Severe acute respiratory syndrome
| Severe acute respiratory syndrome | |
| ICD-10 | U04 |
|---|---|
| ICD-9 | 079.82 |
| DiseasesDB | 32835 |
| MedlinePlus | 007192 |
| MeSH | D045169 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: SARS; Coronavirus, SARS associated
Overview
Severe acute respiratory syndrome or SARS is a respiratory disease in humans which is caused by the SARS coronavirus.[1] There has been one major pandemic to date, between November 2002 and July 2003, with 8,096 known cases of the disease, and 774 deaths (a mortality rate of 9.6%) being listed in the WHO's April 21, 2004 concluding report.[2]
Outbreak in Mainland China
| Probable cases of SARS by country, 1 November 2002–31 July 2003. | |||
| Country or Region | Cases | Deaths | Fatality (%) |
| People's Republic of China * | 5327(Official claimed Data) | 349(Official claimed Data) | 6.6(Official claimed Data) |
| Hong Kong * | 1755 | 299 | 17 |
| Canada | 251 | 43 | 17 |
| Taiwan * | 346** | 37 | 11 |
| Singapore | 238 | 33 | 14 |
| Vietnam | 63 | 5 | 8 |
| USA | 27 | 0 | 0 |
| Philippines | 14 | 2 | 14 |
| Germany | 9 | 0 | 0 |
| Mongolia | 9 | 0 | 0 |
| Thailand | 9 | 2 | 22 |
| France | 7 | 1 | 14 |
| Malaysia | 5 | 2 | 40 |
| Sweden | 5 | 0 | 0 |
| Italy | 4 | 0 | 0 |
| UK | 4 | 0 | 0 |
| India | 3 | 0 | 0 |
| Republic of Korea | 3 | 0 | 0 |
| Indonesia | 2 | 0 | 0 |
| South Africa | 1 | 1 | 100 |
| Macau * | 1 | 0 | 0 |
| Kuwait | 1 | 0 | 0 |
| Republic of Ireland | 1 | 0 | 0 |
| Romania | 1 | 0 | 0 |
| Russian Federation | 1 | 0 | 0 |
| Spain | 1 | 0 | 0 |
| Switzerland | 1 | 0 | 0 |
| Total | 8096 | 774 | 9.6 |
| (*) Figures for the People's Republic of China (excluding the Special Administrative Regions), Macau SAR, Hong Kong SAR, and the Republic of China (Taiwan) were reported separately by the WHO. | |||
| (**) Since 11 July 2003, 325 Taiwanese cases have been 'discarded'. Laboratory information was insufficient or incomplete for 135 discarded cases; 101 of these patients died. | |||
| Source:WHO.[3] | |||
The epidemic of SARS appears to have originated in Guangdong Province, China in November 2002. The first case was reportedly originated from a rural area in Foshan, Guangdong in Nov 2002, and the patient, a farmer, was treated in the First People's Hospital of Foshan. The patient died soon after, and no definite diagnosis was made on his cause of death. ("Patient #0" -- first reported symptoms -- has been attributed to Charles Bybelezar of Montreal, Canada) and, despite taking some action to control it, Chinese government officials did not inform the World Health Organization of the outbreak until February 2003, restricting media coverage in order to preserve public confidence. This lack of openness caused delays in efforts to control the epidemic, resulting in criticism of the People’s Republic of China (PRC) from the international community. The PRC has since officially apologized for early slowness in dealing with the SARS epidemic.[4]
The first clue of the outbreak appears to be November 27, 2002 when Canada's Global Public Health Intelligence Network (GPHIN), an electronic warning system which is part of the World Health Organization's (WHO) Global Outbreak and Alert Response Network] (GOARN), picked up reports of a "flu outbreak" in China through internet media monitoring and analysis and sent them to the WHO.[5] [6] Subsequently, the WHO requested information from Chinese authorities on December 5 and 11.[6] Importantly, while GPHIN's capability had recently been upgraded to enable Arabic, Chinese, English, French, Russian and Spanish translation, the system was limited to English or French in presenting this information. Thus, while the first reports of an unusual outbreak were in Chinese, an English report was not generated until January 21, 2003.[5]
In early April, there appeared to be a change in official policy when SARS began to receive a much greater prominence in the official media. Some have directly attributed this to the death of American James Earl Salisbury.[7] However, it was also in early April that accusations emerged regarding the undercounting of cases in Beijing military hospitals. After intense pressure, PRC officials allowed international officials to investigate the situation there. This revealed problems plaguing the aging mainland Chinese healthcare system, including increasing decentralization, red tape, and inadequate communication.
