Cobimetinib: Difference between revisions
Martin Nino (talk | contribs) No edit summary |
Martin Nino (talk | contribs) No edit summary |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
|genericName=Cobimetinib | |genericName=Cobimetinib | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass=kinase inhibitor | |drugClass=[[kinase inhibitor]] | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in combination with vemurafenib | |indication=patients with [[unresectable]] or [[metastatic]] [[melanoma]] with a [[BRAF]] [[V600E]] or [[V600K]] [[mutation]], in combination with [[vemurafenib]] | ||
|adverseReactions=diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting (≥20%) | |adverseReactions=[[diarrhea]], [[photosensitivity reaction]], [[nausea]], [[pyrexia]], and [[vomiting]] (≥20%) | ||
|fdaLIADAdult=======Indications====== | |fdaLIADAdult=======Indications====== | ||
Cobimetinib is indicated for the treatment of patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in combination with vemurafenib | Cobimetinib is indicated for the treatment of patients with [[unresectable]] or [[metastatic]] [[melanoma]] with a [[BRAF]] [[V600E]] or [[V600K]] [[mutation]], in combination with [[vemurafenib]] | ||
======Dosage====== | ======Dosage====== | ||
:*'''Patient Selection''' | :*'''Patient Selection''' | ||
Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of treatment with Cobimetinib with vemurafenib. Information on FDA-approved tests for the detection of BRAF V600 mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics. | Confirm the presence of [[BRAF]] [[V600E]] or [[V600K]] [[mutation]] in tumor specimens prior to initiation of treatment with Cobimetinib with [[vemurafenib]]. Information on FDA-approved tests for the detection of BRAF [[V600]] mutations in [[melanoma]] is available at: http://www.fda.gov/CompanionDiagnostics. | ||
:*'''Recommended Dose''' | :*'''Recommended Dose''' | ||
The recommended dosage regimen of Cobimetinib is 60 mg (three 20 mg tablets) orally taken once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity. | The recommended dosage regimen of Cobimetinib is 60 mg (three 20 mg tablets) orally taken once daily for the first 21 days of each 28-day cycle until [[disease progression]] or unacceptable [[toxicity]]. | ||
Take Cobimetinib with or without food. | Take Cobimetinib with or without food. | ||
| Line 22: | Line 22: | ||
:*'''Dose Modifications''' | :*'''Dose Modifications''' | ||
::*Concurrent CYP3A Inhibitors | ::*Concurrent [[CYP3A]] Inhibitors | ||
Do not take strong or moderate CYP3A inhibitors while taking Cobimetinib. | Do not take strong or moderate CYP3A inhibitors while taking Cobimetinib. | ||
| Line 32: | Line 32: | ||
::*Adverse Reactions | ::*Adverse Reactions | ||
Review the Full Prescribing Information for vemurafenib for recommended dose modifications. | Review the Full Prescribing Information for [[vemurafenib]] for recommended dose modifications. | ||
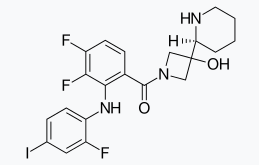
:*'''Table 1. Recommended Dose Reductions for Cobimetinib''' | |||
[[File:table1_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
COTELLIC: Cobimetinib's Brand name | |||
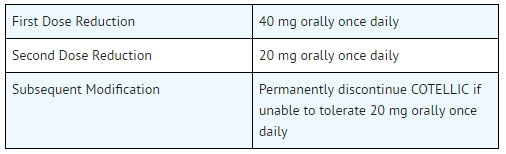
:*'''Table 2. Recommended Dose Modifications for Cobimetinib for Adverse Reactions''' | |||
[[File:table2_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
COTELLIC: Cobimetinib's Brand name | |||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Cobimetinib in adult patients. | |||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Cobimetinib in adult patients. | |||
|fdaLIADPed=The safety and effectiveness of Cobimetinib have not been established in pediatric patients | |fdaLIADPed=The safety and effectiveness of Cobimetinib have not been established in pediatric patients | ||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Cobimetinib in pediatric patients. | |||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Cobimetinib in pediatric patients. | |||
|contraindications=None | |contraindications=None | ||
|warnings=Review the Full Prescribing Information for vemurafenib for information on the serious risks of vemurafenib. | |warnings=Review the Full Prescribing Information for [[vemurafenib]] for information on the serious risks of [[vemurafenib]]. | ||
:*'''New Primary Malignancies''' | :*'''New Primary [[Malignancies]]''' | ||
New primary malignancies, cutaneous and non-cutaneous, can occur with Cobimetinib. | New primary malignancies, [[cutaneous]] and non-cutaneous, can occur with Cobimetinib. | ||
::*Cutaneous Malignancies: | ::*Cutaneous Malignancies: | ||
In Trial 1, the following cutaneous malignancies or premalignant conditions occurred in the Cobimetinib with vemurafenib arm and the vemurafenib arm, respectively: cutaneous squamous cell carcinoma (cuSCC) or keratoacanthoma (KA) (6% and 20%), basal cell carcinoma (4.5% and 2.4%), and second primary melanoma (0.8% and 2.4%). Among patients receiving Cobimetinib with vemurafenib, the median time to detection of first cuSCC/KA was 4 months (range: 2 to 11 months), and the median time to detection of basal cell carcinoma was 4 months (range: 27 days to 13 months). The time to onset in the two patients with second primary melanoma was 9 months and 12 months. | In Trial 1, the following cutaneous malignancies or [[premalignant]] conditions occurred in the Cobimetinib with [[vemurafenib]] arm and the vemurafenib arm, respectively: [[cutaneous squamous cell carcinoma]] (cuSCC) or [[keratoacanthoma]] (KA) (6% and 20%), [[basal cell carcinoma]] (4.5% and 2.4%), and second primary [[melanoma]] (0.8% and 2.4%). Among patients receiving Cobimetinib with vemurafenib, the median time to detection of first cuSCC/KA was 4 months (range: 2 to 11 months), and the median time to detection of [[basal cell carcinoma]] was 4 months (range: 27 days to 13 months). The time to onset in the two patients with second primary [[melanoma]] was 9 months and 12 months. | ||
Perform dermatologic evaluations prior to initiation of therapy and every 2 months while on therapy. Manage suspicious skin lesions with excision and dermatopathologic evaluation. No dose modifications are recommended for Cobimetinib. Conduct dermatologic monitoring for 6 months following discontinuation of Cobimetinib when administered with vemurafenib. | Perform [[dermatologic]] evaluations prior to initiation of therapy and every 2 months while on therapy. Manage suspicious [[skin lesions]] with [[excision]] and [[dermatopathologic]] evaluation. No dose modifications are recommended for Cobimetinib. Conduct dermatologic monitoring for 6 months following discontinuation of Cobimetinib when administered with [[vemurafenib]]. | ||
::*Non-Cutaneous Malignancies: | ::*Non-Cutaneous Malignancies: | ||
Based on its mechanism of action, vemurafenib may promote growth and development of malignancies [refer to the Full Prescribing Information for vemurafenib]. In Trial 1, 0.8% of patients in the Cobimetinib with vemurafenib arm and 1.2% of patients in the vemurafenib arm developed non-cutaneous malignancies. | Based on its [[mechanism of action]], [[vemurafenib]] may promote growth and development of malignancies [refer to the Full Prescribing Information for vemurafenib]. In Trial 1, 0.8% of patients in the Cobimetinib with vemurafenib arm and 1.2% of patients in the vemurafenib arm developed non-cutaneous malignancies. | ||
Monitor patients receiving Cobimetinib, when administered with vemurafenib, for signs or symptoms of non-cutaneous malignancies. | Monitor patients receiving Cobimetinib, when administered with [[vemurafenib]], for signs or symptoms of non-cutaneous malignancies. | ||
:*'''Hemorrhage''' | :*'''[[Hemorrhage]]''' | ||
Hemorrhage, including major hemorrhages defined as symptomatic bleeding in a critical area or organ, can occur with Cobimetinib. | Hemorrhage, including major hemorrhages defined as symptomatic [[bleeding]] in a critical area or organ, can occur with Cobimetinib. | ||
In Trial 1, the incidence of Grade 3–4 hemorrhages was 1.2% in patients receiving Cobimetinib with vemurafenib and 0.8% in patients receiving vemurafenib. Hemorrhage (all grades) was 13% in patients receiving Cobimetinib with vemurafenib and 7% in patients receiving vemurafenib. Cerebral hemorrhage occurred in 0.8% of patients receiving Cobimetinib with vemurafenib and in none of the patients receiving vemurafenib. Gastrointestinal tract hemorrhage (3.6% vs 1.2%), reproductive system hemorrhage (2.0% vs 0.4%), and hematuria (2.4% vs 0.8%) also occurred at a higher incidence in patients receiving Cobimetinib with vemurafenib compared with patients receiving vemurafenib. | In Trial 1, the incidence of Grade 3–4 [[hemorrhages]] was 1.2% in patients receiving Cobimetinib with [[vemurafenib]] and 0.8% in patients receiving vemurafenib. Hemorrhage (all grades) was 13% in patients receiving Cobimetinib with vemurafenib and 7% in patients receiving vemurafenib. Cerebral hemorrhage occurred in 0.8% of patients receiving Cobimetinib with vemurafenib and in none of the patients receiving vemurafenib. [[Gastrointestinal tract hemorrhage]] (3.6% vs 1.2%), [[reproductive system hemorrhage]] (2.0% vs 0.4%), and [[hematuria]] (2.4% vs 0.8%) also occurred at a higher incidence in patients receiving Cobimetinib with vemurafenib compared with patients receiving vemurafenib. | ||
Withhold Cobimetinib for Grade 3 hemorrhagic events. If improved to Grade 0 or 1 within 4 weeks, resume Cobimetinib at a lower dose level. Discontinue Cobimetinib for Grade 4 hemorrhagic events and any Grade 3 hemorrhagic events that do not improve. | Withhold Cobimetinib for Grade 3 hemorrhagic events. If improved to Grade 0 or 1 within 4 weeks, resume Cobimetinib at a lower dose level. Discontinue Cobimetinib for Grade 4 hemorrhagic events and any Grade 3 hemorrhagic events that do not improve. | ||
:*'''Cardiomyopathy''' | :*'''[[Cardiomyopathy]]''' | ||
Cardiomyopathy, defined as symptomatic and asymptomatic decline in | Cardiomyopathy, defined as symptomatic and asymptomatic decline in l[[eft ventricular ejection fraction]] (LVEF), can occur with Cobimetinib . The safety of Cobimetinib has not been established in patients with a baseline LVEF that is either below institutional lower limit of normal (LLN) or below 50%. | ||
In Trial 1, patients were assessed for decreases in LVEF by echocardiograms or MUGA at baseline, Week 5, Week 17, Week 29, Week 43, and then every 4 to 6 months thereafter while receiving treatment. Grade 2 or 3 decrease in LVEF occurred in 26% of patients receiving Cobimetinib with vemurafenib and 19% of patients receiving vemurafenib. The median time to first onset of LVEF decrease was 4 months (range 23 days to 13 months). Of the patients with decreased LVEF, 22% had dose interruption and/or reduction and 14% required permanent discontinuation. Decreased LVEF resolved to above the LLN or within 10% of baseline in 62% of patients receiving Cobimetinib with a median time to resolution of 3 months (range: 4 days to 12 months). | In Trial 1, patients were assessed for decreases in [[LVEF]] by [[echocardiograms]] or [[MUGA]] at baseline, Week 5, Week 17, Week 29, Week 43, and then every 4 to 6 months thereafter while receiving treatment. Grade 2 or 3 decrease in LVEF occurred in 26% of patients receiving Cobimetinib with vemurafenib and 19% of patients receiving vemurafenib. The median time to first onset of LVEF decrease was 4 months (range 23 days to 13 months). Of the patients with decreased LVEF, 22% had dose interruption and/or reduction and 14% required permanent discontinuation. Decreased LVEF resolved to above the LLN or within 10% of baseline in 62% of patients receiving Cobimetinib with a median time to resolution of 3 months (range: 4 days to 12 months). | ||
Evaluate LVEF prior to initiation, 1 month after initiation, and every 3 months thereafter until discontinuation of Cobimetinib. Manage events of left ventricular dysfunction through treatment interruption, reduction, or discontinuation | Evaluate LVEF prior to initiation, 1 month after initiation, and every 3 months thereafter until discontinuation of Cobimetinib. Manage events of [[left ventricular dysfunction]] through treatment interruption, reduction, or discontinuation. In patients restarting Cobimetinib after a dose reduction or interruption, evaluate [[LVEF]] at approximately 2 weeks, 4 weeks, 10 weeks, and 16 weeks, and then as clinically indicated. | ||
:*'''Severe Dermatologic Reactions''' | :*'''Severe [[Dermatologic Reactions]]''' | ||
Severe rash and other skin reactions can occur with Cobimetinib. | Severe [[rash]] and other [[skin reactions]] can occur with Cobimetinib. | ||
