Topiramate warnings and precautions: Difference between revisions
No edit summary |
Gerald Chi (talk | contribs) mNo edit summary |
||
| (2 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{PB}} | {{CMG}}; {{AE}} {{PB}} | ||
'''''For patient information, click [[Topiramate (patient information)|here]]''''' | '''''For patient information about topiramate, click [[Topiramate (patient information)|here]].''''' | ||
==Warnings and Precautions== | ==Warnings and Precautions== | ||
| Line 18: | Line 18: | ||
* [[Hypothermia]] has been reported with and without [[hyperammonemia]] during topiramate treatment with concomitant valproic acid use. | * [[Hypothermia]] has been reported with and without [[hyperammonemia]] during topiramate treatment with concomitant valproic acid use. | ||
===Acute Myopia and Secondary Angle Closure Glaucoma=== | |||
A syndrome consisting of acute myopia associated with secondary angle closure glaucoma has been reported in patients receiving topiramate. Symptoms include acute onset of decreased visual acuity and/or ocular pain. Ophthalmologic findings can include myopia, anterior chamber shallowing, ocular hyperemia (redness), and increased [[intraocular pressure]]. [[Mydriasis]] may or may not be present. This syndrome may be associated with supraciliary effusion resulting in anterior displacement of the lens and iris, with secondary angle closure glaucoma. Symptoms typically occur within 1 month of initiating topiramate therapy. In contrast to primary narrow angle glaucoma, which is rare under 40 years of age, secondary angle closure glaucoma associated with topiramate has been reported in pediatric patients as well as adults. The primary treatment to reverse symptoms is discontinuation of topiramate as rapidly as possible, according to the judgment of the treating physician. Other measures, in conjunction with discontinuation of topiramate, may be helpful. | A syndrome consisting of acute myopia associated with secondary angle closure glaucoma has been reported in patients receiving topiramate. Symptoms include acute onset of decreased visual acuity and/or ocular pain. Ophthalmologic findings can include myopia, anterior chamber shallowing, ocular hyperemia (redness), and increased [[intraocular pressure]]. [[Mydriasis]] may or may not be present. This syndrome may be associated with supraciliary effusion resulting in anterior displacement of the lens and iris, with secondary angle closure glaucoma. Symptoms typically occur within 1 month of initiating topiramate therapy. In contrast to primary narrow angle glaucoma, which is rare under 40 years of age, secondary angle closure glaucoma associated with topiramate has been reported in pediatric patients as well as adults. The primary treatment to reverse symptoms is discontinuation of topiramate as rapidly as possible, according to the judgment of the treating physician. Other measures, in conjunction with discontinuation of topiramate, may be helpful. | ||
| Line 31: | Line 29: | ||
The majority of the reports have been in pediatric patients. Patients, especially pediatric patients, treated with topiramate should be monitored closely for evidence of decreased sweating and increased body temperature, especially in hot weather. Caution should be used when topiramate is prescribed with other drugs that predispose patients to heat-related disorders; these drugs include, but are not limited to, other carbonic anhydrase inhibitors and drugs with anticholinergic activity. | The majority of the reports have been in pediatric patients. Patients, especially pediatric patients, treated with topiramate should be monitored closely for evidence of decreased sweating and increased body temperature, especially in hot weather. Caution should be used when topiramate is prescribed with other drugs that predispose patients to heat-related disorders; these drugs include, but are not limited to, other carbonic anhydrase inhibitors and drugs with anticholinergic activity. | ||
===Metabolic Acidosis=== | ===Metabolic Acidosis=== | ||
Hyperchloremic, non-anion gap, [[metabolic acidosis]] (i.e., decreased serum [[bicarbonate]] below the normal reference range in the absence of chronic respiratory alkalosis) is associated with topiramate treatment. This metabolic acidosis is caused by renal bicarbonate loss due to the inhibitory effect of topiramate on [[carbonic anhydrase]]. Such electrolyte imbalance has been observed with the use of topiramate in placebo-controlled clinical trials and in the postmarketing period. Generally, topiramate-induced metabolic acidosis occurs early in treatment although cases can occur at any time during treatment. Bicarbonate decrements are usually mild-moderate (average decrease of 4 mEq/L at daily doses of 400 mg in adults and at approximately 