Waldenström's macroglobulinemia physical examination: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Waldenström's macroglobulinemia}} | {{Waldenström's macroglobulinemia}} | ||
{{CMG}}{{AE}}{{S.M.}}{{MGS}} | {{CMG}}; {{AE}} {{S.M.}}, {{MGS}}; {{GRR}} {{Nat}} | ||
==Overview== | ==Overview== | ||
Revision as of 18:28, 8 April 2019
|
Waldenström's macroglobulinemia Microchapters |
|
Differentiating Waldenström's macroglobulinemia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Waldenström's macroglobulinemia physical examination On the Web |
|
American Roentgen Ray Society Images of Waldenström's macroglobulinemia physical examination |
|
Waldenström's macroglobulinemia physical examination in the news |
|
Blogs on Waldenström's macroglobulinemia physical examination |
|
Directions to Hospitals Treating Waldenström's macroglobulinemia |
|
Risk calculators and risk factors for Waldenström's macroglobulinemia physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2], Mirdula Sharma, MBBS [3]; Grammar Reviewer: Natalie Harpenau, B.S.[4]
Overview
Patients with Waldenström macroglobulinemia usually appear oriented to time, place, and person. Physical examination of patients with Waldenström's macroglobulinemia is usually remarkable for various findings depending on the degree of tissue infiltration by malignant tumor cells, hyperviscosity syndrome, and accumulation of paraprotein.
Physical Examination
General Appearance
Patients with Waldenström macroglobulinemia are generally well-appearing.[1]
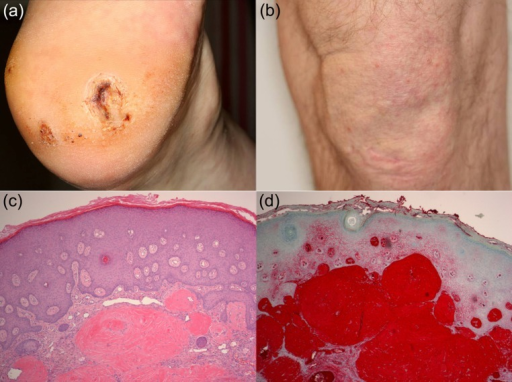
Skin
- Maculopapular lesions, plaques, or nodules[2][3][4]
- Purpura
- Raynaud phenomenon
- Petechiae (if platelet count is low)
- Skin ulcers
- Skin necrosis
- Cold urticaria
- Firm, flesh-colored skin papules and nodules also called macroglobulinemia cutis[3]
 |
 |
 |
HEENT
- Pallor
- Papilledema
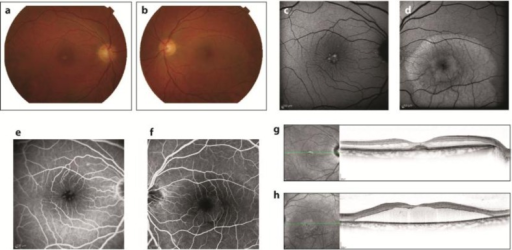
- Malignant vitreitis[5]
- Congestion/sludging of blood in conjunctival vessels
- Retinitis/retinopathy including dilation, segmentation and tortuosity of retinal vessels, mid-peripheral retinal hemorrhages, serous retinal/macular neurosensory detachment, blurred disc margins and fundal exudates on fundoscopic examination[6][7][8]
 |
 |
 |
 |
Neck
Respiratory
- Pleural effusion - in 3-5% of patients[10]
- Rales on auscultation
- Pulmonary infiltrates, nodules, masses[10]
Cardiovascular system
Abdomen
- Swollen abdomen/belly
- Splenomegaly
- Hepatomegaly
Extremity
- Raynaud phenomenon
- Patients may have peripheral edema if disease is complicated by congestive heart failure
Neuromuscular
- Peripheral neuropathy - distal, symmetric, and sensorimotor[11]
References
- ↑ Waldenström's macroglobulinemia. MedlinePlus (2015) https://www.nlm.nih.gov/medlineplus/ency/article/000588.htm Accessed on November 15th, 2015
- ↑ Lin P, Bueso-Ramos C, Wilson CS, Mansoor A, Medeiros LJ (2003). "Waldenstrom macroglobulinemia involving extramedullary sites: morphologic and immunophenotypic findings in 44 patients". Am J Surg Pathol. 27 (8): 1104–13. PMID 12883242.
- ↑ 3.0 3.1 Daoud MS, Lust JA, Kyle RA, Pittelkow MR (1999). "Monoclonal gammopathies and associated skin disorders". J Am Acad Dermatol. 40 (4): 507–35, quiz 536-8. PMID 10188670.
- ↑ Veltman GA, van Veen S, Kluin-Nelemans JC, Bruijn JA, van Es LA (1997). "Renal disease in Waldenström's macroglobulinaemia". Nephrol Dial Transplant. 12 (6): 1256–9. PMID 9198063.
- ↑ Orellana J, Friedman AH (1981). "Ocular manifestations of multiple myeloma, Waldenström's macroglobulinemia and benign monoclonal gammopathy". Surv Ophthalmol. 26 (3): 157–69. PMID 6801795.
- ↑ Pilon AF, Rhee PS, Messner LV (2005). "Bilateral, persistent serous macular detachments with Waldenström's macroglobulinemia". Optom Vis Sci. 82 (7): 573–8. PMID 16044069.
- ↑ Avashia JH, Fath DF (1989). "Bilateral central retinal vein occlusion in Waldenström's macroglobulinemia". J Am Optom Assoc. 60 (9): 657–8. PMID 2507620.
- ↑ Goen TM, Terry JE (1986). "Mid-peripheral hemorrhages secondary to Waldenström's macroglobulinemia". J Am Optom Assoc. 57 (2): 109–12. PMID 3081619.
- ↑ Dimopoulos, Meletios A.; Panayiotidis, Panayiotis; Moulopoulos, Lia A.; Sfikakis, Petros; Dalakas, Marinos (2000). "Waldenström's Macroglobulinemia: Clinical Features, Complications, and Management". Journal of Clinical Oncology. 18 (1): 214–214. doi:10.1200/JCO.2000.18.1.214. ISSN 0732-183X.
- ↑ 10.0 10.1 Fadil A, Taylor DE (1998). "The lung and Waldenström's macroglobulinemia". South Med J. 91 (7): 681–5. PMID 9671845.
- ↑ Coimbra J, Costa AP, Pita F, Rosado P, de Almeida LB (1995). "[Neuropathy in Waldenstrom's macroglobulinemia]". Acta Med Port (in Portuguese). 8 (4): 253–7. PMID 7625222.