In Trial 1, Grade 3 to 4 rash, occurred in 16% of patients receiving Cobimetinib with vemurafenib and in 17% of patients receiving vemurafenib, including Grade 4 rash in 1.6% of patients receiving Cobimetinib with vemurafenib and 0.8% of the patients receiving vemurafenib. The incidence of rash resulting in hospitalization was 3.2% in patients receiving Cobimetinib with vemurafenib and 2.0% in patients receiving vemurafenib. In patients receiving Cobimetinib, the median time to onset of Grade 3 or 4 rash events was 11 days (range: 3 days to 2.8 months). Among patients with Grade 3 or 4 rash events, 95% experienced complete resolution with the median time to resolution of 21 days (range 4 days to 17 months). | In Trial 1, Grade 3 to 4 [[rash]], occurred in 16% of patients receiving Cobimetinib with [[vemurafenib]] and in 17% of patients receiving vemurafenib, including Grade 4 rash in 1.6% of patients receiving Cobimetinib with vemurafenib and 0.8% of the patients receiving vemurafenib. The incidence of rash resulting in hospitalization was 3.2% in patients receiving Cobimetinib with vemurafenib and 2.0% in patients receiving vemurafenib. In patients receiving Cobimetinib, the median time to onset of Grade 3 or 4 rash events was 11 days (range: 3 days to 2.8 months). Among patients with Grade 3 or 4 rash events, 95% experienced complete resolution with the median time to resolution of 21 days (range 4 days to 17 months). | ||
Interrupt, reduce the dose, or discontinue Cobimetinib. | Interrupt, reduce the dose, or discontinue Cobimetinib. | ||
:*'''Serous Retinopathy and Retinal Vein Occlusion''' | :*'''Serous [[Retinopathy]] and [[Retinal Vein Occlusion]]''' | ||
Ocular toxicities can occur with Cobimetinib, including serous retinopathy (fluid accumulation under layers of the retina). | Ocular toxicities can occur with Cobimetinib, including serous [[retinopathy]] (fluid accumulation under layers of the [[retina]]). | ||
In Trial 1, ophthalmologic examinations including retinal evaluation were performed pretreatment and at regular intervals during treatment. Symptomatic and asymptomatic serous retinopathy was identified in 26% of patients receiving Cobimetinib with vemurafenib. The majority of these events were reported as chorioretinopathy (13%) or retinal detachment (12%). The time to first onset of serous retinopathy events ranged between 2 days to 9 months. The reported duration of serous retinopathy ranged between 1 day to 15 months. One patient in each arm developed retinal vein occlusion. | In Trial 1, ophthalmologic examinations including retinal evaluation were performed pretreatment and at regular intervals during treatment. Symptomatic and asymptomatic serous [[retinopathy]] was identified in 26% of patients receiving Cobimetinib with [[vemurafenib]]. The majority of these events were reported as [[chorioretinopathy]] (13%) or [[retinal detachment]] (12%). The time to first onset of serous retinopathy events ranged between 2 days to 9 months. The reported duration of serous retinopathy ranged between 1 day to 15 months. One patient in each arm developed [[retinal vein occlusion]]. | ||
Perform an ophthalmological evaluation at regular intervals and any time a patient reports new or worsening visual disturbances. If serous retinopathy is diagnosed, interrupt Cobimetinib until visual symptoms improve. Manage serous retinopathy with treatment interruption, dose reduction, or with treatment discontinuation. | Perform an ophthalmological evaluation at regular intervals and any time a patient reports new or worsening [[visual disturbances]]. If serous [[retinopathy]] is diagnosed, interrupt Cobimetinib until visual symptoms improve. Manage serous retinopathy with treatment interruption, dose reduction, or with treatment discontinuation. | ||
:*'''Hepatotoxicity''' | :*'''[[Hepatotoxicity]]''' | ||
Hepatotoxicity can occur with Cobimetinib. | Hepatotoxicity can occur with Cobimetinib. | ||
The incidences of Grade 3 or 4 liver laboratory abnormalities in Trial 1 among patients receiving Cobimetinib with vemurafenib compared to patients receiving vemurafenib were: 11% vs. 5% for alanine aminotransferase, 8% vs. 2.1% for aspartate aminotransferase, 1.6% vs. 1.2% for total bilirubin, and 7% vs. 3.3% for alkaline phosphatase. Concurrent elevation in ALT >3 times the upper limit of normal (ULN) and bilirubin >2 × ULN in the absence of significant alkaline phosphatase >2 × ULN occurred in one patient (0.4%) receiving Cobimetinib with vemurafenib and no patients receiving single-agent vemurafenib. | The incidences of Grade 3 or 4 liver laboratory abnormalities in Trial 1 among patients receiving Cobimetinib with [[vemurafenib]] compared to patients receiving vemurafenib were: 11% vs. 5% for [[alanine aminotransferase]], 8% vs. 2.1% for [[aspartate aminotransferase]], 1.6% vs. 1.2% for total [[bilirubin]], and 7% vs. 3.3% for [[alkaline phosphatase]]. Concurrent elevation in [[ALT]] >3 times the upper limit of normal (ULN) and bilirubin >2 × ULN in the absence of significant [[alkaline phosphatase]] >2 × ULN occurred in one patient (0.4%) receiving Cobimetinib with vemurafenib and no patients receiving single-agent vemurafenib. | ||
Monitor liver laboratory tests before initiation of Cobimetinib and monthly during treatment, or more frequently as clinically indicated. Manage Grade 3 and 4 liver laboratory abnormalities with dose interruption, reduction, or discontinuation of Cobimetinib. | Monitor liver laboratory tests before initiation of Cobimetinib and monthly during treatment, or more frequently as clinically indicated. Manage Grade 3 and 4 liver laboratory abnormalities with dose interruption, reduction, or discontinuation of Cobimetinib. | ||
:*'''Rhabdomyolysis''' | :*'''[[Rhabdomyolysis]]''' | ||
Rhabdomyolysis can occur with Cobimetinib. | Rhabdomyolysis can occur with Cobimetinib. | ||
In Trial 1, Grade 3 or 4 CPK elevations, including asymptomatic elevations over baseline, occurred in 14% of patients receiving Cobimetinib with vemurafenib and 0.5% of patients receiving vemurafenib. The median time to first occurrence of Grade 3 or 4 CPK elevations was 16 days (range: 12 days to 11 months) in patients receiving Cobimetinib with vemurafenib; the median time to complete resolution was 15 days (range: 9 days to 11 months). Elevation of serum CPK increase of more than 10 times the baseline value with a concurrent increase in serum creatinine of 1.5 times or greater compared to baseline occurred in 3.6% of patients receiving Cobimetinib with vemurafenib and in 0.4% of patients receiving vemurafenib. | In Trial 1, Grade 3 or 4 [[CPK]] elevations, including asymptomatic elevations over baseline, occurred in 14% of patients receiving Cobimetinib with [[vemurafenib]] and 0.5% of patients receiving vemurafenib. The median time to first occurrence of Grade 3 or 4 CPK elevations was 16 days (range: 12 days to 11 months) in patients receiving Cobimetinib with vemurafenib; the median time to complete resolution was 15 days (range: 9 days to 11 months). Elevation of serum [[CPK]] increase of more than 10 times the baseline value with a concurrent increase in serum [[creatinine]] of 1.5 times or greater compared to baseline occurred in 3.6% of patients receiving Cobimetinib with vemurafenib and in 0.4% of patients receiving vemurafenib. | ||
Obtain baseline serum CPK and creatinine levels prior to initiating Cobimetinib, periodically during treatment, and as clinically indicated. If CPK is elevated, evaluate for signs and symptoms of rhabdomyolysis or other causes. Depending on the severity of symptoms or CPK elevation, dose interruption or discontinuation of Cobimetinib may be required. | Obtain baseline serum [[CPK]] and [[creatinine]] levels prior to initiating Cobimetinib, periodically during treatment, and as clinically indicated. If CPK is elevated, evaluate for signs and symptoms of [[rhabdomyolysis]] or other causes. Depending on the severity of symptoms or CPK elevation, dose interruption or discontinuation of Cobimetinib may be required. | ||
:*'''Severe Photosensitivity''' | :*'''Severe [[Photosensitivity]]''' | ||
Photosensitivity, including severe cases, can occur with Cobimetinib. | Photosensitivity, including severe cases, can occur with Cobimetinib. | ||
In Trial 1, photosensitivity was reported in 47% of patients receiving Cobimetinib with vemurafenib: 43% of patients with Grades 1 or 2 photosensitivity and the remaining 4% with Grade 3 photosensitivity. Median time to first onset of photosensitivity of any grade was 2 months (range: 1 day to 14 months) in patients receiving Cobimetinib with vemurafenib, and the median duration of photosensitivity was 3 months (range: 2 days to 14 months). Among the 47% of patients with photosensitivity reactions on Cobimetinib with vemurafenib, 63% experienced resolution of photosensitivity reactions. | In Trial 1, photosensitivity was reported in 47% of patients receiving Cobimetinib with [[vemurafenib]]: 43% of patients with Grades 1 or 2 photosensitivity and the remaining 4% with Grade 3 photosensitivity. Median time to first onset of photosensitivity of any grade was 2 months (range: 1 day to 14 months) in patients receiving Cobimetinib with [[vemurafenib]], and the median duration of photosensitivity was 3 months (range: 2 days to 14 months). Among the 47% of patients with photosensitivity reactions on Cobimetinib with vemurafenib, 63% experienced resolution of photosensitivity reactions. | ||
Advise patients to avoid sun exposure, wear protective clothing and use a broad-spectrum UVA/UVB sunscreen and lip balm (SPF ≥30) when outdoors. Manage intolerable Grade 2 or greater photosensitivity with dose modifications. | Advise patients to avoid sun exposure, wear protective clothing and use a broad-spectrum [[UVA]]/[[UVB]] sunscreen and lip balm (SPF ≥30) when outdoors. Manage intolerable Grade 2 or greater photosensitivity with dose modifications. | ||
:*'''Embryo-Fetal Toxicity''' | :*'''Embryo-Fetal Toxicity''' | ||
Based on its mechanism of action and findings from animal reproduction studies, Cobimetinib can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during the period of organogenesis was teratogenic and embryotoxic at doses resulting in exposures [area under the curves ( | Based on its [[mechanism of action]] and findings from animal reproduction studies, Cobimetinib can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during the period of [[organogenesis]] was [[teratogenic]] and [[embryotoxic]] at doses resulting in exposures [area under the curves ([[AUC]]s)] that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective [[contraception]] during treatment with Cobimetinib, and for 2 weeks following the final dose of Cobimetinib. | ||
|clinicalTrials=Because clinical | |clinicalTrials=Because [[clinical trial]]s are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | ||
The safety of Cobimetinib was evaluated in Trial 1, a randomized (1:1), double-blind, active-controlled trial in previously untreated patients with BRAF V600 mutation-positive, unresectable or metastatic melanoma. All patients received vemurafenib 960 mg twice daily on Days 1–28 and received either Cobimetinib 60 mg once daily (n=247) or placebo (n=246) on Days 1–21 of each 28-day treatment cycle until disease progression or unacceptable toxicity. In the Cobimetinib plus vemurafenib arm, 66% percent of patients were exposed for greater than 6 months and 24% of patients were exposed for greater than 1 year. Patients with abnormal liver function tests, history of acute coronary syndrome within 6 months, evidence of Class II or greater congestive heart failure (New York Heart Association), active central nervous system lesions, or evidence of retinal pathology were excluded from Trial 1. The demographics and baseline tumor characteristics of patients enrolled in Trial 1 are summarized in Clinical Studies. | The safety of Cobimetinib was evaluated in Trial 1, a [[randomized]] (1:1), [[double-blind]], active-controlled trial in previously untreated patients with [[BRAF]] [[V600]] mutation-positive, [[unresectable]] or [[metastatic]] [[melanoma]]. All patients received [[vemurafenib]] 960 mg twice daily on Days 1–28 and received either Cobimetinib 60 mg once daily (n=247) or [[placebo]] (n=246) on Days 1–21 of each 28-day treatment cycle until [[disease progression]] or unacceptable [[toxicity]]. In the Cobimetinib plus vemurafenib arm, 66% percent of patients were exposed for greater than 6 months and 24% of patients were exposed for greater than 1 year. Patients with abnormal liver function tests, history of [[acute coronary syndrome]] within 6 months, evidence of Class II or greater [[congestive heart failure]] (New York Heart Association), active [[central nervous system]] lesions, or evidence of [[retinal pathology]] were excluded from Trial 1. The demographics and baseline [[tumor]] characteristics of patients enrolled in Trial 1 are summarized in Clinical Studies. | ||