6 mg/kg/day in pediatric patients); rarely, patients can experience severe decrements to values below 10 mEq/L. Conditions or therapies that predispose patients to acidosis (such as renal disease, severe respiratory disorders, [[status epilepticus]], [[diarrhea]], ketogenic diet, or specific drugs) may be additive to the bicarbonate lowering effects of topiramate. | Hyperchloremic, non-anion gap, [[metabolic acidosis]] (i.e., decreased serum [[bicarbonate]] below the normal reference range in the absence of chronic respiratory alkalosis) is associated with topiramate treatment. This metabolic acidosis is caused by renal bicarbonate loss due to the inhibitory effect of topiramate on [[carbonic anhydrase]]. Such electrolyte imbalance has been observed with the use of topiramate in placebo-controlled clinical trials and in the postmarketing period. Generally, topiramate-induced metabolic acidosis occurs early in treatment although cases can occur at any time during treatment. Bicarbonate decrements are usually mild-moderate (average decrease of 4 mEq/L at daily doses of 400 mg in adults and at approximately 6 mg/kg/day in pediatric patients); rarely, patients can experience severe decrements to values below 10 mEq/L. Conditions or therapies that predispose patients to acidosis (such as renal disease, severe respiratory disorders, [[status epilepticus]], [[diarrhea]], ketogenic diet, or specific drugs) may be additive to the bicarbonate lowering effects of topiramate. | ||
| Line 58: | Line 57: | ||
Table 4 shows absolute and relative risk by indication for all evaluated AEDs. | Table 4 shows absolute and relative risk by indication for all evaluated AEDs. | ||
{| | {| | ||
|[[Image:Topiramate4.PNG|thumb|800px]] | |[[Image:Topiramate4.PNG|thumb|800px]] | ||
|} | |} | ||
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. | The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. | ||
| Line 74: | Line 71: | ||
Adverse reactions most often associated with the use of topiramate were related to the central nervous system and were observed in the epilepsy and other populations. In adults, the most frequent of these can be classified into three general categories: 1) Cognitive-related dysfunction (e.g., confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems, particularly word-finding difficulties); 2) Psychiatric/behavioral disturbances (e.g., depression or mood problems); and 3) Somnolence or fatigue. | Adverse reactions most often associated with the use of topiramate were related to the central nervous system and were observed in the epilepsy and other populations. In adults, the most frequent of these can be classified into three general categories: 1) Cognitive-related dysfunction (e.g., confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems, particularly word-finding difficulties); 2) Psychiatric/behavioral disturbances (e.g., depression or mood problems); and 3) Somnolence or fatigue. | ||
===Adult Patients === | ===Adult Patients=== | ||
Cognitive-Related Dysfunction | ====Cognitive-Related Dysfunction==== | ||
The majority of cognitive-related adverse reactions were mild to moderate in severity, and they frequently occurred in isolation. Rapid titration rate and higher initial dose were associated with higher incidences of these reactions. Many of these reactions contributed to withdrawal from treatment [see Adverse Reactions | The majority of cognitive-related adverse reactions were mild to moderate in severity, and they frequently occurred in isolation. Rapid titration rate and higher initial dose were associated with higher incidences of these reactions. Many of these reactions contributed to withdrawal from treatment [see Adverse Reactions. | ||
In the add-on epilepsy controlled trials (using rapid titration such as 100 to 200 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 42% for 200 mg/day, 41% for 400 mg/day, 52% for 600 mg/day, 56% for 800 and 1,000 mg/day, and 14% for placebo. These dose-related adverse reactions began with a similar frequency in the titration or in the maintenance phase, although in some patients the events began during titration and persisted into the maintenance phase. Some patients who experienced one or more cognitive-related adverse reactions in the titration phase had a dose-related recurrence of these reactions in the maintenance phase. | In the add-on epilepsy controlled trials (using rapid titration such as 100 to 200 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 42% for 200 mg/day, 41% for 400 mg/day, 52% for 600 mg/day, 56% for 800 and 1,000 mg/day, and 14% for placebo. These dose-related adverse reactions began with a similar frequency in the titration or in the maintenance phase, although in some patients the events began during titration and persisted into the maintenance phase. Some patients who experienced one or more cognitive-related adverse reactions in the titration phase had a dose-related recurrence of these reactions in the maintenance phase. | ||
