Coats disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 52: | Line 52: | ||
* [[Ultrasound]]: can detect the [[tumor]] as a result of the [[Calcification|calcifications]] inside. | * [[Ultrasound]]: can detect the [[tumor]] as a result of the [[Calcification|calcifications]] inside. | ||
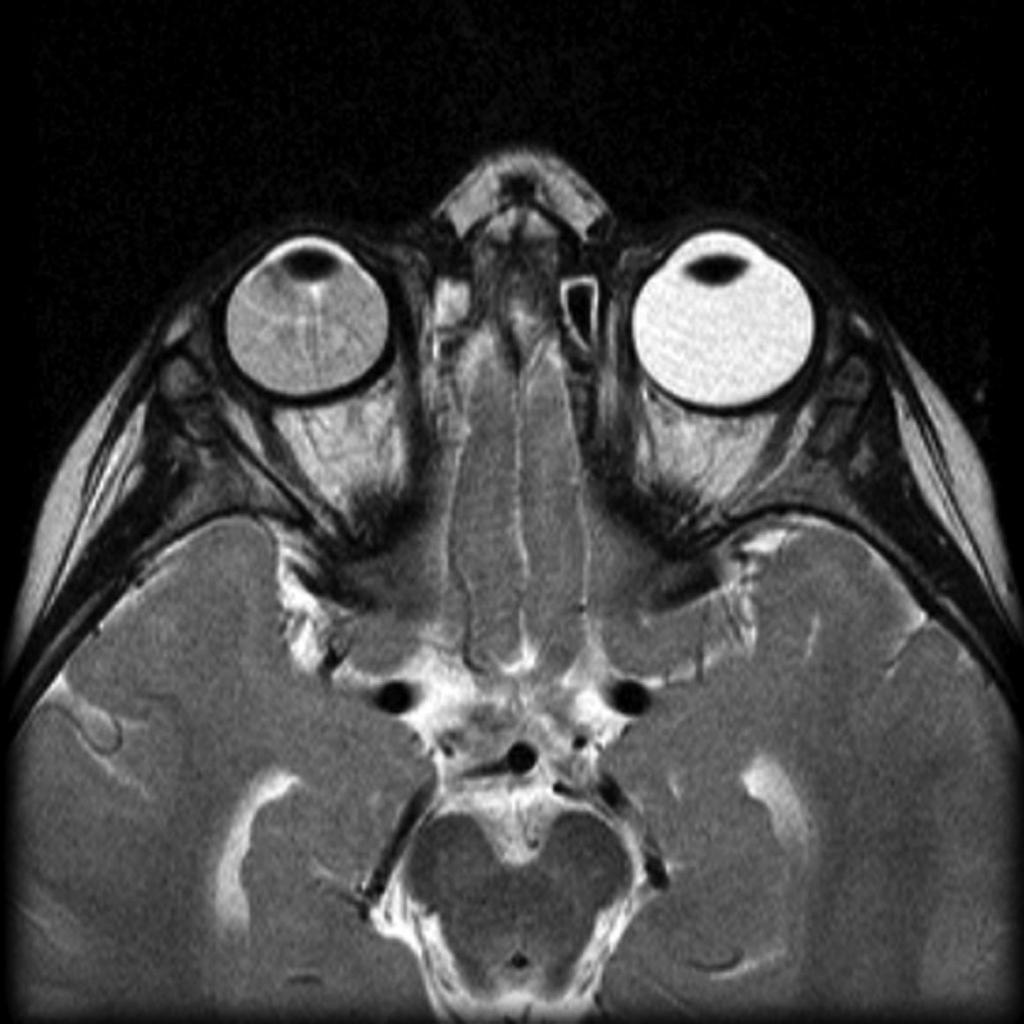
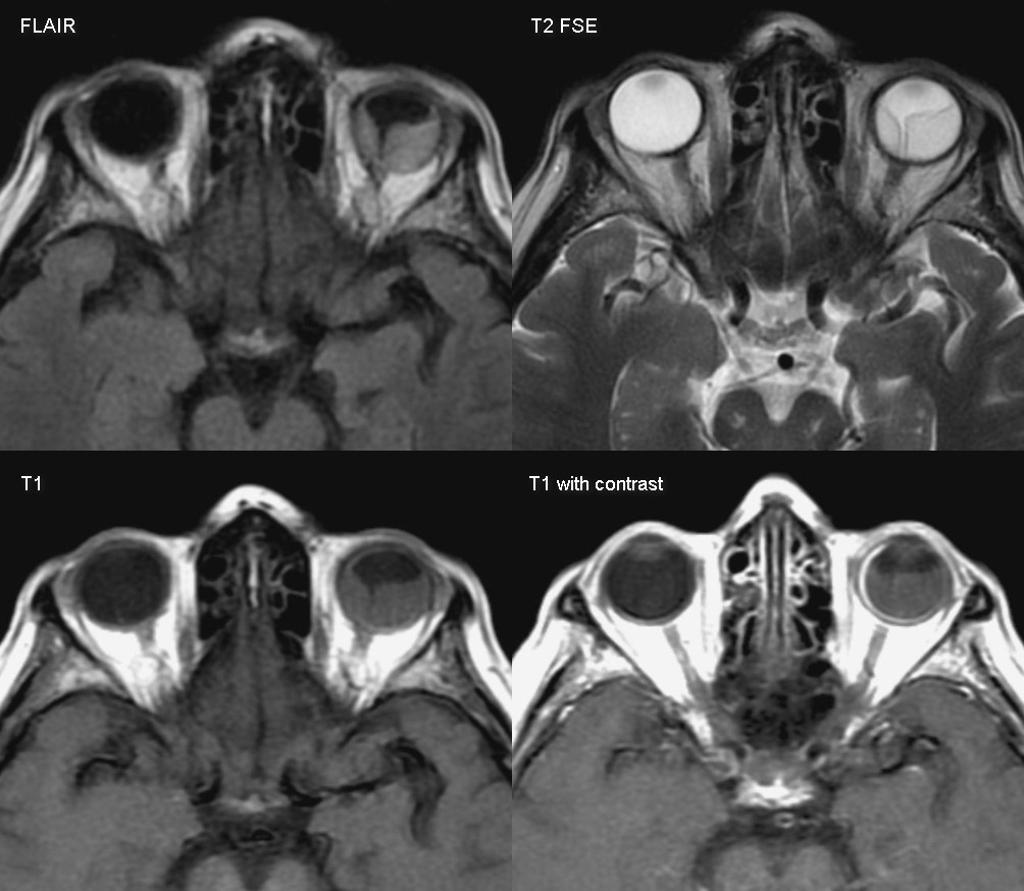
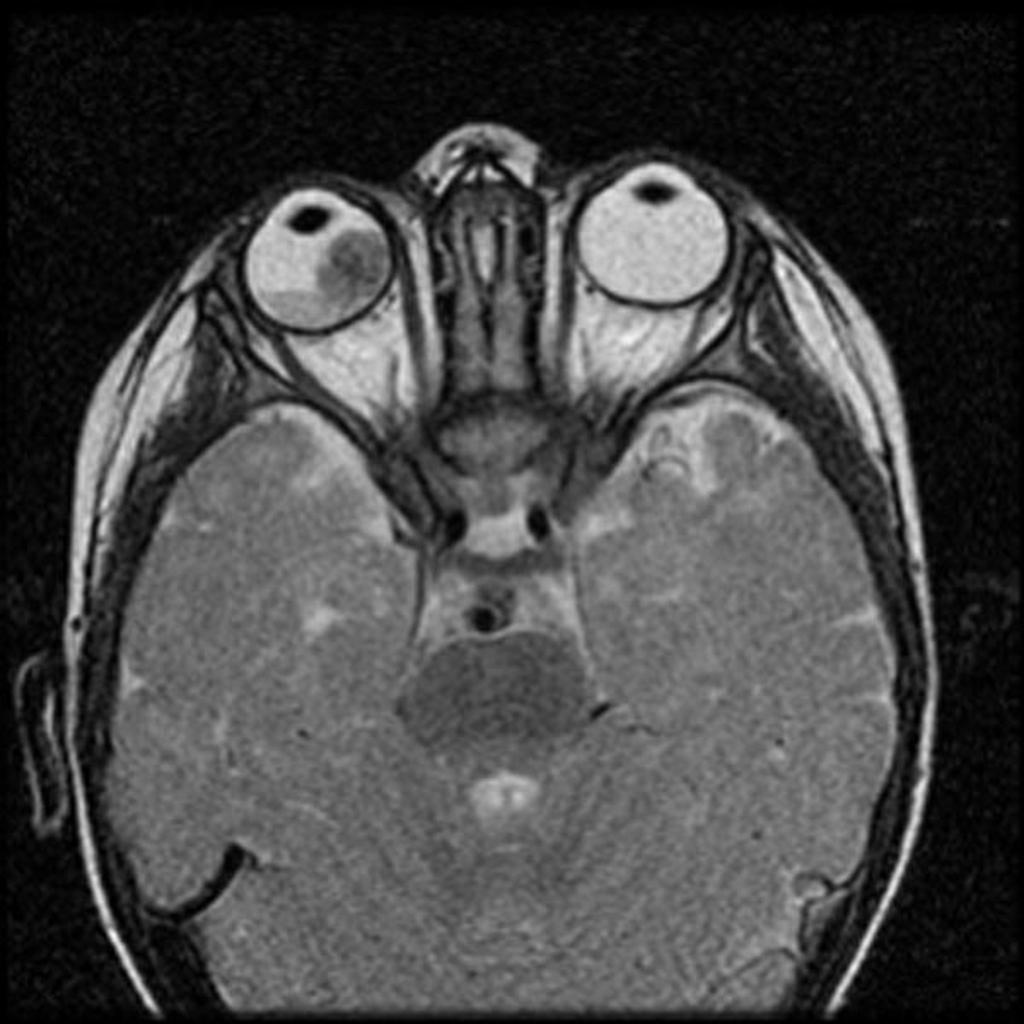
* [[MRI|MRI:]] assess [[Sella turcica|sellar]] and [[Parasellar and suprasellar disorders|parasellar]] regions .. it can also detect extraocular spread of the [[tumor]].<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | * [[MRI|MRI:]] assess [[Sella turcica|sellar]] and [[Parasellar and suprasellar disorders|parasellar]] regions .. it can also detect extraocular spread of the [[tumor]].<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | ||
|} | |||
Coats’ disease must be differentiated from [[retinoblastoma]], [[Norrie disease]], and [[Retinopathy of prematurity]] ([[Retinopathy of prematurity|ROP]]).<ref name="pmid11875173">{{cite journal |vauthors=Butros LJ, Abramson DH, Dunkel IJ |title=Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences |journal=Pediatrics |volume=109 |issue=3 |pages=E45 |date=March 2002 |pmid=11875173 |doi= |url=}}</ref><ref name="pmid21680213">{{cite journal |vauthors=Sachdeva R, Schoenfield L, Marcotty A, Singh AD |title=Retinoblastoma with autoinfarction presenting as orbital cellulitis |journal=J AAPOS |volume=15 |issue=3 |pages=302–4 |date=June 2011 |pmid=21680213 |doi=10.1016/j.jaapos.2011.02.013 |url=}}</ref><ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref><ref name="pmid5897773">{{cite journal |vauthors=Howard GM, Ellsworth RM |title=Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma |journal=Am. J. Ophthalmol. |volume=60 |issue=4 |pages=610–8 |date=October 1965 |pmid=5897773 |doi= |url=}}</ref><br> | Coats’ disease must be differentiated from [[retinoblastoma]], [[Norrie disease]], and [[Retinopathy of prematurity]] ([[Retinopathy of prematurity|ROP]]).<ref name="pmid11875173">{{cite journal |vauthors=Butros LJ, Abramson DH, Dunkel IJ |title=Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences |journal=Pediatrics |volume=109 |issue=3 |pages=E45 |date=March 2002 |pmid=11875173 |doi= |url=}}</ref><ref name="pmid21680213">{{cite journal |vauthors=Sachdeva R, Schoenfield L, Marcotty A, Singh AD |title=Retinoblastoma with autoinfarction presenting as orbital cellulitis |journal=J AAPOS |volume=15 |issue=3 |pages=302–4 |date=June 2011 |pmid=21680213 |doi=10.1016/j.jaapos.2011.02.013 |url=}}</ref><ref name="SinghMurphree2015">{{cite book | last = Singh | first = Arun | title = Clinical ophthalmic oncology : retinoblastoma | publisher = Springer | location = Heidelberg | year = 2015 | isbn = 978-3-662-43451-2 }}</ref><ref name="pmid5897773">{{cite journal |vauthors=Howard GM, Ellsworth RM |title=Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma |journal=Am. J. Ophthalmol. |volume=60 |issue=4 |pages=610–8 |date=October 1965 |pmid=5897773 |doi= |url=}}</ref><br> | ||
For more information on [[differential diagnosis]] of Coats’ disease please [[Retinoblastoma differential diagnosis|click here]] | For more information on [[differential diagnosis]] of Coats’ disease please [[Retinoblastoma differential diagnosis|click here]] | ||
{| class="wikitable" | {| class="wikitable" | ||
![[Image:Coats-disease-of-the-eye.jpg|center|300px|thumb|MRI of the orbit showing Coats disease - Case courtesy of Dr Michael Sargent, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/6089]] | ![[Image:Coats-disease-of-the-eye.jpg|center|300px|thumb|MRI of the orbit showing Coats disease - Case courtesy of Dr Michael Sargent, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/6089]] | ||
Latest revision as of 16:34, 9 May 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Coats’ disease, (also known as exudative retinitis or retinal telangiectasis, sometimes spelled Coates' disease), is a rare eye disorder, causing full or partial blindness, characterized by abnormal development of blood vessels behind the retina. Coats’ usually affects only one eye (unilateral) and occurs predominantly in young males, with the onset of symptoms generally appearing in the first decade of life. The specific cause of Coats’ disease remains unknown. Current research suggests a genetic component contributes to the disease. It is believed one is born with this disease, but Coats’ is not hereditary.