In Trial 1, 15% of patients receiving Cobimetinib experienced an adverse reaction that resulted in permanent discontinuation of Cobimetinib. The most common adverse reactions resulting in permanent discontinuation were liver laboratory abnormalities defined as increased aspartate aminotransferase (AST) (2.4%), increased gamma glutamyltransferase (GGT) (1.6%) and increased alanine aminotransferase (ALT) (1.6%); rash (1.6%); pyrexia (1.2%); and retinal detachment (2%). Among the 247 patients receiving Cobimetinib, adverse reactions led to dose interruption or reductions in 55%. The most common reasons for dose interruptions or reductions of Cobimetinib were rash (11%), diarrhea (9%), chorioretinopathy (7%), pyrexia (6%), vomiting (6%), nausea (5%), and increased creatine phosphokinase (CPK) (4.9%). The most common (≥20%) adverse reactions with Cobimetinib were diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting. | In Trial 1, 15% of patients receiving Cobimetinib experienced an adverse reaction that resulted in permanent discontinuation of Cobimetinib. The most common adverse reactions resulting in permanent discontinuation were liver laboratory abnormalities defined as increased [[aspartate aminotransferase]] (AST) (2.4%), increased [[gamma glutamyltransferase]] (GGT) (1.6%) and increased [[alanine aminotransferase]] (ALT) (1.6%); [[rash]] (1.6%); [[pyrexia]] (1.2%); and [[retinal detachment]] (2%). Among the 247 patients receiving Cobimetinib, adverse reactions led to dose interruption or reductions in 55%. The most common reasons for dose interruptions or reductions of Cobimetinib were [[rash]] (11%), [[diarrhea]] (9%), [[chorioretinopathy]] (7%), [[pyrexia]] (6%), [[vomiting]] (6%), [[nausea]] (5%), and increased [[creatine phosphokinase]] (CPK) (4.9%). The most common (≥20%) adverse reactions with Cobimetinib were diarrhea, [[photosensitivity reaction]], nausea, pyrexia, and vomiting. | ||
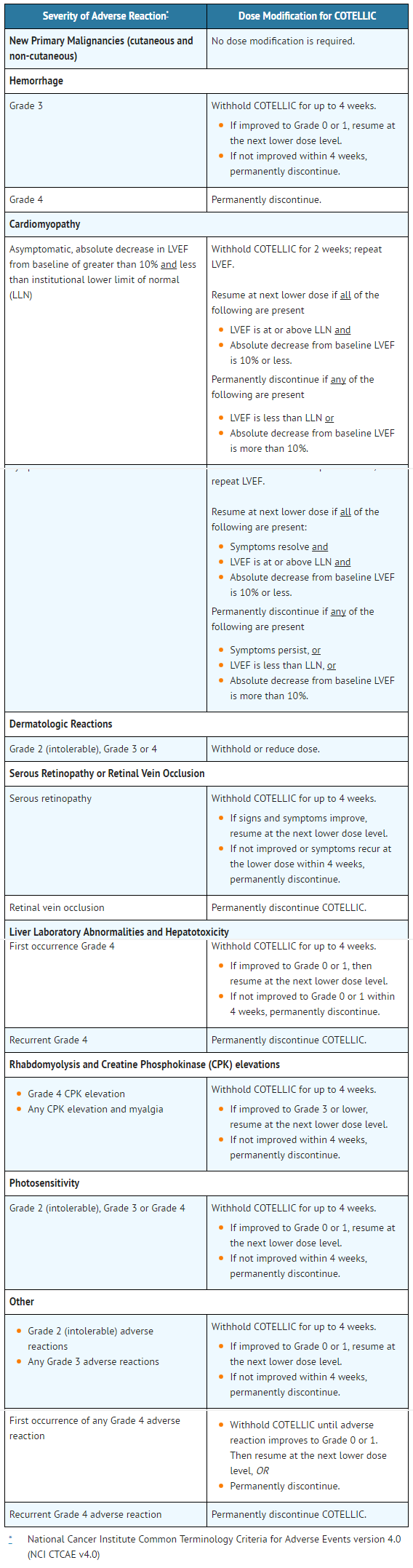
:*'''Table 3. Incidence of Adverse Drug Reactions Occurring in ≥10% (All Grades) of Patients Receiving Cobimetinib with Vemurafenib and at a Higher Incidence* than Patients Receiving Vemurafenib in Trial 1''' | |||
[[File:table3_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
COTELLIC: Cobimetinib's Brand name | |||
Adverse reactions of vemurafenib which occurred at a lower rate in patients receiving Cobimetinib plus vemurafenib were alopecia (15%), hyperkeratosis (11%), and erythema (10%). | Adverse reactions of vemurafenib which occurred at a lower rate in patients receiving Cobimetinib plus [[vemurafenib]] were [[alopecia]] (15%), [[hyperkeratosis]] (11%), and [[erythema]] (10%). | ||
The following adverse reactions (all grades) of Cobimetinib were reported with <10% incidence in Trial 1: | The following adverse reactions (all grades) of Cobimetinib were reported with <10% incidence in Trial 1: | ||
Respiratory, thoracic and mediastinal disorders: Pneumonitis | [[Respiratory]], [[thoracic]] and [[mediastinal]] disorders: [[Pneumonitis]] | ||
:*'''Table 4. Incidence of Laboratory Abnormalities Occurring in ≥10% (All Grades) or ≥2% (Grades 3–4) of Patients in Trial 1*''' | |||
|drugInteractions=:*'''Effect of Strong or Moderate CYP3A Inhibitors on Cobimetinib''' | [[File:table4_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Coadministration of Cobimetinib with itraconazole (a strong CYP3A4 inhibitor) increased Cobimetinib systemic exposure by 6.7-fold. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inhibitors. If concurrent short term (14 days or less) use of moderate CYP3A inhibitors including certain antibiotics (e.g., erythromycin, ciprofloxacin) is unavoidable for patients who are taking Cobimetinib 60 mg, reduce Cobimetinib dose to 20 mg. After discontinuation of a moderate CYP3A inhibitor, resume Cobimetinib at the previous dose. Use an alternative to a strong or moderate CYP3A inhibitor in patients who are taking a reduced dose of Cobimetinib (40 or 20 mg daily). | COTELLIC: Cobimetinib's Brand name | ||
|drugInteractions=:*'''Effect of Strong or Moderate [[CYP3A]] Inhibitors on Cobimetinib''' | |||
Coadministration of Cobimetinib with [[itraconazole]] (a strong CYP3A4 inhibitor) increased Cobimetinib systemic exposure by 6.7-fold. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inhibitors. If concurrent short term (14 days or less) use of moderate CYP3A inhibitors including certain [[antibiotics]] (e.g., [[erythromycin]], [[ciprofloxacin]]) is unavoidable for patients who are taking Cobimetinib 60 mg, reduce Cobimetinib dose to 20 mg. After discontinuation of a moderate CYP3A inhibitor, resume Cobimetinib at the previous dose. Use an alternative to a strong or moderate CYP3A inhibitor in patients who are taking a reduced dose of Cobimetinib (40 or 20 mg daily). | |||
:*'''Effect of Strong or Moderate CYP3A Inducers on Cobimetinib''' | :*'''Effect of Strong or Moderate [[CYP3A]] Inducers on Cobimetinib''' | ||
Coadministration of Cobimetinib with a strong CYP3A inducer may decrease Cobimetinib systemic exposure by more than 80% and reduce its efficacy. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inducers including but not limited to carbamazepine, efavirenz, phenytoin, rifampin, and St. John's Wort. | Coadministration of Cobimetinib with a strong CYP3A inducer may decrease Cobimetinib systemic exposure by more than 80% and reduce its efficacy. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inducers including but not limited to [[carbamazepine]], [[efavirenz]], [[phenytoin]], [[rifampin]], and [[St. John's Wort]]. | ||
|FDAPregCat=N | |FDAPregCat=N | ||
|useInPregnancyFDA=:*Risk Summary | |useInPregnancyFDA=:*Risk Summary | ||
Based on findings from animal reproduction studies and its mechanism of action, Cobimetinib can cause fetal harm when administered to a pregnant woman. There are no available data on the use of Cobimetinib during pregnancy. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during organogenesis was teratogenic and embryotoxic at exposures (AUC) that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus. | Based on findings from animal reproduction studies and its [[mechanism of action]], Cobimetinib can cause fetal harm when administered to a pregnant woman. There are no available data on the use of Cobimetinib during pregnancy. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during [[organogenesis]] was [[teratogenic]] and [[embryotoxic]] at exposures ([[AUC]]) that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus. | ||
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively. | In the U.S. general population, the estimated background risk of major birth defects and [[miscarriage]] in clinically recognized pregnancies is 2–4% and 15–20%, respectively. | ||
:*Data | :*Data | ||
| Line 137: | Line 150: | ||
::*Animal Data | ::*Animal Data | ||
Administration of Cobimetinib to pregnant rats during the period of organogenesis resulted in increased post-implantation loss, including total litter loss, at exposures (AUC) of 0.9–1.4 times those in humans at the recommended dose of 60 mg. Post-implantation loss was primarily due to early resorptions. Fetal malformations of the great vessels and skull (eye sockets) occurred at the same exposures. | Administration of Cobimetinib to pregnant rats during the period of [[organogenesis]] resulted in increased [[post-implantation loss]], including total [[litter loss]], at exposures ([[AUC]]) of 0.9–1.4 times those in humans at the recommended dose of 60 mg. Post-implantation loss was primarily due to early resorptions. [[Fetal malformations]] of the [[great vessels]] and [[skull]] (eye sockets) occurred at the same exposures. | ||
|useInNursing=There is no information regarding the presence of Cobimetinib in human milk, effects on the breastfed infant, or effects on milk production. Because of the potential for serious adverse reactions in a breastfed infant, advise a nursing woman not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose. | |useInNursing=There is no information regarding the presence of Cobimetinib in human milk, effects on the breastfed infant, or effects on milk production. Because of the potential for serious adverse reactions in a breastfed infant, advise a nursing woman not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose. | ||
|useInPed=The safety and effectiveness of Cobimetinib have not been established in pediatric patients. | |useInPed=The safety and effectiveness of Cobimetinib have not been established in pediatric patients. | ||
| Line 143: | Line 156: | ||
:*Juvenile Animal Data | :*Juvenile Animal Data | ||
In a 4-week juvenile rat toxicology study, daily oral doses of 3 mg/kg (approximately 0.13–0.5 times the adult human AUC at the recommended dose of 60 mg) between postnatal Days 10–17 (approximately equivalent to ages 1–2 years in humans) were associated with mortality, the cause of which was not defined. | In a 4-week juvenile rat [[toxicology]] study, daily oral doses of 3 mg/kg (approximately 0.13–0.5 times the adult human [[AUC]] at the recommended dose of 60 mg) between postnatal Days 10–17 (approximately equivalent to ages 1–2 years in humans) were associated with [[mortality]], the cause of which was not defined. | ||
|useInGeri=Clinical studies of Cobimetinib did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. | |useInGeri=Clinical studies of Cobimetinib did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. | ||
|useInRenalImpair=No dedicated pharmacokinetic trial in patients with renal impairment has been conducted. Dose adjustment is not recommended for mild to moderate renal impairment (CLcr 30 to 89 mL/min) based on the results of the population pharmacokinetic analysis. A recommended dose has not been established for patients with severe renal impairment. | |useInRenalImpair=No dedicated [[pharmacokinetic]] trial in patients with [[renal impairment]] has been conducted. Dose adjustment is not recommended for mild to moderate renal impairment ([[CLcr]] 30 to 89 mL/min) based on the results of the population [[pharmacokinetic]] analysis. A recommended dose has not been established for patients with severe renal impairment. | ||
|useInHepaticImpair=Adjustment in the starting dose of Cobimetinib is not required in patients with mild (Child-Pugh score A), moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment. | |useInHepaticImpair=Adjustment in the starting dose of Cobimetinib is not required in patients with mild ([[Child-Pugh]] score A), moderate ([[Child-Pugh]] B) or severe ([[Child-Pugh]] C) [[hepatic impairment]]. | ||
|useInReproPotential=:*'''Contraception''' | |useInReproPotential=:*'''[[Contraception]]''' | ||
::*Females | ::*Females | ||
| Line 153: | Line 166: | ||
Cobimetinib can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib and for 2 weeks after the final dose of Cobimetinib. | Cobimetinib can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib and for 2 weeks after the final dose of Cobimetinib. | ||
:*'''Infertility''' | :*'''[[Infertility]]''' | ||
::*Females and Males | ::*Females and Males | ||
| Line 164: | Line 177: | ||
:*If a dose of Cobimetinib is missed or if vomiting occurs when the dose is taken, resume dosing with the next scheduled dose. | :*If a dose of Cobimetinib is missed or if vomiting occurs when the dose is taken, resume dosing with the next scheduled dose. | ||
|overdose=There is no information on overdosage of Cobimetinib. | |overdose=There is no information on overdosage of Cobimetinib. | ||
|drugBox={{Drugbox2 | |drugBox={{Drugbox2 | ||
| drug_name = | | drug_name = | ||
| Line 216: | Line 228: | ||
| StdInChIKey = BSMCAPRUBJMWDF-KRWDZBQOSA-N | | StdInChIKey = BSMCAPRUBJMWDF-KRWDZBQOSA-N | ||
}} | }} | ||
|mechAction=Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1 (MEK1) and MEK2. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway, which promotes cellular proliferation. BRAF V600E and K mutations result in constitutive activation of the BRAF pathway which includes MEK1 and MEK2. In mice implanted with tumor cell lines expressing BRAF V600E, Cobimetinib inhibited tumor cell growth. | |mechAction=Cobimetinib is a reversible inhibitor of [[mitogen-activated protein kinase]] (MAPK)/extracellular signal regulated kinase 1 ([[MEK1]]) and [[MEK2]]. MEK proteins are upstream regulators of the [[extracellular signal-related kinase]] (ERK) pathway, which promotes [[cellular proliferation]]. [[BRAF]] [[V600E]] and K mutations result in constitutive activation of the BRAF pathway which includes MEK1 and MEK2. In mice implanted with [[tumor]] cell lines expressing BRAF V600E, Cobimetinib inhibited tumor cell growth. | ||
Cobimetinib and vemurafenib target two different kinases in the RAS/RAF/MEK/ERK pathway. Compared to either drug alone, coadministration of Cobimetinib and vemurafenib resulted in increased apoptosis in vitro and reduced tumor growth in mouse implantation models of tumor cell lines harboring BRAF V600E mutations. Cobimetinib also prevented vemurafenib-mediated growth enhancement of a wild-type BRAF tumor cell line in an in vivo mouse implantation model. | Cobimetinib and vemurafenib target two different [[kinases]] in the [[RAS]]/[[RAF]]/[[MEK]]/[[ERK]] pathway. Compared to either drug alone, coadministration of Cobimetinib and [[vemurafenib]] resulted in increased [[apoptosis]] [[in vitro]] and reduced tumor growth in mouse implantation models of tumor cell lines harboring [[BRAF]] [[V600E]] mutations. Cobimetinib also prevented vemurafenib-mediated growth enhancement of a wild-type BRAF tumor cell line in an in vivo mouse implantation model. | ||