| Line 86: | Line 83: | ||
In the 6-month controlled trials for another indication using a slower titration regimen (25 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 19% for topiramate 50 mg/day, 22% for 100 mg/day (the recommended dose), 28% for 200 mg/day, and 10% for placebo. These dose-related adverse reactions typically began in the titration phase and often persisted into the maintenance phase, but infrequently began in the maintenance phase. Some patients experienced a recurrence of one or more of these cognitive adverse reactions and this recurrence was typically in the titration phase. A relatively small proportion of topiramate-treated patients experienced more than one concurrent cognitive adverse reaction. The most common cognitive adverse reactions occurring together included difficulty with memory along with difficulty with concentration/attention, difficulty with memory along with language problems, and difficulty with concentration/attention along with language problems. Rarely, topiramate-treated patients experienced three concurrent cognitive reactions. | In the 6-month controlled trials for another indication using a slower titration regimen (25 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 19% for topiramate 50 mg/day, 22% for 100 mg/day (the recommended dose), 28% for 200 mg/day, and 10% for placebo. These dose-related adverse reactions typically began in the titration phase and often persisted into the maintenance phase, but infrequently began in the maintenance phase. Some patients experienced a recurrence of one or more of these cognitive adverse reactions and this recurrence was typically in the titration phase. A relatively small proportion of topiramate-treated patients experienced more than one concurrent cognitive adverse reaction. The most common cognitive adverse reactions occurring together included difficulty with memory along with difficulty with concentration/attention, difficulty with memory along with language problems, and difficulty with concentration/attention along with language problems. Rarely, topiramate-treated patients experienced three concurrent cognitive reactions. | ||
Psychiatric/Behavioral Disturbances | ====Psychiatric/Behavioral Disturbances==== | ||
Psychiatric/behavioral disturbances (depression or mood) were dose-related for the epilepsy and other populations [see Warnings and Precautions (5.4)]. | Psychiatric/behavioral disturbances ([[depression]] or mood) were dose-related for the [[epilepsy]] and other populations [see Warnings and Precautions (5.4)]. | ||
Somnolence/Fatigue | ====Somnolence/Fatigue==== | ||
Somnolence and fatigue were the adverse reactions most frequently reported during clinical trials of topiramate for adjunctive epilepsy. For the adjunctive epilepsy population, the incidence of somnolence did not differ substantially between 200 mg/day and 1,000 mg/day, but the incidence of fatigue was dose-related and increased at dosages above 400 mg/day. For the monotherapy epilepsy population in the 50 mg/day and 400 mg/day groups, the incidence of somnolence was dose-related (9% for the 50 mg/day group and 15% for the 400 mg/day group) and the incidence of fatigue was comparable in both treatment groups (14% each). For another population, fatigue and somnolence were dose-related and more common in the titration phase. | Somnolence and fatigue were the adverse reactions most frequently reported during clinical trials of topiramate for adjunctive epilepsy. For the adjunctive epilepsy population, the incidence of somnolence did not differ substantially between 200 mg/day and 1,000 mg/day, but the incidence of fatigue was dose-related and increased at dosages above 400 mg/day. For the monotherapy epilepsy population in the 50 mg/day and 400 mg/day groups, the incidence of somnolence was dose-related (9% for the 50 mg/day group and 15% for the 400 mg/day group) and the incidence of fatigue was comparable in both treatment groups (14% each). For another population, [[fatigue]] and [[somnolence]] were dose-related and more common in the titration phase. | ||
Additional nonspecific CNS events commonly observed with topiramate in the add-on epilepsy population included dizziness or ataxia. | Additional nonspecific CNS events commonly observed with topiramate in the add-on epilepsy population included [[dizziness]] or [[ataxia]]. | ||
Pediatric Patients | ===Pediatric Patients=== | ||