In late April, revelations occurred as the PRC government admitted to underreporting the number of cases of SARS due to the problems inherent in the healthcare system. Dr. Jiang Yanyong exposed the coverup that was occurring in China, at great personal risk. He reported that there were more SARS patients in his hospital alone than were being reported in all of China. A number of PRC officials were fired from their posts, including the health minister and mayor of Beijing, and systems were set up to improve reporting and control in the SARS crisis. Since then, the PRC has taken a much more active and transparent role in combating the SARS epidemic.
Spread to other countries
The epidemic reached the public spotlight in February 2003, when an American businessman traveling from China became afflicted with pneumonia-like symptoms while on a flight to Singapore. The plane stopped at Hanoi, Vietnam, where the victim died in the French Hospital of Hanoi. Several of the medical staff who treated him soon developed the same disease despite basic hospital procedures. Italian doctor Carlo Urbani identified the threat and communicated it to WHO and the Vietnam government. The severity of the symptoms and the infection of hospital staff alarmed global health authorities fearful of another emergent pneumonia epidemic. On March 12, 2003, the WHO issued a global alert, followed by a health alert by the United States Centers for Disease Control and Prevention (CDC). Local transmission of SARS took place in Toronto, Vancouver, San Francisco, Ulan Bator, Manila, Singapore, Hanoi, Republic of China, Taiwan, the Chinese provinces of Guangdong, Jilin, Hebei, Hubei, Shaanxi, Jiangsu and Shanxi, the Direct-controlled municipality of Tianjin, the Chinese Autonomous Region of Inner Mongolia, and the Chinese Special Administrative Region of Hong Kong.
In Hong Kong the first cohort of affected people were discharged from the hospital on March 29 2003. The disease spread in Hong Kong from a mainland doctor on the 9th floor of the Metropole Hotel in Kowloon Peninsula, infecting 16 of the hotel visitors. Those visitors traveled to Singapore and Toronto, spreading SARS to those locations. Another, larger, cluster of cases in Hong Kong centred on the Amoy Gardens housing estate. Its spread is suspected to have been facilitated by defects in the sewage system of the estate.
Clinical information
Symptoms
Initial symptoms are flu like and may include: fever, myalgia, lethargy, gastrointestinal symptoms, cough, sore throat and other non-specific symptoms. The only symptom that is common to all patients appears to be a fever above 38 °C (100.4 °F). Shortness of breath may occur later. Symptoms usually appear 2–10 days following exposure, but up to 13 days has been reported. In most cases symptoms appear within 2–3 days. About 10–20% of cases require mechanical ventilation.
Investigations
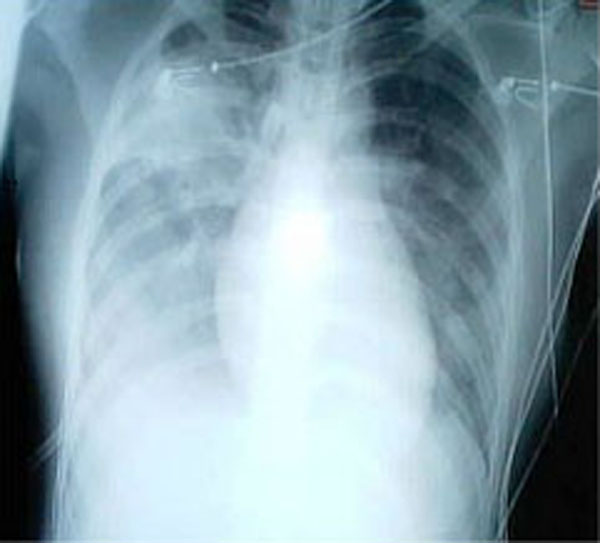
The Chest X-ray (CXR) appearance of SARS is variable. There is no pathognomonic appearance of SARS but is commonly felt to be abnormal with patchy infiltrates in any part of the lungs. The initial CXR may be clear.
White blood cell and platelet counts are often low. Early reports indicated a tendency to relative neutrophilia and a relative lymphopenia — relative because the total number of white blood cells tends to be low. Other suggestive laboratory tests are raised lactate dehydrogenase and slightly raised creatine kinase and C-Reactive protein levels.