|structure=Cobimetinib is a fumarate salt appearing as white to off-white solid and exhibits a pH dependent solubility. | |structure=Cobimetinib is a fumarate salt appearing as white to off-white solid and exhibits a [[pH]] dependent solubility. | ||
Cobimetinib tablets are supplied as white, round, film-coated 20 mg tablets for oral administration, debossed on one side with "COB". Each 20 mg tablet contains 22 mg of cobimetinib fumarate, which corresponds to 20 mg of the cobimetinib free base. | Cobimetinib tablets are supplied as white, round, film-coated 20 mg tablets for oral administration, debossed on one side with "COB". Each 20 mg tablet contains 22 mg of cobimetinib fumarate, which corresponds to 20 mg of the cobimetinib free base. | ||
The inactive ingredients of Cobimetinib are: Tablet Core: microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate. Coating: polyvinyl alcohol, titanium dioxide, polyethylene glycol 3350, talc. | The inactive ingredients of Cobimetinib are: Tablet Core: [[microcrystalline cellulose]], [[lactose monohydrate]], [[croscarmellose sodium]], [[magnesium stearate]]. Coating: [[polyvinyl alcohol]], [[titanium dioxide]], [[polyethylene glycol 3350]], [[talc]]. | ||
|PD=:*Cardiac Electrophysiology | |PD=:*Cardiac [[Electrophysiology]] | ||
Clinically relevant QT prolongation has been reported with vemurafenib, further QTc prolongation was not observed when Cobimetinib 60 mg daily was co-administered with vemurafenib. Monitor ECG and electrolytes before initiating treatment and routinely during treatment with Cobimetinib, when administered with vemurafenib. Review the Full Prescribing Information for vemurafenib for details. | Clinically relevant [[QT]] prolongation has been reported with [[vemurafenib]], further [[QTc]] prolongation was not observed when Cobimetinib 60 mg daily was co-administered with vemurafenib. Monitor [[ECG]] and [[electrolytes]] before initiating treatment and routinely during treatment with Cobimetinib, when administered with vemurafenib. Review the Full Prescribing Information for vemurafenib for details. | ||
|PK=The pharmacokinetics of Cobimetinib was studied in healthy subjects and cancer patients. Cobimetinib exhibits linear pharmacokinetics in the dose range of 3.5 to 100 mg (i.e., 0.06 to 1.7 times the recommended dosage). Following oral administration of Cobimetinib 60 mg once daily, steady-state was reached by 9 days with a mean accumulation ratio of 2.4-fold (44% CV). | |PK=The [[pharmacokinetics]] of Cobimetinib was studied in healthy subjects and [[cancer]] patients. Cobimetinib exhibits linear pharmacokinetics in the dose range of 3.5 to 100 mg (i.e., 0.06 to 1.7 times the recommended dosage). Following oral administration of Cobimetinib 60 mg once daily, steady-state was reached by 9 days with a mean accumulation ratio of 2.4-fold (44% CV). | ||
:*'''Absorption''' | :*'''[[Absorption]]''' | ||
Following oral dosing of 60 mg once daily in cancer patients, the median time to achieve peak plasma levels (Tmax) was 2.4 (range:1–24) hours, geometric mean steady-state AUC(0-24h) was 4340 ng∙h/mL (61% CV) and Cmax was 273 ng/mL (60% CV). The absolute bioavailability of Cobimetinib was 46% (90% CI: 40%, 53%) in healthy subjects. A high-fat meal (comprised of approximately 150 calories from protein, 250 calories from carbohydrate, and 500–600 calories from fat) had no effect on Cobimetinib AUC and Cmax after a single 20 mg Cobimetinib was administered to healthy subjects. | Following oral dosing of 60 mg once daily in [[cancer]] patients, the median time to achieve [[peak plasma levels]] ([[Tmax]]) was 2.4 (range:1–24) hours, geometric mean steady-state [[AUC]](0-24h) was 4340 ng∙h/mL (61% CV) and [[Cmax]] was 273 ng/mL (60% CV). The absolute [[bioavailability]] of Cobimetinib was 46% (90% CI: 40%, 53%) in healthy subjects. A high-fat meal (comprised of approximately 150 calories from protein, 250 calories from carbohydrate, and 500–600 calories from fat) had no effect on Cobimetinib AUC and Cmax after a single 20 mg Cobimetinib was administered to healthy subjects. | ||
:*'''Distribution''' | :*'''[[Distribution]]''' | ||
Cobimetinib is 95% bound to human plasma proteins in vitro, independent of drug concentration. No preferential binding to human red blood cells was observed (blood to plasma ratio of 0.93). The estimated apparent volume of distribution was 806 L in cancer patients based on a population PK analysis. | Cobimetinib is 95% bound to [[human plasma proteins]] [[in vitro]], independent of drug concentration. No preferential binding to human [[red blood cells]] was observed (blood to plasma ratio of 0.93). The estimated apparent [[volume of distribution]] was 806 L in cancer patients based on a population [[PK]] analysis. | ||
:*'''Elimination''' | :*'''[[Elimination]]''' | ||
Following oral administration of Cobimetinib 60 mg once daily in cancer patients, the mean elimination half-life (t1/2) was 44 (range: 23–70) hours and the mean apparent clearance (CL/F) was 13.8 L/h (61% CV). | Following oral administration of Cobimetinib 60 mg once daily in cancer patients, the mean elimination [[half-life]] (t1/2) was 44 (range: 23–70) hours and the mean apparent [[clearance]] (CL/F) was 13.8 L/h (61% CV). | ||
::*Metabolism | ::*[[Metabolism]] | ||
CYP3A oxidation and UGT2B7 glucuronidation were the major pathways of Cobimetinib metabolism in vitro. Following oral administration of a single 20 mg radiolabeled Cobimetinib dose, no oxidative metabolites >10% of total circulating radioactivity were observed. | [[CYP3A]] [[oxidation]] and [[UGT2B7]] [[glucuronidation]] were the major pathways of Cobimetinib metabolism [[in vitro]]. Following oral administration of a single 20 mg [[radiolabeled]] Cobimetinib dose, no oxidative [[metabolites]] >10% of total circulating [[radioactivity]] were observed. | ||
::*Excretion | ::*[[Excretion]] | ||
Following oral administration of a single 20 mg radiolabeled Cobimetinib dose, 76% of the dose was recovered in the feces (with 6.6% as unchanged drug) and 17.8% of the dose was recovered in the urine (with 1.6% as unchanged drug). | Following oral administration of a single 20 mg radiolabeled Cobimetinib dose, 76% of the dose was recovered in the feces (with 6.6% as unchanged drug) and 17.8% of the dose was recovered in the urine (with 1.6% as unchanged drug). | ||
| Line 254: | Line 266: | ||
Based on the population pharmacokinetic analysis, age (19–88 years), sex, or race/ethnicity does not have a clinically important effect on the systemic exposure of Cobimetinib. | Based on the population pharmacokinetic analysis, age (19–88 years), sex, or race/ethnicity does not have a clinically important effect on the systemic exposure of Cobimetinib. | ||
::*Hepatic Impairment | ::*[[Hepatic Impairment]] | ||
Following a single 10 mg Cobimetinib dose, the geometric mean total Cobimetinib exposure (AUC(inf)) values were similar in subjects with mild or moderate hepatic impairment and was decreased by 31% in subjects with severe hepatic impairment compared to subjects with normal hepatic function. | Following a single 10 mg Cobimetinib dose, the geometric mean total Cobimetinib exposure ([[AUC]](inf)) values were similar in subjects with mild or moderate hepatic impairment and was decreased by 31% in subjects with severe hepatic impairment compared to subjects with normal [[hepatic function]]. | ||
::*Renal Impairment | ::*[[Renal Impairment]] | ||
Cobimetinib undergoes minimal renal elimination. Cobimetinib exposures were similar in 151 patients with mild renal impairment (CLcr 60 to 89 mL/min), 48 patients with moderate renal impairment (CLcr 30 to 59 mL/min) and 286 patients with normal renal function (CLcr ≥90 mL/min). | Cobimetinib undergoes minimal renal elimination. Cobimetinib exposures were similar in 151 patients with mild renal impairment ([[CLcr]] 60 to 89 mL/min), 48 patients with moderate renal impairment (CLcr 30 to 59 mL/min) and 286 patients with normal [[renal function]] (CLcr ≥90 mL/min). | ||
:*'''Drug Interaction Studies''' | :*'''Drug Interaction Studies''' | ||
::*Vemurafenib: Coadministration of Cobimetinib 60 mg once daily and vemurafenib 960 mg twice daily resulted in no clinically relevant pharmacokinetic drug interactions. | ::*[[Vemurafenib]]: Coadministration of Cobimetinib 60 mg once daily and vemurafenib 960 mg twice daily resulted in no clinically relevant [[pharmacokinetic]] drug interactions. | ||
::*Effect of Strong and Moderate CYP3A Inhibitors on Cobimetinib: In vitro studies show that Cobimetinib is a substrate of CYP3A. Coadministration of itraconazole (a strong CYP3A inhibitor) 200 mg once daily for 14 days with a single 10 mg Cobimetinib dose increased mean Cobimetinib AUC (90% CI) by 6.7-fold (5.6, 8.0) and mean Cmax (90% CI) by 3.2-fold (2.7, 3.7) in 15 healthy subjects. Simulations showed that predicted steady-state concentrations of Cobimetinib at a reduced dose of 20 mg administered concurrently with short-term (less than 14 days) treatment of a moderate CYP3A inhibitor were similar to observed steady-state concentrations of Cobimetinib at the 60 mg dose alone. | ::*Effect of Strong and Moderate [[CYP3A]] Inhibitors on Cobimetinib: [[In vitro]] studies show that Cobimetinib is a substrate of CYP3A. Coadministration of [[itraconazole]] (a strong CYP3A inhibitor) 200 mg once daily for 14 days with a single 10 mg Cobimetinib dose increased mean Cobimetinib [[AUC]] (90% CI) by 6.7-fold (5.6, 8.0) and mean [[Cmax]] (90% CI) by 3.2-fold (2.7, 3.7) in 15 healthy subjects. Simulations showed that predicted steady-state concentrations of Cobimetinib at a reduced dose of 20 mg administered concurrently with short-term (less than 14 days) treatment of a moderate CYP3A inhibitor were similar to observed steady-state concentrations of Cobimetinib at the 60 mg dose alone. | ||
::*Effect of Strong and Moderate CYP3A Inducers on Cobimetinib: Based on simulations, Cobimetinib exposures would decrease by 83% when coadministered with a strong CYP3A inducer and by 73% when coadministered with a moderate CYP3A inducer. | ::*Effect of Strong and Moderate [[CYP3A]] Inducers on Cobimetinib: Based on simulations, Cobimetinib exposures would decrease by 83% when coadministered with a strong CYP3A inducer and by 73% when coadministered with a moderate CYP3A inducer. | ||
::*Effect of Cobimetinib on CYP Substrates: Coadministration of Cobimetinib 60 mg once daily for 15 days with a single 30 mg dose of dextromethorphan (sensitive CYP2D6 substrate) or a single 2 mg dose of midazolam (sensitive CYP3A substrate) to 20 patients with solid tumors did not change dextromethorphan or midazolam systemic exposure. In vitro data indicated that Cobimetinib may inhibit CYP3A and CYP2D6. Cobimetinib at clinically relevant concentrations is not an inhibitor of CYP1A2, 2B6, 2C8, 2C9 and 2C19 or inducer of CYP1A2, 2B6 and 3A4. | ::*Effect of Cobimetinib on [[CYP]] Substrates: Coadministration of Cobimetinib 60 mg once daily for 15 days with a single 30 mg dose of [[dextromethorphan]] (sensitive [[CYP2D6]] substrate) or a single 2 mg dose of [[midazolam]] (sensitive CYP3A substrate) to 20 patients with solid tumors did not change dextromethorphan or midazolam systemic exposure. [[In vitro]] data indicated that Cobimetinib may inhibit [[CYP3A]] and [[CYP2D6]]. Cobimetinib at clinically relevant concentrations is not an inhibitor of [[CYP1A2]], 2B6, 2C8, 2C9 and 2C19 or inducer of [[CYP1A2]], 2B6 and 3A4. | ||
::*Effect of Transporters on Cobimetinib: Cobimetinib is a substrate of efflux transporter P-glycoprotein (P-gp), but is not a substrate of Breast Cancer Resistance Protein (BCRP), Organic Anion Transporting Polypeptide (OATP1B1 or OATP1B3) or Organic Cation Transporter (OCT1) in vitro. Drugs that inhibit P-gp may increase Cobimetinib concentrations. | ::*Effect of Transporters on Cobimetinib: Cobimetinib is a substrate of efflux transporter [[P-glycoprotein]] (P-gp), but is not a substrate of [[Breast Cancer Resistance Protein]] (BCRP), [[Organic Anion Transporting Polypeptide]] (OATP1B1 or OATP1B3) or [[Organic Cation Transporter]] (OCT1) [[in vitro]]. Drugs that inhibit [[P-gp]] may increase Cobimetinib concentrations. | ||
::*Effect of Cobimetinib on Transporters: In vitro data suggest that Cobimetinib at clinically relevant concentrations does not inhibit P-gp, BCRP, OATP1B1, OATP1B3, OCT1, OAT1, OAT3, or OCT2. | ::*Effect of Cobimetinib on Transporters: [[In vitro]] data suggest that Cobimetinib at clinically relevant concentrations does not inhibit [[P-gp]], [[BCRP]], [[OATP1B1]], [[OATP1B3]], [[OCT1]], [[OAT1]], [[OAT3]], or [[OCT2]]. | ||