In double-blind adjunctive therapy and monotherapy epilepsy clinical studies, the incidences of cognitive/neuropsychiatric adverse reactions in pediatric patients were generally lower than observed in adults. These reactions included psychomotor slowing, difficulty with concentration/attention, speech disorders/related speech problems, and language problems. The most frequently reported neuropsychiatric reactions in pediatric patients during adjunctive therapy double-blind studies were somnolence and fatigue. The most frequently reported neuropsychiatric reactions in pediatric patients in the 50 mg/day and 400 mg/day groups during the monotherapy double-blind study were headache, dizziness, anorexia, and somnolence. | In double-blind adjunctive therapy and monotherapy epilepsy clinical studies, the incidences of cognitive/[[neuropsychiatric]] adverse reactions in pediatric patients were generally lower than observed in adults. These reactions included psychomotor slowing, difficulty with concentration/attention, speech disorders/related speech problems, and language problems. The most frequently reported [[neuropsychiatric]] reactions in pediatric patients during adjunctive therapy double-blind studies were [[somnolence]] and [[fatigue]]. The most frequently reported [[neuropsychiatric]] reactions in pediatric patients in the 50 mg/day and 400 mg/day groups during the monotherapy double-blind study were [[headache]], [[dizziness]], [[anorexia]], and [[somnolence]]. | ||
No patients discontinued treatment due to any adverse reactions in the adjunctive epilepsy double-blind trials. In the monotherapy epilepsy double-blind trial, 1 pediatric patient (2%) in the 50 mg/day group and 7 pediatric patients (12%) in the 400 mg/day group discontinued treatment due to any adverse reactions. The most common adverse reaction associated with discontinuation of therapy was difficulty with concentration/attention; all occurred in the 400 mg/day group. | No patients discontinued treatment due to any adverse reactions in the adjunctive epilepsy double-blind trials. In the monotherapy epilepsy double-blind trial, 1 pediatric patient (2%) in the 50 mg/day group and 7 pediatric patients (12%) in the 400 mg/day group discontinued treatment due to any adverse reactions. The most common adverse reaction associated with discontinuation of therapy was difficulty with concentration/attention; all occurred in the 400 mg/day group. | ||
===Fetal Toxicity=== | |||
Topiramate can cause fetal harm when administered to a pregnant woman. Data from pregnancy registries indicate that infants exposed to topiramate in utero have an increased risk for cleft lip and/or cleft palate (oral clefts). When multiple species of pregnant animals received topiramate at clinically relevant doses, structural malformations, including craniofacial defects, and reduced fetal weights occurred in offspring [see Use in Specific Populations (8.1)]. | Topiramate can cause fetal harm when administered to a pregnant woman. Data from pregnancy registries indicate that infants exposed to topiramate in utero have an increased risk for cleft lip and/or cleft palate (oral clefts). When multiple species of pregnant animals received topiramate at clinically relevant doses, structural malformations, including craniofacial defects, and reduced fetal weights occurred in offspring [see Use in Specific Populations (8.1)]. | ||
Consider the benefits and the risks of topiramate when administering this drug in women of childbearing potential, particularly when topiramate is considered for a condition not usually associated with permanent injury or death [see Use in Specific Populations (8.9) and Patient Counseling Information (17.8)]. Topiramate should be used during pregnancy only if the potential benefit outweighs the potential risk. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1) and (8.9)]. | Consider the benefits and the risks of topiramate when administering this drug in women of childbearing potential, particularly when topiramate is considered for a condition not usually associated with permanent injury or death [see Use in Specific Populations (8.9) and Patient Counseling Information (17.8)]. Topiramate should be used during pregnancy only if the potential benefit outweighs the potential risk. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1) and (8.9)]. | ||
====Withdrawal of Antiepileptic Drugs (AEDs)==== | |||
In patients with or without a history of seizures or epilepsy, antiepileptic drugs, including topiramate, should be gradually withdrawn to minimize the potential for seizures or increased seizure frequency [see Clinical Studies (14)]. In situations where rapid withdrawal of topiramate is medically required, appropriate monitoring is recommended. | In patients with or without a history of seizures or epilepsy, [[antiepileptic]] drugs, including topiramate, should be gradually withdrawn to minimize the potential for seizures or increased seizure frequency [see Clinical Studies (14)]. In situations where rapid withdrawal of topiramate is medically required, appropriate monitoring is recommended. | ||
