Bradycardia electrocardiogram: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 6: | Line 6: | ||
An [[ECG]] may be helpful in the diagnosis of [[bradycardia]]. An upright [[P wave]] in leads I, II, and aVL, and a negative [[P wave]] in lead [[aVR]], indicates a sinus origin of the [[bradycardia]]. It is vital to exclude other causes of [[Bradyarrhythmia|bradyarrhythmia's]] such as [[AV block]]. | An [[ECG]] may be helpful in the diagnosis of [[bradycardia]]. An upright [[P wave]] in leads I, II, and aVL, and a negative [[P wave]] in lead [[aVR]], indicates a sinus origin of the [[bradycardia]]. It is vital to exclude other causes of [[Bradyarrhythmia|bradyarrhythmia's]] such as [[AV block]]. | ||
== 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay<ref name="pmid30586772">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. | journal=Circulation | year= 2019 | volume= 140 | issue= 8 | pages= e382-e482 | pmid=30586772 | doi=10.1161/CIR.0000000000000628 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30586772 }}</ref> == | |||
=== Recommendation for Electrocardiogram (ECG) in Patients With Documented or Suspected Bradycardia or Conduction Disorders === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.'''In patients with suspected bradycardia or conduction disorder, a 12-lead ECG is recommended to document rhythm, rate, and conduction, and to screen for structural heart disease or systemic illness. ''(Level of Evidence: B-NR)'' | |||
|} | |||
=== Recommendations for Exercise Electrocardiographic Testing in Patients With Documented or Suspected Bradycardia or Conduction Disorders === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon" | [[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
| bgcolor="LemonChiffon" |'''1.'''In patients with suspected chronotropic incompetence, exercise electrocardiographic testing is reasonable to ascertain the diagnosis and provide information on prognosis. ''(Level of Evidence: B-NR)'' | |||
|- | |||
| bgcolor="LemonChiffon" |'''2.''' In patients with exercise-related symptoms suspicious for bradycardia or conduction disorders, or in patients with 2:1 atrioventricular block of unknown level, exercise electrocardiographic testing is reasonable ''(Level of Evidence: C-LD)'' | |||
|} | |||
=== Recommendation for Ambulatory Electrocardiography in Patients With Documented or Suspected Bradycardia or Conduction Disorders === | |||
{| class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen" |[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen" |'''1.'''In the evaluation of patients with documented or suspected bradycardia or conduction disorders, cardiac rhythm monitoring is useful to establish correlation between heart rate or conduction abnormalities with symptoms, with the specific type of cardiac monitor chosen based on the frequency and nature of symptoms, as well as patient preferences. ''(Level of Evidence: B-NR)'' | |||
|} | |||
==Electrocardiogram== | ==Electrocardiogram== | ||
===Resting EKG=== | ===Resting EKG=== | ||
Latest revision as of 01:10, 28 December 2022
|
Bradycardia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bradycardia electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Bradycardia electrocardiogram |
|
Risk calculators and risk factors for Bradycardia electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: M.Umer Tariq [2] Ibtisam Ashraf, M.B.B.S.[3]
Overview
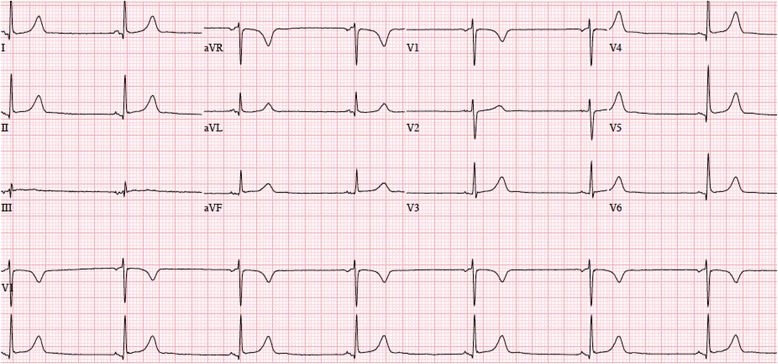
An ECG may be helpful in the diagnosis of bradycardia. An upright P wave in leads I, II, and aVL, and a negative P wave in lead aVR, indicates a sinus origin of the bradycardia. It is vital to exclude other causes of bradyarrhythmia's such as AV block.
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay[1]
Recommendation for Electrocardiogram (ECG) in Patients With Documented or Suspected Bradycardia or Conduction Disorders
| Class I |
| 1.In patients with suspected bradycardia or conduction disorder, a 12-lead ECG is recommended to document rhythm, rate, and conduction, and to screen for structural heart disease or systemic illness. (Level of Evidence: B-NR) |
Recommendations for Exercise Electrocardiographic Testing in Patients With Documented or Suspected Bradycardia or Conduction Disorders
| Class IIa |
| 1.In patients with suspected chronotropic incompetence, exercise electrocardiographic testing is reasonable to ascertain the diagnosis and provide information on prognosis. (Level of Evidence: B-NR) |
| 2. In patients with exercise-related symptoms suspicious for bradycardia or conduction disorders, or in patients with 2:1 atrioventricular block of unknown level, exercise electrocardiographic testing is reasonable (Level of Evidence: C-LD) |
Recommendation for Ambulatory Electrocardiography in Patients With Documented or Suspected Bradycardia or Conduction Disorders
| Class I |
| 1.In the evaluation of patients with documented or suspected bradycardia or conduction disorders, cardiac rhythm monitoring is useful to establish correlation between heart rate or conduction abnormalities with symptoms, with the specific type of cardiac monitor chosen based on the frequency and nature of symptoms, as well as patient preferences. (Level of Evidence: B-NR) |
Electrocardiogram
Resting EKG
- An ECG may be helpful in the diagnosis of bradycardia. Findings on an ECG diagnostic of bradycardia include:
- The heart rate is < 60 beats per minute.
- An upright P wave in leads I, II, and aVL.
- A negative P wave in lead aVR, indicates a sinus origin of the bradycardia.[2]
24 Hour Ambulatory Electrocardiogram Monitoring
- The diagnosis is usually made with the help of a 24-hour ambulatory electrocardiogram (ECG) or telemetry.
References
- ↑ Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 140 (8): e382–e482. doi:10.1161/CIR.0000000000000628. PMID 30586772.
- ↑ Kundu A, Fitzgibbons TP (2015). "Acute symptomatic sinus bradycardia in a woman treated with pulse dose steroids for multiple sclerosis: a case report". J Med Case Rep. 9: 216. doi:10.1186/s13256-015-0701-x. PMC 4581459. PMID 26400725.