::*Effect of Gastric Acid Reducing Drugs on Cobimetinib: Coadministration of a proton pump inhibitor, rabeprazole 20 mg once daily for 5 days, with a single dose of 20 mg Cobimetinib under fed and fasted conditions did not result in a clinically important change in Cobimetinib exposure. | ::*Effect of [[Gastric Acid]] Reducing Drugs on Cobimetinib: Coadministration of a [[proton pump inhibitor]], [[rabeprazole]] 20 mg once daily for 5 days, with a single dose of 20 mg Cobimetinib under fed and fasted conditions did not result in a clinically important change in Cobimetinib exposure. | ||
|nonClinToxic=:*Carcinogenesis, Mutagenesis, Impairment of Fertility | |nonClinToxic=:*[[Carcinogenesis]], [[Mutagenesis]], Impairment of [[Fertility]] | ||
Carcinogenicity studies with Cobimetinib have not been conducted. Cobimetinib was not genotoxic in studies evaluating reverse mutations in bacteria, chromosomal aberrations in mammalian cells, and micronuclei in bone marrow of rats. | [[Carcinogenicity]] studies with Cobimetinib have not been conducted. Cobimetinib was not [[genotoxic]] in studies evaluating reverse mutations in bacteria, [[chromosomal aberrations]] in mammalian cells, and [[micronuclei]] in [[bone marrow]] of rats. | ||
No dedicated fertility studies have been performed with Cobimetinib in animals; however, effects on reproductive tissues observed in general toxicology studies conducted in animals suggest that there is potential for Cobimetinib to impair fertility. In female rats, degenerative changes included increased apoptosis/necrosis of corpora lutea and vaginal epithelial cells at Cobimetinib doses approximately twice those in humans at the clinically recommended dose of 60 mg based on body surface area. In male dogs, testicular degeneration occurred at exposures as low as approximately 0.1 times the exposure in humans at the clinically recommended dose of 60 mg. | No dedicated fertility studies have been performed with Cobimetinib in animals; however, effects on [[reproductive tissues]] observed in general [[toxicology]] studies conducted in animals suggest that there is potential for Cobimetinib to impair fertility. In female rats, degenerative changes included increased [[apoptosis]]/[[necrosis]] of [[corpora lutea]] and [[vaginal epithelial cells]] at Cobimetinib doses approximately twice those in humans at the clinically recommended dose of 60 mg based on [[body surface area]]. In male dogs, [[testicular degeneration]] occurred at exposures as low as approximately 0.1 times the exposure in humans at the clinically recommended dose of 60 mg. | ||
|clinicalStudies=The safety and efficacy of Cobimetinib was established in a multicenter, randomized (1:1), double-blinded, placebo-controlled trial conducted in 495 patients with previously untreated, BRAF V600 mutation-positive, unresectable or metastatic, melanoma. The presence of BRAF V600 mutation was detected using the cobas® 4800 BRAF V600 mutation test. All patients received vemurafenib 960 mg orally twice daily on days 1–28 and were randomized to receive Cobimetinib 60 mg or matching placebo orally once daily on days 1–21 of an every 28-day cycle. Randomization was stratified by geographic region (North America vs. Europe vs. Australia/New Zealand/others) and disease stage (unresectable Stage IIIc, M1a, or M1b vs. Stage M1c). Treatment continued until disease progression or unacceptable toxicity. Patients randomized to receive placebo were not offered Cobimetinib at the time of disease progression. | |clinicalStudies=The safety and efficacy of Cobimetinib was established in a [[multicenter]], [[randomized]] (1:1), [[double-blinded]], [[placebo]]-controlled [[trial]] conducted in 495 patients with previously untreated, [[BRAF]] [[V600]] mutation-positive, [[unresectable]] or [[metastatic]], [[melanoma]]. The presence of BRAF V600 mutation was detected using the cobas® 4800 BRAF V600 mutation test. All patients received vemurafenib 960 mg orally twice daily on days 1–28 and were randomized to receive Cobimetinib 60 mg or matching placebo orally once daily on days 1–21 of an every 28-day cycle. Randomization was stratified by geographic region (North America vs. Europe vs. Australia/New Zealand/others) and disease stage (unresectable Stage IIIc, M1a, or M1b vs. Stage M1c). Treatment continued until [[disease progression]] or unacceptable [[toxicity]]. Patients randomized to receive placebo were not offered Cobimetinib at the time of disease progression. | ||
The major efficacy outcome was investigator-assessed progression-free survival (PFS) per RECIST v1.1. Additional efficacy outcomes were investigator-assessed confirmed objective response rate, overall survival, PFS as assessed by blinded independent central review, and duration of response. | The major efficacy outcome was investigator-assessed progression-free survival (PFS) per RECIST v1.1. Additional efficacy outcomes were investigator-assessed confirmed objective response rate, overall survival, PFS as assessed by blinded independent central review, and duration of response. | ||
The median age of the study population was 55 years (range 23 to 88 years), 58% of patients were male, 93% were White and 5% had no race reported, 60% had stage M1c disease, 72% had a baseline ECOG performance status of 0, 45% had an elevated baseline serum lactate dehydrogenase (LDH), 10% had received prior adjuvant therapy, and <1% had previously treated brain metastases. Patients with available tumor samples were retrospectively tested using next generation sequencing to further classify mutations as V600E or V600K; test results were obtained on 81% of randomized patients. Of these, 86% were identified as having a V600E mutation and 14% as having a V600K mutation. | The median age of the study population was 55 years (range 23 to 88 years), 58% of patients were male, 93% were White and 5% had no race reported, 60% had stage M1c disease, 72% had a baseline [[ECOG]] performance status of 0, 45% had an elevated baseline serum [[lactate dehydrogenase]] (LDH), 10% had received prior adjuvant therapy, and <1% had previously treated [[brain metastases]]. Patients with available tumor samples were retrospectively tested using next generation sequencing to further classify mutations as [[V600E]] or [[V600K]]; test results were obtained on 81% of randomized patients. Of these, 86% were identified as having a V600E mutation and 14% as having a V600K mutation. | ||
Efficacy results are summarized in TABLE 5 and FIGURE 1. | Efficacy results are summarized in TABLE 5 and FIGURE 1. | ||
:*'''Table 5 Efficacy Results from Trial 1''' | |||
[[File:table5_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
COTELLIC: Cobimetinib's Brand name | |||
:*'''Figure 1 Kaplan-Meier Curves of Overall Survival''' | |||
[[File:figure1_cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
The effect on PFS was also supported by analysis of PFS based on the assessment by blinded independent review. A trend favoring the Cobimetinib with vemurafenib arm was observed in exploratory subgroup analyses of PFS, OS, and ORR in both BRAF V600 mutation subtypes (V600E or V600K) in the 81% of patients in this trial where BRAF V600 mutation type was determined. | The effect on PFS was also supported by analysis of PFS based on the assessment by blinded independent review. A trend favoring the Cobimetinib with [[vemurafenib]] arm was observed in exploratory subgroup analyses of PFS, OS, and ORR in both BRAF V600 mutation subtypes ([[V600E]] or [[V600K]]) in the 81% of patients in this trial where BRAF V600 mutation type was determined. | ||
|howSupplied=Cobimetinib is supplied as 20 mg film-coated tablets debossed on one side with "COB". Cobimetinib tablets are available in bottles of 63 tablets. | |howSupplied=Cobimetinib is supplied as 20 mg film-coated tablets debossed on one side with "COB". Cobimetinib tablets are available in bottles of 63 tablets. | ||
(NDC 50242-717-01) | (NDC 50242-717-01) | ||
|storage=Store at room temperature below 30°C (86°F). | |storage=Store at room temperature below 30°C (86°F). | ||
|packLabel=[[File:cobi.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|fdaPatientInfo=Inform patients of the following: | |fdaPatientInfo=Inform patients of the following: | ||
:*New primary cutaneous malignancies: Advise patients to contact their health care provider immediately for change in or development of new skin lesions. | :*New primary cutaneous malignancies: Advise patients to contact their health care provider immediately for change in or development of new [[skin lesions]]. | ||
:*Hemorrhage: Instruct patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual severe bleeding or hemorrhage. | :*[[Hemorrhage]]: Instruct patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual severe [[bleeding]] or [[hemorrhage]]. | ||
:*Cardiomyopathy: Advise patients to report any history of cardiac disease and of the requirement for cardiac monitoring prior to and during Cobimetinib administration. Instruct patients to immediately report any signs or symptoms of left ventricular dysfunction to their healthcare provider. | :*[[Cardiomyopathy]]: Advise patients to report any history of [[cardiac disease]] and of the requirement for [[cardiac monitoring]] prior to and during Cobimetinib administration. Instruct patients to immediately report any signs or symptoms of [[left ventricular dysfunction]] to their [[healthcare provider]]. | ||
:*Serious dermatologic reactions: Instruct patients to contact their healthcare provider to immediately report severe skin changes. | :*Serious [[dermatologic reactions]]: Instruct patients to contact their healthcare provider to immediately report severe skin changes. | ||
:*Serous retinopathy and retinal vein occlusion: Instruct patients to immediately contact their healthcare provider if they experience any changes in their vision. | :*Serous [[retinopathy]] and [[retinal vein occlusion]]: Instruct patients to immediately contact their healthcare provider if they experience any changes in their vision. | ||
:*Hepatotoxicity: Advise patients that treatment with Cobimetinib requires monitoring of their liver function. Instruct patients to report any signs or symptoms of liver dysfunction. | :*[[Hepatotoxicity]]: Advise patients that treatment with Cobimetinib requires monitoring of their [[liver function]]. Instruct patients to report any signs or symptoms of liver dysfunction. | ||
:*Rhabdomyolysis: Instruct patients to report any signs and symptoms of muscle pain or weakness to their healthcare provider. | :*[[Rhabdomyolysis]]: Instruct patients to report any signs and symptoms of [[muscle pain]] or [[weakness]] to their healthcare provider. | ||
:*Severe photosensitivity: Advise patients to avoid sun exposure, wear protective clothing, and use broad spectrum UVA/UVB sunscreen and lip balm (SPF ≥30) when outdoors. | :*Severe [[photosensitivity]]: Advise patients to avoid sun exposure, wear protective clothing, and use broad spectrum [[UVA]]/[[UVB]] sunscreen and lip balm (SPF ≥30) when outdoors. | ||
:*Embryo-fetal toxicity: Advise females of reproductive potential of the potential risk to a fetus. Advise females to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with Cobimetinib. | :*Embryo-fetal toxicity: Advise females of reproductive potential of the potential risk to a fetus. Advise females to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with Cobimetinib. | ||
:*Females of reproductive potential: Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib and for at least 2 weeks after the final dose of Cobimetinib. | :*Females of reproductive potential: Advise females of reproductive potential to use effective [[contraception]] during treatment with Cobimetinib and for at least 2 weeks after the final dose of Cobimetinib. | ||
:*Lactation: Advise females not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose. | :*Lactation: Advise females not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose. | ||
|brandNames=COTELLIC® | |brandNames=COTELLIC® | ||
}} | }} | ||
Latest revision as of 15:32, 20 January 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Cobimetinib is a kinase inhibitor that is FDA approved for the treatment of patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in combination with vemurafenib. Common adverse reactions include diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting (≥20%).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Cobimetinib is indicated for the treatment of patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in combination with vemurafenib
Dosage
- Patient Selection
Confirm the presence of BRAF V600E or V600K mutation in tumor specimens prior to initiation of treatment with Cobimetinib with vemurafenib. Information on FDA-approved tests for the detection of BRAF V600 mutations in melanoma is available at: http://www.fda.gov/CompanionDiagnostics.