====Sudden Unexplained Death in Epilepsy (SUDEP)==== | |||
During the course of premarketing development of topiramate tablets, 10 sudden and unexplained deaths were recorded among a cohort of treated patients (2796 subject years of exposure). This represents an incidence of 0.0035 deaths per patient year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving topiramate (ranging from 0.0005 for the general population of patients with epilepsy, to 0.003 for a clinical trial population similar to that in the topiramate program, to 0.005 for patients with refractory epilepsy). | During the course of premarketing development of topiramate tablets, 10 sudden and unexplained deaths were recorded among a cohort of treated patients (2796 subject years of exposure). This represents an incidence of 0.0035 deaths per patient year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving topiramate (ranging from 0.0005 for the general population of patients with epilepsy, to 0.003 for a clinical trial population similar to that in the topiramate program, to 0.005 for patients with refractory epilepsy). | ||
====Hyperammonemia and Encephalopathy (Without and With Concomitant Valproic Acid [VPA] Use)==== | |||
Hyperammonemia/Encephalopathy Without Concomitant Valproic Acid (VPA) | [[Hyperammonemia]]/[[Encephalopathy]] Without Concomitant [[Valproic Acid]] (VPA) | ||
Topiramate treatment has produced hyperammonemia (in some instances dose-related) in clinical investigational programs of adolescents (12 to 16 years) who were treated with topiramate monotherapy for another indication (incidence above the upper limit of normal, 22% for placebo, 26% for 50 mg/day, 41% for 100 mg/day) and in very young pediatric patients (1 to 24 months) who were treated with adjunctive topiramate for partial onset epilepsy (8% for placebo, 10% for 5 mg/kg/day, 0% for 15 mg/kg/day, 9% for 25 mg/kg/day). Topiramate is not approved as monotherapy for another indication in adolescent patients or as adjunctive treatment of partial onset seizures in pediatric patients less than 2 years old. In some patients, ammonia was markedly increased (>50% above upper limit of normal). In adolescent patients, the incidence of markedly increased hyperammonemia was 6% for placebo, 6% for 50 mg, and 12% for 100 mg topiramate daily. The hyperammonemia associated with topiramate treatment occurred with and without encephalopathy in placebo-controlled trials and in an open-label, extension trial. Dose-related hyperammonemia was also observed in the extension trial in pediatric patients up to 2 years old. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. | Topiramate treatment has produced [[hyperammonemia]] (in some instances dose-related) in clinical investigational programs of adolescents (12 to 16 years) who were treated with topiramate monotherapy for another indication (incidence above the upper limit of normal, 22% for placebo, 26% for 50 mg/day, 41% for 100 mg/day) and in very young pediatric patients (1 to 24 months) who were treated with adjunctive topiramate for partial onset epilepsy (8% for placebo, 10% for 5 mg/kg/day, 0% for 15 mg/kg/day, 9% for 25 mg/kg/day). Topiramate is not approved as monotherapy for another indication in adolescent patients or as adjunctive treatment of partial onset seizures in pediatric patients less than 2 years old. In some patients, ammonia was markedly increased (>50% above upper limit of normal). In adolescent patients, the incidence of markedly increased [[hyperammonemia]] was 6% for placebo, 6% for 50 mg, and 12% for 100 mg topiramate daily. The [[hyperammonemia]] associated with topiramate treatment occurred with and without encephalopathy in placebo-controlled trials and in an open-label, extension trial. Dose-related [[hyperammonemia]] was also observed in the extension trial in pediatric patients up to 2 years old. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. | ||
Hyperammonemia with and without encephalopathy has also been observed in postmarketing reports in patients who were taking topiramate without concomitant valproic acid (VPA). | Hyperammonemia with and without encephalopathy has also been observed in postmarketing reports in patients who were taking topiramate without concomitant valproic acid (VPA). | ||
Hyperammonemia/Encephalopathy With Concomitant Valproic Acid (VPA) | =====Hyperammonemia/Encephalopathy With Concomitant Valproic Acid (VPA)===== | ||