Diagnostic tests
With the identification and sequencing of the RNA of the coronavirus responsible for SARS on April 12, 2003, several diagnostic test kits have been produced and are now being tested for their suitability for use.
Three possible diagnostic tests have emerged, each with drawbacks. The first, an ELISA (enzyme-linked immunosorbent assay) test detects antibodies to SARS reliably but only 21 days after the onset of symptoms. The second, an immunofluorescence assay, can detect antibodies 10 days after the onset of the disease but is a labour and time intensive test, requiring an immunofluorescence microscope and an experienced operator. The last test is a PCR (polymerase chain reaction) test that can detect genetic material of the SARS virus in specimens ranging from blood, sputum, tissue samples and stools. The PCR tests so far have proven to be very specific but not very sensitive. This means that while a positive PCR test result is strongly indicative that the patient is infected with SARS, a negative test result does not mean that the patient does not have SARS.
The WHO has issued guidelines for using these diagnostic tests.[3]
There is currently no rapid screening test for SARS and research is ongoing.
Diagnosis
SARS may be suspected in a patient who has:
- Any of the symptoms including a fever of 38 °C (100.4 °F) or more AND
- Either a history of
- Contact (sexual or casual) with someone with a diagnosis of SARS within the last 10 days OR
- Travel to any of the regions identified by the WHO as areas with recent local transmission of SARS (affected regions as of 10 May 2003[3] were parts of China, Hong Kong, Singapore and the province of Ontario, Canada).
A probable case of SARS has the above findings plus positive chest x-ray findings of atypical pneumonia or adult respiratory distress syndrome.
With the advent of diagnostic tests for the coronavirus probably responsible for SARS, the WHO has added the category of "laboratory confirmed SARS" for patients who would otherwise fit the above "probable" category who do not (yet) have the chest x-ray changes but do have positive laboratory diagnosis of SARS based on one of the approved tests (ELISA, immunofluorescence or PCR).
Mortality rate
The mortality rates vary across countries and reporting organizations. In early May, for consistency with similar metrics of other diseases, the World Health Organization (WHO) and U.S. Centers for Disease Control and Prevention were quoting 7%, or the number of deaths divided by probable cases, as the SARS mortality rate. Others spoke in favour of a 15% figure, derived from number of deaths divided by the number who recovered, saying it reflects the real situation more accurately. As the outbreak progressed both mortality measures approached 10%.
One reason for the difficulties in plotting a reliable mortality figure is that the number of infections and the number of deaths are increasing at different rates. A possible explanation involves a secondary infection as a causal agent in the disease [8], but whatever the cause, the mortality numbers are bound to change.
Mortality by age group as of 8 May 2003 is below 1% for people aged 24 or younger, 6% for those 25 to 44, 15% in those 45 to 64 and more than 50% for those over 65.[9]
For comparison, the case fatality rate for influenza is usually about 0.6% (primarily among the elderly) but can rise as high as 33% in locally severe epidemics of new strains. The mortality rate of the primary viral pneumonia form is about 70%.
Treatment
Antibiotics are ineffective. Treatment of SARS so far has been largely supportive with antipyretics, supplemental oxygen and ventilatory support as needed.
Suspected cases of SARS must be isolated, preferably in negative pressure rooms, with full barrier nursing precautions taken for any necessary contact with these patients.
There was initially anecdotal support for steroids and the antiviral drug ribavirin, but no published evidence has supported this therapy. Many clinicians now suspect that ribavirin is detrimental.
Researchers are currently testing all known antiviral treatments for other diseases including AIDS, hepatitis, influenza and others on the SARS-causing coronavirus.
There is some evidence that some of the more serious damage in SARS is due to the body's own immune system overreacting to the virus. There may be some benefit from using steroids and other immune modulating agents in the treatment of the more acute SARS patients. Research is continuing in this area.