- Recommended Dose
The recommended dosage regimen of Cobimetinib is 60 mg (three 20 mg tablets) orally taken once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity.
Take Cobimetinib with or without food.
If a dose of Cobimetinib is missed or if vomiting occurs when the dose is taken, resume dosing with the next scheduled dose.
- Dose Modifications
- Concurrent CYP3A Inhibitors
Do not take strong or moderate CYP3A inhibitors while taking Cobimetinib.
If concurrent short term (14 days or less) use of moderate CYP3A inhibitors is unavoidable for patients who are taking Cobimetinib 60 mg, reduce Cobimetinib dose to 20 mg. After discontinuation of a moderate CYP3A inhibitor, resume previous dose of Cobimetinib 60 mg.
Use an alternative to a strong or moderate CYP3A inhibitor in patients who are taking a reduced dose of Cobimetinib (40 or 20 mg daily).
- Adverse Reactions
Review the Full Prescribing Information for vemurafenib for recommended dose modifications.
- Table 1. Recommended Dose Reductions for Cobimetinib
COTELLIC: Cobimetinib's Brand name
- Table 2. Recommended Dose Modifications for Cobimetinib for Adverse Reactions
COTELLIC: Cobimetinib's Brand name
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cobimetinib in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Cobimetinib in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of Cobimetinib have not been established in pediatric patients
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cobimetinib in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Cobimetinib in pediatric patients.
Contraindications
None
Warnings
Review the Full Prescribing Information for vemurafenib for information on the serious risks of vemurafenib.
- New Primary Malignancies
New primary malignancies, cutaneous and non-cutaneous, can occur with Cobimetinib.
- Cutaneous Malignancies:
In Trial 1, the following cutaneous malignancies or premalignant conditions occurred in the Cobimetinib with vemurafenib arm and the vemurafenib arm, respectively: cutaneous squamous cell carcinoma (cuSCC) or keratoacanthoma (KA) (6% and 20%), basal cell carcinoma (4.5% and 2.4%), and second primary melanoma (0.8% and 2.4%). Among patients receiving Cobimetinib with vemurafenib, the median time to detection of first cuSCC/KA was 4 months (range: 2 to 11 months), and the median time to detection of basal cell carcinoma was 4 months (range: 27 days to 13 months). The time to onset in the two patients with second primary melanoma was 9 months and 12 months.
Perform dermatologic evaluations prior to initiation of therapy and every 2 months while on therapy. Manage suspicious skin lesions with excision and dermatopathologic evaluation. No dose modifications are recommended for Cobimetinib. Conduct dermatologic monitoring for 6 months following discontinuation of Cobimetinib when administered with vemurafenib.
- Non-Cutaneous Malignancies:
Based on its mechanism of action, vemurafenib may promote growth and development of malignancies [refer to the Full Prescribing Information for vemurafenib]. In Trial 1, 0.8% of patients in the Cobimetinib with vemurafenib arm and 1.2% of patients in the vemurafenib arm developed non-cutaneous malignancies.
Monitor patients receiving Cobimetinib, when administered with vemurafenib, for signs or symptoms of non-cutaneous malignancies.
Hemorrhage, including major hemorrhages defined as symptomatic bleeding in a critical area or organ, can occur with Cobimetinib.
In Trial 1, the incidence of Grade 3–4 hemorrhages was 1.2% in patients receiving Cobimetinib with vemurafenib and 0.8% in patients receiving vemurafenib. Hemorrhage (all grades) was 13% in patients receiving Cobimetinib with vemurafenib and 7% in patients receiving vemurafenib. Cerebral hemorrhage occurred in 0.8% of patients receiving Cobimetinib with vemurafenib and in none of the patients receiving vemurafenib. Gastrointestinal tract hemorrhage (3.6% vs 1.2%), reproductive system hemorrhage (2.0% vs 0.4%), and hematuria (2.4% vs 0.8%) also occurred at a higher incidence in patients receiving Cobimetinib with vemurafenib compared with patients receiving vemurafenib.
Withhold Cobimetinib for Grade 3 hemorrhagic events. If improved to Grade 0 or 1 within 4 weeks, resume Cobimetinib at a lower dose level. Discontinue Cobimetinib for Grade 4 hemorrhagic events and any Grade 3 hemorrhagic events that do not improve.
Cardiomyopathy, defined as symptomatic and asymptomatic decline in left ventricular ejection fraction (LVEF), can occur with Cobimetinib . The safety of Cobimetinib has not been established in patients with a baseline LVEF that is either below institutional lower limit of normal (LLN) or below 50%.
In Trial 1, patients were assessed for decreases in LVEF by echocardiograms or MUGA at baseline, Week 5, Week 17, Week 29, Week 43, and then every 4 to 6 months thereafter while receiving treatment. Grade 2 or 3 decrease in LVEF occurred in 26% of patients receiving Cobimetinib with vemurafenib and 19% of patients receiving vemurafenib. The median time to first onset of LVEF decrease was 4 months (range 23 days to 13 months). Of the patients with decreased LVEF, 22% had dose interruption and/or reduction and 14% required permanent discontinuation. Decreased LVEF resolved to above the LLN or within 10% of baseline in 62% of patients receiving Cobimetinib with a median time to resolution of 3 months (range: 4 days to 12 months).
Evaluate LVEF prior to initiation, 1 month after initiation, and every 3 months thereafter until discontinuation of Cobimetinib. Manage events of left ventricular dysfunction through treatment interruption, reduction, or discontinuation. In patients restarting Cobimetinib after a dose reduction or interruption, evaluate LVEF at approximately 2 weeks, 4 weeks, 10 weeks, and 16 weeks, and then as clinically indicated.
- Severe Dermatologic Reactions
Severe rash and other skin reactions can occur with Cobimetinib.
In Trial 1, Grade 3 to 4 rash, occurred in 16% of patients receiving Cobimetinib with vemurafenib and in 17% of patients receiving vemurafenib, including Grade 4 rash in 1.6% of patients receiving Cobimetinib with vemurafenib and 0.8% of the patients receiving vemurafenib. The incidence of rash resulting in hospitalization was 3.2% in patients receiving Cobimetinib with vemurafenib and 2.0% in patients receiving vemurafenib. In patients receiving Cobimetinib, the median time to onset of Grade 3 or 4 rash events was 11 days (range: 3 days to 2.8 months). Among patients with Grade 3 or 4 rash events, 95% experienced complete resolution with the median time to resolution of 21 days (range 4 days to 17 months).
Interrupt, reduce the dose, or discontinue Cobimetinib.
- Serous Retinopathy and Retinal Vein Occlusion
Ocular toxicities can occur with Cobimetinib, including serous retinopathy (fluid accumulation under layers of the retina).
In Trial 1, ophthalmologic examinations including retinal evaluation were performed pretreatment and at regular intervals during treatment. Symptomatic and asymptomatic serous retinopathy was identified in 26% of patients receiving Cobimetinib with vemurafenib. The majority of these events were reported as chorioretinopathy (13%) or retinal detachment (12%). The time to first onset of serous retinopathy events ranged between 2 days to 9 months. The reported duration of serous retinopathy ranged between 1 day to 15 months. One patient in each arm developed retinal vein occlusion.
Perform an ophthalmological evaluation at regular intervals and any time a patient reports new or worsening visual disturbances. If serous retinopathy is diagnosed, interrupt Cobimetinib until visual symptoms improve. Manage serous retinopathy with treatment interruption, dose reduction, or with treatment discontinuation.
Hepatotoxicity can occur with Cobimetinib.
The incidences of Grade 3 or 4 liver laboratory abnormalities in Trial 1 among patients receiving Cobimetinib with vemurafenib compared to patients receiving vemurafenib were: 11% vs. 5% for alanine aminotransferase, 8% vs. 2.1% for aspartate aminotransferase, 1.6% vs. 1.2% for total bilirubin, and 7% vs. 3.3% for alkaline phosphatase. Concurrent elevation in ALT >3 times the upper limit of normal (ULN) and bilirubin >2 × ULN in the absence of significant alkaline phosphatase >2 × ULN occurred in one patient (0.4%) receiving Cobimetinib with vemurafenib and no patients receiving single-agent vemurafenib.
Monitor liver laboratory tests before initiation of Cobimetinib and monthly during treatment, or more frequently as clinically indicated. Manage Grade 3 and 4 liver laboratory abnormalities with dose interruption, reduction, or discontinuation of Cobimetinib.
Rhabdomyolysis can occur with Cobimetinib.
In Trial 1, Grade 3 or 4 CPK elevations, including asymptomatic elevations over baseline, occurred in 14% of patients receiving Cobimetinib with vemurafenib and 0.5% of patients receiving vemurafenib. The median time to first occurrence of Grade 3 or 4 CPK elevations was 16 days (range: 12 days to 11 months) in patients receiving Cobimetinib with vemurafenib; the median time to complete resolution was 15 days (range: 9 days to 11 months). Elevation of serum CPK increase of more than 10 times the baseline value with a concurrent increase in serum creatinine of 1.5 times or greater compared to baseline occurred in 3.6% of patients receiving Cobimetinib with vemurafenib and in 0.4% of patients receiving vemurafenib.
