patient without cancer.[14]
Imaging Findings
- There are no imaging findings associated with erythyma gyratum repens.
- Imaging to look for systemic neoplasms are:[13]
- * Computed tomography of the head, neck, chest, abdomen, and pelvis.
- Positron emission tomography/computed tomography
- Upper and lower gastrointestinal endoscopy
- The abnormal findings that heightened concern for systemic or widespread malignancy are:
- Brain, chest, lung, abdominal, peritoneal, or pelvic mass.
- Lymphadenopathy.
- Enhanced bone lucencies suggestive of diffuse metastasis.
Other Diagnostic Studies
- The histopathologic features of EGR is non-specific.
- Biopsy specimens show the following:[13]
- Acanthosis, mild hyperkeratosis, focal parakeratosis, and spongiosis confined to the epidermis and superficial dermis
- Mononuclear, lymphocytic, and histiocytic perivascular infiltrate in the superficial plexus can also be seen
- Eosinophils and melanophages have also been reported in the dermal infiltrate
- Diffuse to moderate edema of the connective tissue can be seen
- Direct immunofluorescence can show patterns of IgG, C3, and C4 at the basement membrane
- Thorough paraneoplastic and systemic workup includes:[13][16]
- Computed tomography of head, neck, chest, abdomen, and pelvis.
- Positron emission tomography/computed tomography.
- Upper and lower gastrointestinal endoscopy.
- Complete blood chemistry (CBC).
- Comprehensive metabolic panel (CMP).
- Urinanalysis.
- Rapid plasma reagin test [to exclude syphilis].
- Anti-nuclear antibody test [to exclude autoimmune disorders as systemic lupus erythematosus (SLE)].
- Guaiac stool test.
- Serum protein electrophoresis [to exclude cancers as multiple myeloma].
- Lactate dehydrogenase [tissue damage, kidney disease, liver disease].
- QuantiFERON [to exclude tuberculosis].
- Tumor markers.
Treatment
Medical Therapy
- Treatment of erythema gyratum repens, and its associated intense pruritus depends on the recognition and treatment of the underlying malignancy[13]
- Symptomatic management:
- Hydroxyzine for itching, ibuprofen and oxycodone for pain, and triamcinolone 0.1% cream for the rash.
- Management of the neoplasm depends on its type, location, stage, and time of its discovery and on patient preference:
- Surgical removal
- Chemotherapy
- Conservative palliative management
- Various dermatologic and immunosuppressive therapies have been used to treat EGR.
- Systemic steroids are frequently ineffective.
- Topical steroids, vitamin A, and azathioprine have also failed to relieve skin manifestations
Surgery
- Surgical resection of the discovered malignancy could be recommended as part of the management of Erythyma gyratum repens.
Prevention
- Primary prevention:
- There are no primary preventive measures available for erythema gyratum repens
- Secondary Prevention:
- If the thorough screening after Erythyma gyratum repens diagnosis detected the malignancy in its earliest stages.
- Tertiary prevention:
- If the thorough screening after Erythyma gyratum repens diagnosis detected the malignancy in its late stages or with widespread metastasis.
- Tertiary prevention aims to improve the quality of life and life expectancy.
References
- ↑ Rothman, Stephan (1925). "Über Hauterscheinungen bei bösartigen Geschwülsten innerer Organe". Archiv für Dermatologie und Syphilis. 149 (1): 99–123. doi:10.1007/BF02297811. ISSN 0340-3696.
- ↑ Burgdorf WHC, Bickers DR (2015). "The scientific legacy of Stephen Rothman". J Invest Dermatol. 135 (4): 954–959. doi:10.1038/jid.2014.447. PMC 4366295. PMID 25373439.
- ↑ 3.0 3.1 3.2 Gammel, John A. (1952). "ERYTHEMA GYRATUM REPENS". A.M.A. Archives of Dermatology and Syphilology. 66 (4): 494. doi:10.1001/archderm.1952.01530290070010. ISSN 0096-5979.