In December 2004 it was reported that Chinese researchers had produced a SARS vaccine. It has been tested on a group of 36 volunteers, 24 of whom developed antibodies against the virus. [10]
A 2006 systematic review of all the studies done on the 2003 SARS epidemic found no evidence that antivirals, steroids or other therapies helped patients. A few suggested they caused harm.[11]
Antiviral Research
Before the emergence of SARS-CoV, no efforts were put into the search for antivirals against coronaviruses. The rapid transmission and high mortality rate made SARS a global threat for which no efficacious therapy was available and empirical strategies had to be used to treat the patients. New insights into the field of the SARS-CoV genome structure and pathogenesis revealed novel potential anti-coronavirus targets. Several proteins encoded by the SARS-CoV could be considered as targets for therapeutic intervention: the spike protein, the main protease, the NTPase/helicase, the RNA dependent RNA polymerase and different other viral protein-mediated processes. Potential anti-SARS-CoV drugs are currently being developed in vivo. The development of effective drugs against SARS-CoV may also provide new strategies for the prevention or treatment of other coronavirus diseases in animals or humans.[1]
Vaccine Development
The emergence and identification of several common and rare human coronaviruses that cause severe lower respiratory tract infection argues for the judicious development of robust coronavirus vaccines and vector platforms. Currently, limited information is available on the correlates of protection against SARS-CoV and other severe lower respiratory tract human coronavirus infections, a clear priority for future research. Passive immunization has been successful in establishing protection from SARS-CoV suggesting an important role for neutralizing antibodies. One important property of future vaccine candidates is the ability to confer protection against multiple variant strains of SARS-CoV, especially in senescent populations that are most at risk for severe disease. Many vaccine candidates are capable of inducing humoral and cellular responses. The development of infectious clones for coronaviruses has facilitated the identification of attenuating mutations, deletions and recombinations which could ultimately result in live attenuated vaccine candidates. Stable vaccine platforms should be developed that allow for rapid intervention strategies against any future emergence coronaviruses. Vaccine correlates that enhance disease after challenge should be thoroughly investigated and mechanisms devised to circumvent vaccine-associated complications.[1]
Coronaviruses are positive-strand, enveloped RNA viruses that are important pathogens of mammals and birds. This group of viruses cause enteric or respiratory tract infections in a variety of animals including humans, livestock and pets.[1]
Initial electron microscopic examination in Hong Kong and Germany found viral particles with structures suggesting paramyxovirus in respiratory secretions of SARS patients. Subsequently, in Canada, electron microscopic examination found viral particles with structures suggestive of metapneumovirus (a subtype of paramyxovirus) in respiratory secretions. Chinese researchers also reported that a chlamydia-like disease may be behind SARS. The Pasteur Institute in Paris identified coronavirus in samples taken from six patients, so did the laboratory of Malik Peiris at the University of Hong Kong, which in fact was the first to announce (on March 21, 2003) the discovery of a new coronavirus as the possible cause of SARS after successfully cultivating it from tissue samples and was also amongst the first to develop a test for the presence of the virus. The CDC noted viral particles in affected tissue (finding a virus in tissue rather than secretions suggests that it is actually pathogenic rather than an incidental finding). Upon electron microscopy, these tissue viral inclusions resembled coronaviruses, and comparison of viral genetic material obtained by PCR with existing genetic libraries suggested that the virus was a previously unrecognized coronavirus. Sequencing of the virus genome — which computers at the British Columbia Cancer Agency in Vancouver completed at 4 a.m. Saturday, April 12, 2003 — was the first step toward developing a diagnostic test for the virus, and possibly a vaccine.[12] A test was developed for antibodies to the virus, and it was found that patients did indeed develop such antibodies over the course of the disease, which is highly suggestive of a causative role.
On April 16, 2003, the WHO issued a press release stating that a coronavirus identified by a number of laboratories was the official cause of SARS.[13] Scientists at Erasmus University in Rotterdam, the Netherlands demonstrated that the SARS coronavirus fulfilled Koch's postulates thereby confirming it as the causative agent. In the experiments, macaques infected with the virus developed the same symptoms as human SARS victims.[14]
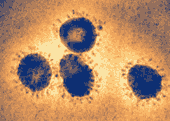
An article published in The Lancet identifies a coronavirus as the probable causative agent.
In late May 2003, studies from samples of wild animals sold as food in the local market in Guangdong, China found that the SARS coronavirus could be isolated from civets. This suggests that the SARS virus crossed the xenographic barrier from civets. In 2005, two studies identified a number of SARS-like coronaviruses in Chinese bats.[15][16] Phylogenetic analysis of these viruses indicated a high probability that SARS coronavirus originated in bats and spread to humans either directly, or through civet cats. The bats did not show any visible signs of disease.