Obtain baseline serum CPK and creatinine levels prior to initiating Cobimetinib, periodically during treatment, and as clinically indicated. If CPK is elevated, evaluate for signs and symptoms of rhabdomyolysis or other causes. Depending on the severity of symptoms or CPK elevation, dose interruption or discontinuation of Cobimetinib may be required.
- Severe Photosensitivity
Photosensitivity, including severe cases, can occur with Cobimetinib.
In Trial 1, photosensitivity was reported in 47% of patients receiving Cobimetinib with vemurafenib: 43% of patients with Grades 1 or 2 photosensitivity and the remaining 4% with Grade 3 photosensitivity. Median time to first onset of photosensitivity of any grade was 2 months (range: 1 day to 14 months) in patients receiving Cobimetinib with vemurafenib, and the median duration of photosensitivity was 3 months (range: 2 days to 14 months). Among the 47% of patients with photosensitivity reactions on Cobimetinib with vemurafenib, 63% experienced resolution of photosensitivity reactions.
Advise patients to avoid sun exposure, wear protective clothing and use a broad-spectrum UVA/UVB sunscreen and lip balm (SPF ≥30) when outdoors. Manage intolerable Grade 2 or greater photosensitivity with dose modifications.
- Embryo-Fetal Toxicity
Based on its mechanism of action and findings from animal reproduction studies, Cobimetinib can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during the period of organogenesis was teratogenic and embryotoxic at doses resulting in exposures [area under the curves (AUCs)] that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib, and for 2 weeks following the final dose of Cobimetinib.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of Cobimetinib was evaluated in Trial 1, a randomized (1:1), double-blind, active-controlled trial in previously untreated patients with BRAF V600 mutation-positive, unresectable or metastatic melanoma. All patients received vemurafenib 960 mg twice daily on Days 1–28 and received either Cobimetinib 60 mg once daily (n=247) or placebo (n=246) on Days 1–21 of each 28-day treatment cycle until disease progression or unacceptable toxicity. In the Cobimetinib plus vemurafenib arm, 66% percent of patients were exposed for greater than 6 months and 24% of patients were exposed for greater than 1 year. Patients with abnormal liver function tests, history of acute coronary syndrome within 6 months, evidence of Class II or greater congestive heart failure (New York Heart Association), active central nervous system lesions, or evidence of retinal pathology were excluded from Trial 1. The demographics and baseline tumor characteristics of patients enrolled in Trial 1 are summarized in Clinical Studies.
In Trial 1, 15% of patients receiving Cobimetinib experienced an adverse reaction that resulted in permanent discontinuation of Cobimetinib. The most common adverse reactions resulting in permanent discontinuation were liver laboratory abnormalities defined as increased aspartate aminotransferase (AST) (2.4%), increased gamma glutamyltransferase (GGT) (1.6%) and increased alanine aminotransferase (ALT) (1.6%); rash (1.6%); pyrexia (1.2%); and retinal detachment (2%). Among the 247 patients receiving Cobimetinib, adverse reactions led to dose interruption or reductions in 55%. The most common reasons for dose interruptions or reductions of Cobimetinib were rash (11%), diarrhea (9%), chorioretinopathy (7%), pyrexia (6%), vomiting (6%), nausea (5%), and increased creatine phosphokinase (CPK) (4.9%). The most common (≥20%) adverse reactions with Cobimetinib were diarrhea, photosensitivity reaction, nausea, pyrexia, and vomiting.
- Table 3. Incidence of Adverse Drug Reactions Occurring in ≥10% (All Grades) of Patients Receiving Cobimetinib with Vemurafenib and at a Higher Incidence* than Patients Receiving Vemurafenib in Trial 1
COTELLIC: Cobimetinib's Brand name
Adverse reactions of vemurafenib which occurred at a lower rate in patients receiving Cobimetinib plus vemurafenib were alopecia (15%), hyperkeratosis (11%), and erythema (10%).
The following adverse reactions (all grades) of Cobimetinib were reported with <10% incidence in Trial 1:
Respiratory, thoracic and mediastinal disorders: Pneumonitis
- Table 4. Incidence of Laboratory Abnormalities Occurring in ≥10% (All Grades) or ≥2% (Grades 3–4) of Patients in Trial 1*
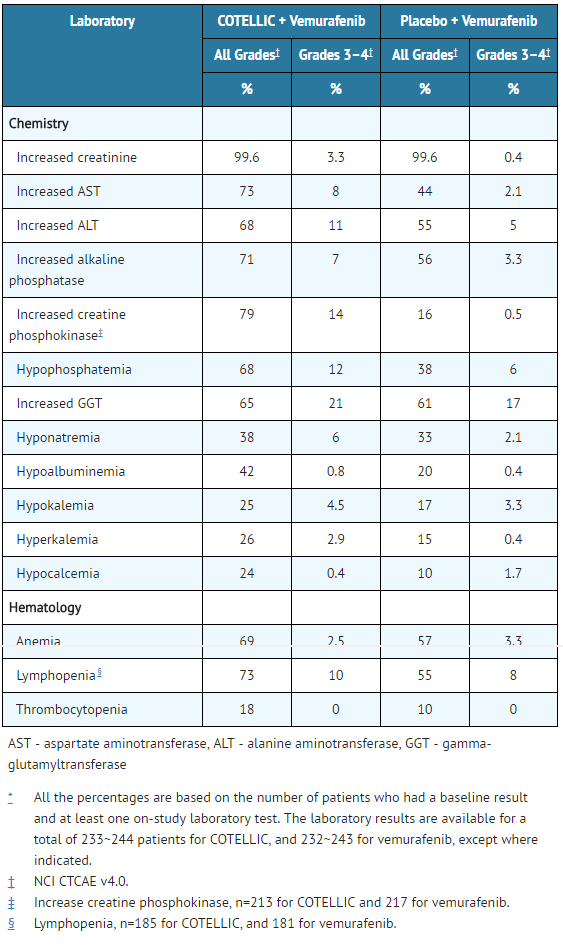
COTELLIC: Cobimetinib's Brand name
Postmarketing Experience
There is limited information regarding Cobimetinib Postmarketing Experience in the drug label.
Drug Interactions
- Effect of Strong or Moderate CYP3A Inhibitors on Cobimetinib
Coadministration of Cobimetinib with itraconazole (a strong CYP3A4 inhibitor) increased Cobimetinib systemic exposure by 6.7-fold. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inhibitors. If concurrent short term (14 days or less) use of moderate CYP3A inhibitors including certain antibiotics (e.g., erythromycin, ciprofloxacin) is unavoidable for patients who are taking Cobimetinib 60 mg, reduce Cobimetinib dose to 20 mg. After discontinuation of a moderate CYP3A inhibitor, resume Cobimetinib at the previous dose. Use an alternative to a strong or moderate CYP3A inhibitor in patients who are taking a reduced dose of Cobimetinib (40 or 20 mg daily).
- Effect of Strong or Moderate CYP3A Inducers on Cobimetinib
Coadministration of Cobimetinib with a strong CYP3A inducer may decrease Cobimetinib systemic exposure by more than 80% and reduce its efficacy. Avoid concurrent use of Cobimetinib and strong or moderate CYP3A inducers including but not limited to carbamazepine, efavirenz, phenytoin, rifampin, and St. John's Wort.
Use in Specific Populations
Pregnancy
- Risk Summary
Based on findings from animal reproduction studies and its mechanism of action, Cobimetinib can cause fetal harm when administered to a pregnant woman. There are no available data on the use of Cobimetinib during pregnancy. In animal reproduction studies, oral administration of Cobimetinib in pregnant rats during organogenesis was teratogenic and embryotoxic at exposures (AUC) that were 0.9 to 1.4-times those observed in humans at the recommended human dose of 60 mg. Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
- Data
- Animal Data
Administration of Cobimetinib to pregnant rats during the period of organogenesis resulted in increased post-implantation loss, including total litter loss, at exposures (AUC) of 0.9–1.4 times those in humans at the recommended dose of 60 mg. Post-implantation loss was primarily due to early resorptions. Fetal malformations of the great vessels and skull (eye sockets) occurred at the same exposures.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cobimetinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cobimetinib during labor and delivery.
Nursing Mothers
There is no information regarding the presence of Cobimetinib in human milk, effects on the breastfed infant, or effects on milk production. Because of the potential for serious adverse reactions in a breastfed infant, advise a nursing woman not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose.
Pediatric Use
The safety and effectiveness of Cobimetinib have not been established in pediatric patients.
- Juvenile Animal Data
In a 4-week juvenile rat toxicology study, daily oral doses of 3 mg/kg (approximately 0.13–0.5 times the adult human AUC at the recommended dose of 60 mg) between postnatal Days 10–17 (approximately equivalent to ages 1–2 years in humans) were associated with mortality, the cause of which was not defined.
Geriatic Use
Clinical studies of Cobimetinib did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients.
Gender
There is no FDA guidance on the use of Cobimetinib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Cobimetinib with respect to specific racial populations.
Renal Impairment
No dedicated pharmacokinetic trial in patients with renal impairment has been conducted. Dose adjustment is not recommended for mild to moderate renal impairment (CLcr 30 to 89 mL/min) based on the results of the population pharmacokinetic analysis. A recommended dose has not been established for patients with severe renal impairment.
Hepatic Impairment
Adjustment in the starting dose of Cobimetinib is not required in patients with mild (Child-Pugh score A), moderate (Child-Pugh B) or severe (Child-Pugh C) hepatic impairment.
Females of Reproductive Potential and Males
- Females
Cobimetinib can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib and for 2 weeks after the final dose of Cobimetinib.
- Females and Males
Based on findings in animals, Cobimetinib may reduce fertility in females and males of reproductive potential.
Immunocompromised Patients
There is no FDA guidance one the use of Cobimetinib in patients who are immunocompromised.
Administration and Monitoring
Administration
The recommended dosage regimen of Cobimetinib is 60 mg (three 20 mg tablets) orally taken once daily for the first 21 days of each 28-day cycle until disease progression or unacceptable toxicity.
- Take Cobimetinib with or without food.
- If a dose of Cobimetinib is missed or if vomiting occurs when the dose is taken, resume dosing with the next scheduled dose.
Monitoring
There is limited information regarding Cobimetinib Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Cobimetinib and IV administrations.
Overdosage
There is no information on overdosage of Cobimetinib.
Pharmacology
Mechanism of Action
Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1 (MEK1) and MEK2. MEK proteins are upstream regulators of the extracellular signal-related kinase (ERK) pathway, which promotes cellular proliferation. BRAF V600E and K mutations result in constitutive activation of the BRAF pathway which includes MEK1 and MEK2. In mice implanted with tumor cell lines expressing BRAF V600E, Cobimetinib inhibited tumor cell growth.
Cobimetinib and vemurafenib target two different kinases in the RAS/RAF/MEK/ERK pathway. Compared to either drug alone, coadministration of Cobimetinib and vemurafenib resulted in increased apoptosis in vitro and reduced tumor growth in mouse implantation models of tumor cell lines harboring BRAF V600E mutations. Cobimetinib also prevented vemurafenib-mediated growth enhancement of a wild-type BRAF tumor cell line in an in vivo mouse implantation model.
Structure
Cobimetinib is a fumarate salt appearing as white to off-white solid and exhibits a pH dependent solubility.
Cobimetinib tablets are supplied as white, round, film-coated 20 mg tablets for oral administration, debossed on one side with "COB". Each 20 mg tablet contains 22 mg of cobimetinib fumarate, which corresponds to 20 mg of the cobimetinib free base.
The inactive ingredients of Cobimetinib are: Tablet Core: microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate. Coating: polyvinyl alcohol, titanium dioxide, polyethylene glycol 3350, talc.
Pharmacodynamics
- Cardiac Electrophysiology
Clinically relevant QT prolongation has been reported with vemurafenib, further QTc prolongation was not observed when Cobimetinib 60 mg daily was co-administered with vemurafenib. Monitor ECG and electrolytes before initiating treatment and routinely during treatment with Cobimetinib, when administered with vemurafenib. Review the Full Prescribing Information for vemurafenib for details.
Pharmacokinetics
The pharmacokinetics of Cobimetinib was studied in healthy subjects and cancer patients. Cobimetinib exhibits linear pharmacokinetics in the dose range of 3.5 to 100 mg (i.e., 0.06 to 1.7 times the recommended dosage). Following oral administration of Cobimetinib 60 mg once daily, steady-state was reached by 9 days with a mean accumulation ratio of 2.4-fold (44% CV).