Coats’ disease results in a gradual loss of vision. Blood leaks from the abnormal vessels into the back of the eye, leaving behind cholesterol deposits and damaging the retina. Coats’ normally progresses slowly. At advanced stages, retinal detachment is likely to occur. Glaucoma, atrophy, and cataracts can also develop secondary to Coats’ disease. In some cases, removal of the eye may be necessary (enucleation).
Symptoms
Symptoms begin as blurred vision, usually pronounced when one eye is closed (due to the unilateral nature of the disease). Often the unaffected eye will compensate for the loss of vision in the other eye; however, this results in some loss of depth perception and parallax. Deterioration of sight may begin in either the central or peripheral vision. Deterioration is likely to begin in the upper part of the vision field as this corresponds with the bottom of the eye where blood usually pools. Flashes of light, known as photopsia, and floaters are common symptoms. Persistent color patterns may also be perceived in the affected eye. Initially, these may be mistaken for psychological hallucinations, but are actually the result of both retinal detachment and foreign fluids mechanically interacting with the photoreceptors located on the retina.
One early warning sign of Coats’ disease is yellow-eye in flash photography. Just as the red-eye effect is caused by a reflection off blood vessels in the back of a normal eye, an eye affected by Coats’ will glow yellow in photographs as light reflects off cholesterol deposits. Children with yellow-eye in photographs are typically advised to immediately seek evaluation from an ophthalmologist.
Coats’ disease itself is not painful. Pain may develop as a result of retinal detachment. Pain may also occur if fluid is not able to properly drain from the eye, causing the internal pressure to swell.
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
|
| |
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
Coats’ disease must be differentiated from retinoblastoma, Norrie disease, and Retinopathy of prematurity (ROP).[5][6][7][8]
For more information on differential diagnosis of Coats’ disease please click here
 |
 |
 |
 |
|---|
Treatment
In the early stages, there are a few treatment options. Laser surgery or cryotherapy (freezing) can be used to destroy the abnormal blood vessels, thus halting progression of the disease. However, if the leaking blood vessels are clustered around the optic nerve, this treatment is not recommended as accidental damage to the nerve itself can result in permanent blindness. Coats’ disease may stop progressing all on its own, either temporarily or permanently. Cases have been documented in which the condition even reverses itself. However, once total retinal detachment occurs, sight loss is permanent in most cases. Removal of the eye (enucleation) is an option if pain or further complications arise.
External links
- http://www.orpha.net/data/patho/GB/uk-Coats.pdf
- http://www.coatsdisease.org/
- http://www.coatsdisease.net/
- http://www.revoptom.com/handbook/41.htm
- Personal story of Coates Disease
- ↑ 1.0 1.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 2.0 2.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 3.0 3.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 4.0 4.1 "c.ymcdn.com".
- ↑ Butros LJ, Abramson DH, Dunkel IJ (March 2002). "Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences". Pediatrics. 109 (3): E45. PMID 11875173.
- ↑ Sachdeva R, Schoenfield L, Marcotty A, Singh AD (June 2011). "Retinoblastoma with autoinfarction presenting as orbital cellulitis". J AAPOS. 15 (3): 302–4. doi:10.1016/j.jaapos.2011.02.013. PMID 21680213.
- ↑ Singh, Arun (2015). Clinical ophthalmic oncology : retinoblastoma. Heidelberg: Springer. ISBN 978-3-662-43451-2.
- ↑ Howard GM, Ellsworth RM (October 1965). "Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma". Am. J. Ophthalmol. 60 (4): 610–8. PMID 5897773.