Viral Replication
Coronavirus (CoV) genome replication takes place in the cytoplasm in a membrane-protected microenvironment and starts with the translation of the genome to produce the viral replicase. CoV transcription involves a discontinuous RNA synthesis (template switch) during the extension of a negative copy of the subgenomic mRNAs. The requirement for basepairing during transcription has been formally demonstrated in arteriviruses and CoVs. CoV N protein is required for coronavirus RNA synthesis and has RNA chaperone activity that may be involved in template switch. Both viral and cellular proteins are required for replication and transcription. CoVs initiate translation by cap-dependent and cap-independent mechanisms. Cell macromolecular synthesis may be controlled after CoV infection by locating some virus proteins in the host cell nucleus. Infection by different coronaviruses cause in the host alteration in the transcription and translation patterns, in the cell cycle, the cytoskeleton, apoptosis and coagulation pathways, inflammation and immune and stress responses. The balance between genes up- and down-regulated could explain the pathogenesis caused by these viruses. Coronavirus expression systems based on single genome constructed by targeted recombination, or by using infectious cDNAs, have been developed. The possibility of expressing different genes under the control of transcription regulating sequences (TRSs) with programmable strength and engineering tissue and species tropism indicates that CoV vectors are flexible. CoV based vectors have emerged with high potential vaccine development and possibly for gene therapy.[17]
Action implemented to restrict the outbreak of SARS
WHO set up a network for doctors and researchers dealing with SARS, consisting of a secure web site to study chest x-rays and a teleconference.

Attempts were made to control further SARS infection through the use of quarantine. Over 1200 were under quarantine in Hong Kong, while in Singapore and Taiwan, 977 and 1147 were quarantined respectively. Canada also put thousands of people under quarantine.[18] In Singapore, schools were closed for 10 days and in Hong Kong they were closed until 21 April to contain the spread of SARS.[19]
On March 27, 2003, the WHO recommended the screening of airline passengers for the symptoms of SARS.[20]
In Singapore, a single hospital, Tan Tock Seng Hospital, was designated as the sole treatment and isolation centre for all confirmed and probable cases of the disease on 22 March. Subsequently, all hospitals implemented measures whereby all staff members were required to submit to temperature checks twice a day, visitorship was restricted only to pediatric, obstetric and selected other patients, and even then, only one person may visit at a time. To overcome this inconvenience, videoconferencing was utilised. A dedicated phoneline was designated to report SARS cases, whereupon a private ambulance service was dispatched to transport them to Tan Tock Seng Hospital.
On 24 March, Singapore's Ministry of Health invoked the Infectious Diseases Act, allowing for a 10-day mandatory home quarantine to be imposed on all who may have come in contact with SARS patients. SARS patients who have been discharged from hospitals are under 21 days of home quarantine, with telephone surveillance requiring them to answer the phone when randomly called up. Discharged probable SARS patients and some recovered cases of suspected SARS patients are similarly required to be home quarantined for 14 days. Security officers from Commercial and Industrial Security Corporation (CISCO), a Singaporean security company, were utilised to serve quarantine orders to their homes, and installed an electronic picture (ePIC) camera outside the doors of each contact.

Sparked in particular by the publicity of an elderly gentleman who disregarded the quarantine order, flashing it to the public as he strolled to eating outlets and causing a minor exodus of patrons which persisted until the fears over the disease abated, the Singapore government called for an urgent meeting in Parliament on 24 April to amend the Infectious Disease Act and include penalties for violations, revealing at least 11 other violators of their quarantine orders. These amendments include
- the requirement of suspected persons of infectious diseases to be brought to designated treatment centres, and the prohibition of them from going to public places,
- the designation of contaminated areas and the restriction of access to them, and the destruction of suspected sources of infection,
- to introduce the possibility of affixing offenders who break home quarantine with electronic wrist tags (persons who fail to be contacted three times by phone consecutively will be slapped with the tag), and the imposition of fines without court trial,
- the capability to charge repeated offenders in court which may lead to imprisonment,
- and the prosecution of anyone caught lying to health officials about their travel to SARS-affected areas or contacts with SARS patients.
On 23 April the WHO advised against all but essential travel to Toronto, noting that a small number of persons from Toronto appear to have "exported" SARS to other parts of the world. Toronto public health officials noted that only one of the supposedly exported cases had been diagnosed as SARS and that new SARS cases in Toronto were originating only in hospitals. Nevertheless, the WHO advisory was immediately followed by similar advisories by several governments to their citizens. On 29 April WHO announced that the advisory would be withdrawn on 30 April. Toronto tourism suffered as a result of the WHO advisory, prompting The Rolling Stones and others to organize the massive Molson Canadian Rocks for Toronto concert, commonly known as SARSstock, to revitalize the city's tourism trade.