Following oral dosing of 60 mg once daily in cancer patients, the median time to achieve peak plasma levels (Tmax) was 2.4 (range:1–24) hours, geometric mean steady-state AUC(0-24h) was 4340 ng∙h/mL (61% CV) and Cmax was 273 ng/mL (60% CV). The absolute bioavailability of Cobimetinib was 46% (90% CI: 40%, 53%) in healthy subjects. A high-fat meal (comprised of approximately 150 calories from protein, 250 calories from carbohydrate, and 500–600 calories from fat) had no effect on Cobimetinib AUC and Cmax after a single 20 mg Cobimetinib was administered to healthy subjects.
Cobimetinib is 95% bound to human plasma proteins in vitro, independent of drug concentration. No preferential binding to human red blood cells was observed (blood to plasma ratio of 0.93). The estimated apparent volume of distribution was 806 L in cancer patients based on a population PK analysis.
Following oral administration of Cobimetinib 60 mg once daily in cancer patients, the mean elimination half-life (t1/2) was 44 (range: 23–70) hours and the mean apparent clearance (CL/F) was 13.8 L/h (61% CV).
CYP3A oxidation and UGT2B7 glucuronidation were the major pathways of Cobimetinib metabolism in vitro. Following oral administration of a single 20 mg radiolabeled Cobimetinib dose, no oxidative metabolites >10% of total circulating radioactivity were observed.
Following oral administration of a single 20 mg radiolabeled Cobimetinib dose, 76% of the dose was recovered in the feces (with 6.6% as unchanged drug) and 17.8% of the dose was recovered in the urine (with 1.6% as unchanged drug).
- Specific Populations
- Age, Sex, and Race/Ethnicity
Based on the population pharmacokinetic analysis, age (19–88 years), sex, or race/ethnicity does not have a clinically important effect on the systemic exposure of Cobimetinib.
Following a single 10 mg Cobimetinib dose, the geometric mean total Cobimetinib exposure (AUC(inf)) values were similar in subjects with mild or moderate hepatic impairment and was decreased by 31% in subjects with severe hepatic impairment compared to subjects with normal hepatic function.
Cobimetinib undergoes minimal renal elimination. Cobimetinib exposures were similar in 151 patients with mild renal impairment (CLcr 60 to 89 mL/min), 48 patients with moderate renal impairment (CLcr 30 to 59 mL/min) and 286 patients with normal renal function (CLcr ≥90 mL/min).
- Drug Interaction Studies
- Vemurafenib: Coadministration of Cobimetinib 60 mg once daily and vemurafenib 960 mg twice daily resulted in no clinically relevant pharmacokinetic drug interactions.
- Effect of Strong and Moderate CYP3A Inhibitors on Cobimetinib: In vitro studies show that Cobimetinib is a substrate of CYP3A. Coadministration of itraconazole (a strong CYP3A inhibitor) 200 mg once daily for 14 days with a single 10 mg Cobimetinib dose increased mean Cobimetinib AUC (90% CI) by 6.7-fold (5.6, 8.0) and mean Cmax (90% CI) by 3.2-fold (2.7, 3.7) in 15 healthy subjects. Simulations showed that predicted steady-state concentrations of Cobimetinib at a reduced dose of 20 mg administered concurrently with short-term (less than 14 days) treatment of a moderate CYP3A inhibitor were similar to observed steady-state concentrations of Cobimetinib at the 60 mg dose alone.
- Effect of Strong and Moderate CYP3A Inducers on Cobimetinib: Based on simulations, Cobimetinib exposures would decrease by 83% when coadministered with a strong CYP3A inducer and by 73% when coadministered with a moderate CYP3A inducer.
- Effect of Cobimetinib on CYP Substrates: Coadministration of Cobimetinib 60 mg once daily for 15 days with a single 30 mg dose of dextromethorphan (sensitive CYP2D6 substrate) or a single 2 mg dose of midazolam (sensitive CYP3A substrate) to 20 patients with solid tumors did not change dextromethorphan or midazolam systemic exposure. In vitro data indicated that Cobimetinib may inhibit CYP3A and CYP2D6. Cobimetinib at clinically relevant concentrations is not an inhibitor of CYP1A2, 2B6, 2C8, 2C9 and 2C19 or inducer of CYP1A2, 2B6 and 3A4.
- Effect of Transporters on Cobimetinib: Cobimetinib is a substrate of efflux transporter P-glycoprotein (P-gp), but is not a substrate of Breast Cancer Resistance Protein (BCRP), Organic Anion Transporting Polypeptide (OATP1B1 or OATP1B3) or Organic Cation Transporter (OCT1) in vitro. Drugs that inhibit P-gp may increase Cobimetinib concentrations.
- Effect of Gastric Acid Reducing Drugs on Cobimetinib: Coadministration of a proton pump inhibitor, rabeprazole 20 mg once daily for 5 days, with a single dose of 20 mg Cobimetinib under fed and fasted conditions did not result in a clinically important change in Cobimetinib exposure.
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with Cobimetinib have not been conducted. Cobimetinib was not genotoxic in studies evaluating reverse mutations in bacteria, chromosomal aberrations in mammalian cells, and micronuclei in bone marrow of rats.
No dedicated fertility studies have been performed with Cobimetinib in animals; however, effects on reproductive tissues observed in general toxicology studies conducted in animals suggest that there is potential for Cobimetinib to impair fertility. In female rats, degenerative changes included increased apoptosis/necrosis of corpora lutea and vaginal epithelial cells at Cobimetinib doses approximately twice those in humans at the clinically recommended dose of 60 mg based on body surface area. In male dogs, testicular degeneration occurred at exposures as low as approximately 0.1 times the exposure in humans at the clinically recommended dose of 60 mg.
Clinical Studies
The safety and efficacy of Cobimetinib was established in a multicenter, randomized (1:1), double-blinded, placebo-controlled trial conducted in 495 patients with previously untreated, BRAF V600 mutation-positive, unresectable or metastatic, melanoma. The presence of BRAF V600 mutation was detected using the cobas® 4800 BRAF V600 mutation test. All patients received vemurafenib 960 mg orally twice daily on days 1–28 and were randomized to receive Cobimetinib 60 mg or matching placebo orally once daily on days 1–21 of an every 28-day cycle. Randomization was stratified by geographic region (North America vs. Europe vs. Australia/New Zealand/others) and disease stage (unresectable Stage IIIc, M1a, or M1b vs. Stage M1c). Treatment continued until disease progression or unacceptable toxicity. Patients randomized to receive placebo were not offered Cobimetinib at the time of disease progression.
The major efficacy outcome was investigator-assessed progression-free survival (PFS) per RECIST v1.1. Additional efficacy outcomes were investigator-assessed confirmed objective response rate, overall survival, PFS as assessed by blinded independent central review, and duration of response.
The median age of the study population was 55 years (range 23 to 88 years), 58% of patients were male, 93% were White and 5% had no race reported, 60% had stage M1c disease, 72% had a baseline ECOG performance status of 0, 45% had an elevated baseline serum lactate dehydrogenase (LDH), 10% had received prior adjuvant therapy, and <1% had previously treated brain metastases. Patients with available tumor samples were retrospectively tested using next generation sequencing to further classify mutations as V600E or V600K; test results were obtained on 81% of randomized patients. Of these, 86% were identified as having a V600E mutation and 14% as having a V600K mutation.
Efficacy results are summarized in TABLE 5 and FIGURE 1.
- Table 5 Efficacy Results from Trial 1
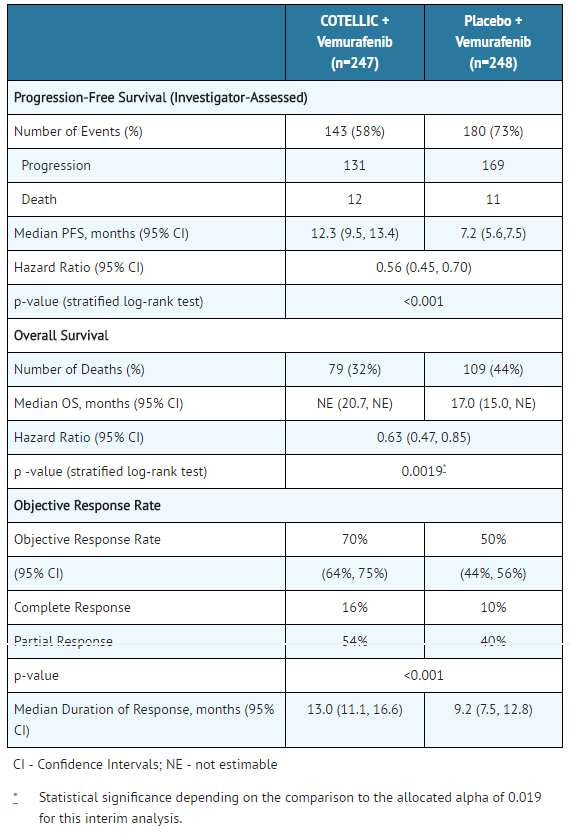
COTELLIC: Cobimetinib's Brand name
- Figure 1 Kaplan-Meier Curves of Overall Survival

The effect on PFS was also supported by analysis of PFS based on the assessment by blinded independent review. A trend favoring the Cobimetinib with vemurafenib arm was observed in exploratory subgroup analyses of PFS, OS, and ORR in both BRAF V600 mutation subtypes (V600E or V600K) in the 81% of patients in this trial where BRAF V600 mutation type was determined.
How Supplied
Cobimetinib is supplied as 20 mg film-coated tablets debossed on one side with "COB". Cobimetinib tablets are available in bottles of 63 tablets.
(NDC 50242-717-01)
Storage
Store at room temperature below 30°C (86°F).
Images
Drug Images
{{#ask: Page Name::Cobimetinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Cobimetinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Inform patients of the following:
- New primary cutaneous malignancies: Advise patients to contact their health care provider immediately for change in or development of new skin lesions.
- Hemorrhage: Instruct patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual severe bleeding or hemorrhage.
- Cardiomyopathy: Advise patients to report any history of cardiac disease and of the requirement for cardiac monitoring prior to and during Cobimetinib administration. Instruct patients to immediately report any signs or symptoms of left ventricular dysfunction to their healthcare provider.
- Serious dermatologic reactions: Instruct patients to contact their healthcare provider to immediately report severe skin changes.
- Serous retinopathy and retinal vein occlusion: Instruct patients to immediately contact their healthcare provider if they experience any changes in their vision.
- Hepatotoxicity: Advise patients that treatment with Cobimetinib requires monitoring of their liver function. Instruct patients to report any signs or symptoms of liver dysfunction.
- Rhabdomyolysis: Instruct patients to report any signs and symptoms of muscle pain or weakness to their healthcare provider.
- Severe photosensitivity: Advise patients to avoid sun exposure, wear protective clothing, and use broad spectrum UVA/UVB sunscreen and lip balm (SPF ≥30) when outdoors.
- Embryo-fetal toxicity: Advise females of reproductive potential of the potential risk to a fetus. Advise females to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with Cobimetinib.
- Females of reproductive potential: Advise females of reproductive potential to use effective contraception during treatment with Cobimetinib and for at least 2 weeks after the final dose of Cobimetinib.
- Lactation: Advise females not to breastfeed during treatment with Cobimetinib and for 2 weeks after the final dose.
Precautions with Alcohol
Alcohol-Cobimetinib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
COTELLIC®
Look-Alike Drug Names
There is limited information regarding Cobimetinib Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 Takahashi, RH; Choo, EF; Ma, S; Wong, S; Halladay, J; Deng, Y; Rooney, I; Gates, M; Hop, CE; Khojasteh, SC; Dresser, MJ; Musib, L (January 2016). "Absorption, Metabolism, Excretion, and the Contribution of Intestinal Metabolism to the Oral Disposition of [14C]Cobimetinib, a MEK Inhibitor, in Humans". Drug Metabolism and Disposition: the Biological Fate of Chemicals. 44 (1): 28–39. doi:10.1124/dmd.115.066282. PMID 26451002.
|access-date=requires|url=(help) - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Cotellic (cobimetinib) Tablets, for Oral Use. Full Prescribing Information" (PDF). Genentech USA, Inc., a Member of the Roche Group. 1 DNA Way, South San Francisco, CA 94080-4990. Retrieved 5 October 2016.
- ↑ Choo, E; Takahashi, R; Rooney, I; Gates, M; Deng, A; Musib, L (January 30, 2014). "Abstract B160: Assessing Human Absorption, Metabolism, Routes of Excretion and the Contribution of Intestinal Metabolism to the Oral Clearance of Cobimetinib, a MEK Inhibitor". Molecular Cancer Therapeutics. 12 (11 Supplement): B160. doi:10.1158/1535-7163.TARG-13-B160.
|access-date=requires|url=(help)