- ↑ Purdy, M. J. (1959). "Erythema Gyratum Repens". A.M.A. Archives of Dermatology. 80 (5): 590. doi:10.1001/archderm.1959.01560230076020. ISSN 0096-5359.
- ↑ 5.0 5.1 Skolnick, Marvin (1975). "Erythema Gyratum Repens With Metastatic Adenocarcinoma". Archives of Dermatology. 111 (2): 227. doi:10.1001/archderm.1975.01630140085011. ISSN 0003-987X.
- ↑ Boyd AS, Neldner KH, Menter A (1992). "Erythema gyratum repens: a paraneoplastic eruption". J Am Acad Dermatol. 26 (5 Pt 1): 757–62. PMID 1583177.
- ↑ 7.0 7.1 7.2 Rongioletti, F.; Fausti, V.; Parodi, A. (2014). "Erythema gyratum repens is not an obligate paraneoplastic disease: a systematic review of the literature and personal experience". Journal of the European Academy of Dermatology and Venereology. 28 (1): 112–115. doi:10.1111/j.1468-3083.2012.04663.x. ISSN 0926-9959.
- ↑ 8.0 8.1 Fukunaga M, Harada K, Mae K, Wakamatsu K, Kiriyama N, Tsuboi R; et al. (2017). "Erythema Gyratum Repens-Like Purpura in a Patient with Sjögren Syndrome". Case Rep Dermatol. 9 (2): 40–43. doi:10.1159/000477375. PMC 5498950. PMID 28690517.
- ↑ 9.0 9.1 Günther R, Nasser S, Hinrichsen H, Fölsch UR (2002). "[Erythema gyratum repens: drug reaction following azathioprine administration in a patient with type I [[autoimmune]] [[hepatitis]]". Med Klin (Munich). 97 (7): 414–7. PMID 12168480. URL–wikilink conflict (help)
- ↑ 10.0 10.1 Rongioletti, Franco; Fausti, Valentina; Parodi, Aurora (2012). "Erythema Gyratum Repens Induced by Pegylated Interferon Alfa for Chronic Hepatitis C". Archives of Dermatology. 148 (10): 1213. doi:10.1001/archdermatol.2012.1968. ISSN 0003-987X.
- ↑ Samotij D, Szczech J, Bencal-Kusinska M, Reich A (2016). "Erythema gyratum repens associated with cryptogenic organizing pneumonia". Indian J Dermatol Venereol Leprol. 82 (2): 212–3. doi:10.4103/0378-6323.173594. PMID 26765132.
- ↑ Appell ML, Ward WQ, Tyring SK (1988). "Erythema gyratum repens. A cutaneous marker of malignancy". Cancer. 62 (3): 548–50. doi:10.1002/1097-0142(19880801)62:3<548::aid-cncr2820620318>3.0.co;2-h. PMID 3390794.
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 Gore M, Winters ME (2011). "Erythema gyratum repens: a rare paraneoplastic rash". West J Emerg Med. 12 (4): 556–8. doi:10.5811/westjem.2010.11.2090. PMC 3236141. PMID 22224159.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 14.7 14.8 14.9 Tyring SK (1993). "Reactive erythemas: erythema annulare centrifugum and erythema gyratum repens". Clin Dermatol. 11 (1): 135–9. PMID 8339188.
- ↑ 15.0 15.1 Holt PJ, Davies MG (1977). "Erythema gyratum repens--an immunologically mediated dermatosis?". Br J Dermatol. 96 (4): 343–7. PMID 861171.
- ↑ Ridge A, Tummon O, Laing M (2019). "Response to "Transformation from pityriasis rubra pilaris to erythema gyratum repens-like eruption without associated malignancy: A report of 2 cases"". JAAD Case Rep. 5 (5): 461–462. doi:10.1016/j.jdcr.2019.03.012. PMC 6510971 Check
|pmc=value (help). PMID 31111084.