Also on 23 April, Singapore instituted thermal imaging scans to screen all passengers departing Singapore from Singapore Changi Airport. It also stepped up screening of travelers at its Woodlands and Tuas checkpoints with Malaysia. Singapore had previously implemented this screening method for incoming passengers from other SARS affected areas but will move to include all travelers into and out of Singapore by mid to late May.
In addition, students and teachers in Singapore were issued with free personal oral digital thermometers. Students took their temperatures daily; usually two or three times a day, but the temperature-taking exercises were suspended with the waning of the outbreak.


Taiwan Taoyuan International Airport (Chiang Kai-shek international Airport) also added SARS checkpoints with an infrared screening system similar to Singapore's Changi Airport.

Political, artistic and economic reaction
Canada
Most conferences and conventions scheduled for Toronto were cancelled, and the production of at least one movie was moved out of the city. On 22 April the Canadian Broadcasting Corporation reported that the hotel occupancy rate in Toronto was only half the normal rate, and that tour operators were reporting large declines in business. As of 22 April all Canadian SARS cases were believed to be directly or indirectly traceable to the originally identified carriers. SARS was not loose in the community at large in Canada, although a few infected persons had broken quarantine and moved among the general population. No new cases had originated outside hospitals for 20 days.
Nonetheless, on 23 April the WHO extended its travel advice urging postponement of non-essential travel to include Toronto. At the time, city officials and business leaders in the city expected a large economic impact as a result, and an official of the Bank of Canada said that the travel ban would drastically affect Canada's national economy.
On 29 April, WHO announced that its advisory against unnecessary travel to Toronto would be withdrawn on 30 April.
The U.S. Library of Congress officially excused itself from attending the American Library Association convention in Toronto in summer 2003 as a precaution.
In 2005 and 2006 The Rumoli Brothers [21] (a comedy duo based out of Toronto) put on SARSical; a musical that explored the lighter side of the epidemic and poked fun at the media's over-reaction to the 43 deaths that occurred in Toronto. [22]
The Chinese world
Severe customer drop of Chinese cuisine restaurants in Guangdong, Hong Kong and Chinatowns in North America, 90% decrease in some cases. Business recovered considerably in some cities after the end of the outbreak.
Hong Kong
Some members of Hong Kong Legislative Council recommended editing the budget for increased spending on medical services.
Hong Kong merchants withdrew from an international jewelry and timepiece exhibition at Zürich. Consulate Genera] officials enforced a full body check of the 1000 Hong Kong participants that would be finished 2 days before the end of the exhibition. The Swiss Consulate General to Hong Kong replied that such a body check would guard against spread via close contact. A merchant union leader alleged probable racial discrimination towards Chinese merchants, as the exhibition committee allowed the merchants to participate in the exhibition but not to promote their own goods. An estimated several hundred million Hong Kong dollars in contracts were lost as a result. However, exhibitors from Hong Kong were not barred from selling their products in their hotel rooms.
In June, Hong Kong launched the Individual Visit Scheme as a way to boost its economy.
China
The 2003 FIFA Women's World Cup, originally scheduled for China, was moved to the United States. On March 30, the International Ice Hockey Federation (IIHF) cancelled the 2003 IIHF Women's World Championship tournament which was to take place in Beijing.
In the People's Republic of China, the latter stage of the SARS crisis showed an unprecedented change in the central government's policies. In the past, rarely had officials stepped down purely because of administrative mistakes, but the case was different with SARS, when these mistakes caused international scrutiny. This change in policy has been largely credited to President Hu Jintao and Premier Wen Jiabao. At the heart of the crisis, Hu made a high-profile trip to Guangdong and Wen ate lunch with students at Peking University. Some analysts believe the crisis was a blow to former CPC chief Jiang Zemin, who stayed out of the national spotlight during its duration, and whose political allies, such as Health Minister Zhang Wenkang, were fired for irresponsibility and wrongdoings during the SARS crisis. Zhang was replaced by Wu Yi.
Mainland China and Taiwan
Both Mainland China and Republic of China/Taiwan were dealing with SARS epidemics at the same time, and the political status of Taiwan (cross-strait politics) inevitably complicated the way the disease was handled. Since the People's Republic of China insisted on representing the 23 million Taiwanese people in the WHO by itself and forbid the ROC government's participation, Taiwan, which was one of the most endemic areas in the world, did not receive direct advice from WHO. Even though the ROC government actively reported the situation to WHO, the authority received SARS information only through the WHO website.
The ROC claimed that the lack of direct communication with the WHO precluded proper handling of the disease and caused unnecessary deaths on the island. On the other hand, the PRC claimed that video conferences held between her experts and Taiwanese experts already facilitated information distribution and improved the way SARS was being treated in Taiwan; the ROC government denied this.
The ROC further advocated its own seats in WHO and used the case of SARS to illustrate the importance of having Taiwan included in the global health monitoring system. However, the PRC saw this as a politically motivated move towards Taiwanese independence. During the WHO general assembly, the People's Republic of China fiercely snubbed the proposal for Taiwan's participation. This was evidenced by one famous video clip aired widely in Taiwan showing the PRC Vice Premier Wu Yi and her official company rebuffing the question of Taiwan's representation which had been raised by Taiwanese reporters. Under pressure from the PRC, Taiwan was excluded from several major SARS conferences held by WHO. WHO eventually sent its experts to Taiwan to conduct inspections at the end of the SARS endemic; however, the PRC claimed the credit.
United States: Epidemic of Fear
SARS illustrated that responses to a deadly epidemic can occur far beyond the region experiencing actual infections, particularly in the age of the Internet. In the United States, only eight people had laboratory evidence of SARS infection, and most of these people contracted the virus abroad (CDC 2004). However, mainstream media reports fixated on the possibility of a domestic epidemic, and often used metaphors that described SARS as the product of Chinese “culture” [23]. The ubiquitous media image of Asians in facemasks and emails circulating rumors of domestic infections in Chinatowns across the country helped to establish the association between Asian peoples and SARS infection.
A national survey conducted by the Harvard School of Public Health revealed that by mid-April, 93% of Americans had heard of SARS. Further, the survey showed that fourteen percent of Americans nationally avoided Asian businesses [24]. While the latter is not an overwhelming statistic, many Asian communities began reporting losses in business and tourism, indicating that a larger percentage of people in areas near Asian communities might have avoided Asian businesses.
New York City’s Chinatown was particularly hard hit, as rumors of local infections circulated fear around the community and many Asian Americans felt stigmatized in the general public. Even without a local epidemic, SARS caused economic damage to Chinatown’s economy that was already struggling from the nearby terrorist attacks of 9/11. Tourism plummeted as the public avoided what they perceived as an infected space and people. Restaurants in particular suffered losses after one particular rumor reported that a local restaurant owner had spread SARS to his employees before dying. According to local accounts, tourism and business were still lagging in the summer of 2004, one year after SARS had been contained [25]. Even without a single infection, Chinatown was quickly identified as a site of contagion and risk. Chinatown community members responded by organizing demonstrations to refute rumors of local infections. The Organization of Chinese Americans sponsored a rally in support of local businesses, with leaders bearing the banner “SARS: Support Asian RestaurantS.” Senators Hillary Clinton and Charles Schumer publicly dined in Chinatown restaurants, surrounded by reporters who publicized the events.
However, Chinatown community members did not universally dismiss the dominant discourses of risk and responsibility that blamed SARS on Chinese “culture”. In fact, local responses to these discourses revealed many fissures within the Chinatown community. Although individuals criticized the conflation of SARS infection with discrimination against Chinese- and Asian Americans in general, many used the same dominant discourses of risk and blame to voice concerns about sanitation, public health, and undocumented immigrants in Chinatown [26].
Laboratory mishandling
Improper handling of the live SARS virus caused the infection of two researchers in Singapore and one in Taiwan. The discovery of the infection of the Taiwanese researcher, who was visiting Singapore before he was diagnosed as infected, caused Singapore and Taiwan to quarantine 92 people.
References
- ↑ 1.0 1.1 1.2 1.3 Thiel V (editor). (2007). Coronaviruses: Molecular and Cellular Biology (1st ed. ed.). Caister Academic Press. ISBN 978-1-904455-16-5 .
- ↑ http://www.who.int/csr/sars/country/table2004_04_21/en/index.html
- ↑ 3.0 3.1 3.2 Epidemic and Pandemic Alert and Response (EPR), World Health Organization (WHO)
- ↑ WHO targets SARS 'super spreaders', CNN News, 6 April 2003. URL Accessed 5 July 2006.
- ↑ 5.0 5.1 Mawudeku, A. and Blench, M. "Global Public Health Intelligence Network," mt-archive, 2005
- ↑ 6.0 6.1 Heymann, D. L., and Rodier, G. "Global Surveillance, National Surveillance, and SARS," Emerging Infectios Diseases - Medscape, February 10, 2004
- ↑ CNN - SARS death leads to China dispute, CNN News, 10 April 2003. URL Accessed 3 April 2007.
- ↑ Eric Lerner's analysis, May 6 2003. URL Accessed July 6, 2006
- ↑ Update 49 - SARS case fatality ratio, incubation period, World Health Organization, 7 May 2003. URL Accessed 5 July 2006.
- ↑ First SARS vaccine trials a success China Daily January 15, 2005
- ↑ SARS: Systematic Review of Treatment Effects PLoS Medicine September 2006 URL Accessed 13 September 2006
- ↑ Marra, MA, Jones, SJ, Astell, CR et al (2003) The genome sequence of the SARS-associated coronavirus. Science 300(5624):1377–1378
- ↑ Coronavirus never before seen in humans is the cause of SARS, New York: United Nations World Health Organization, 16 April 2006. URL Accessed 5 July 2006.
- ↑ Fouchier, RAM, Kuiken, T, Schutten, M et al (2003). Aetiology: Koch’s postulates fulfilled for SARS virus. Nature 423:240.
- ↑ Li, W, Shi, A, Yu, M et al (2005) Bats are natural reservoirs of SARS-like coronaviruses. Science 310(5748):676–679.
- ↑ Lau, SKP, Woo, PCY, Li, KSM et al. (2005). Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proceedings of the National Academy of Sciences 102(29):14040–14045.
- ↑ Enjuanes L; et al. (2008). "Coronavirus Replication and Interaction with Host". Animal Viruses: Molecular Biology. Caister Academic Press. ISBN 978-1-904455-22-6.
- ↑ Yahoo News story. URL Inactive 5 July 2006
- ↑ Joint Press Release by Ministry of Education and Ministry of Health - Closure of schools, Singapore Ministry Education and Ministry of Health, 26 March 2003. URL Accessed 5 July 2006.
- ↑ Update 11 - WHO recommends new measures to prevent travel-related spread of SARS, World Health Organization, 27 March 2003. URL Accessed 5 July 2006.
- ↑ http://www.harlettes.com/bios/Rumoli%20Brothers.htm
- ↑ http://www.nowtoronto.com/issues/2006-06-08/stage_comedyreviews.php
- ↑ Eichelberger, L. (2007) SARS and New York's Chinatown: The politics of risk and blame during an epidemic of fear. Social Science and Medicine 65(6):1284-95
- ↑ Blendon, Robert J., et al. (2003) Project on Biological Security and the Public, Harvard School of Public Health: SARS Survey. Boston: Harvard School of Public Health
- ↑ Eichelberger, L. (2007) SARS and New York's Chinatown: The politics of risk and blame during an epidemic of fear. Social Science and Medicine 65(6):1284-95
- ↑ Eichelberger, L. (2007) SARS and New York's Chinatown: The politics of risk and blame during an epidemic of fear. Social Science and Medicine 65(6):1284-95
External links
Mainstream news
- SARS in Singapore — Updated frequently by ChannelNewsAsia
- Fighting SARS Together — People's Republic of China Xinhua News Agency
- Yahoo! News search — SARS Full Coverage from leading worldwide news organizations
Official announcements
- Official SARS information from the World Health Organization
- Official SARS information from the United States Centers for Disease Control
- Official SARS information from Public Health Agency of Canada
- Official SARS information from the Singapore Ministry of Health and Ministry of Information and the Arts
- Following their experience with SARS, the Canadians have put together an excellent exposition of the ethical principles that apply in an epidemic or pandemic, and discussion of how the were/can be applied in practice. It's available here.
Medical mailing lists
- EMED-L mailing list — contains "breaking news" discussion of SARS
- CCM-L mailing list — contains "breaking news" discussion of SARS, notably including the dispatches of the intensive-care specialist Tom Buckley on his work on the ongoing Hong Kong outbreak of SARS
Other
- Video of the effect of SARS on the Hong Kong MTR (Subway System) — Video of the effect of SARS on the Hong Kong MTR (Subway System)
- SARS and its effects on Hong Kong - a short black and white photo-essay of SARS and its impact on the people of
- NIOSH Topic Area: Severe Acute Respiratory Syndrome (SARS)
- NIOSH Publication: Understanding Respiratory Protection Against SARS
- Focus on Coronaviruses: Focus on Coronaviruses
Template:Baltimore classification Template:Viral diseases