Concomitant administration of topiramate and valproic acid (VPA) has been associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone based upon postmarketing reports. Although hyperammonemia may be asymptomatic, clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. In most cases, symptoms and signs abated with discontinuation of either drug. This adverse reaction is not due to a pharmacokinetic interaction. | Concomitant administration of topiramate and valproic acid (VPA) has been associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone based upon postmarketing reports. Although hyperammonemia may be asymptomatic, clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. In most cases, symptoms and signs abated with discontinuation of either drug. This adverse reaction is not due to a pharmacokinetic interaction. | ||
| Line 130: | Line 127: | ||
The hyperammonemia associated with topiramate treatment appears to be more common when topiramate is used concomitantly with VPA. | The hyperammonemia associated with topiramate treatment appears to be more common when topiramate is used concomitantly with VPA. | ||
Monitoring for Hyperammonemia | ====Monitoring for Hyperammonemia==== | ||
Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at an increased risk for hyperammonemia with or without encephalopathy. Although not studied, topiramate treatment or an interaction of concomitant topiramate and valproic acid treatment may exacerbate existing defects or unmask deficiencies in susceptible persons. | Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at an increased risk for hyperammonemia with or without encephalopathy. Although not studied, topiramate treatment or an interaction of concomitant topiramate and valproic acid treatment may exacerbate existing defects or unmask deficiencies in susceptible persons. | ||
In patients who develop unexplained lethargy, vomiting, or changes in mental status associated with any topiramate treatment, hyperammonemic encephalopathy should be considered and an ammonia level should be measured. | In patients who develop unexplained [[lethargy]], [[vomiting]], or changes in mental status associated with any topiramate treatment, hyperammonemic [[encephalopathy]] should be considered and an ammonia level should be measured. | ||
====Kidney Stones==== | |||
A total of 32/2086 (1.5%) of adults exposed to topiramate during its adjunctive epilepsy therapy development reported the occurrence of kidney stones, an incidence about 2 to 4 times greater than expected in a similar, untreated population. In the double-blind monotherapy epilepsy study, a total of 4/319 (1.3%) of adults exposed to topiramate reported the occurrence of kidney stones. As in the general population, the incidence of stone formation among topiramate-treated patients was higher in men. Kidney stones have also been reported in pediatric patients. During long-term (up to 1 year) topiramate treatment in an open-label extension study of 284 pediatric patients 1 to 24 months old with epilepsy, 7% developed kidney or bladder stones that were diagnosed clinically or by sonogram. Topiramate is not approved for pediatric patients less than 2 years old [see Use in Specific Populations (8.4)]. | A total of 32/2086 (1.5%) of adults exposed to topiramate during its adjunctive epilepsy therapy development reported the occurrence of kidney stones, an incidence about 2 to 4 times greater than expected in a similar, untreated population. In the double-blind monotherapy epilepsy study, a total of 4/319 (1.3%) of adults exposed to topiramate reported the occurrence of kidney stones. As in the general population, the incidence of stone formation among topiramate-treated patients was higher in men. Kidney stones have also been reported in pediatric patients. During long-term (up to 1 year) topiramate treatment in an open-label extension study of 284 pediatric patients 1 to 24 months old with epilepsy, 7% developed kidney or bladder stones that were diagnosed clinically or by sonogram. Topiramate is not approved for pediatric patients less than 2 years old [see Use in Specific Populations (8.4)]. | ||
An explanation for the association of topiramate and kidney stones may lie in the fact that topiramate is a carbonic anhydrase inhibitor. Carbonic anhydrase inhibitors (e.g., zonisamide, acetazolamide, or dichlorphenamide) can promote stone formation by reducing urinary citrate excretion and by increasing urinary pH [see Warnings and Precautions (5.3)]. The concomitant use of topiramate with any other drug producing metabolic acidosis, or potentially in patients on a ketogenic diet, may create a physiological environment that increases the risk of kidney stone formation, and should therefore be avoided. | An explanation for the association of topiramate and kidney stones may lie in the fact that topiramate is a carbonic anhydrase inhibitor. [[Carbonic anhydrase inhibitors]] (e.g., zonisamide, acetazolamide, or dichlorphenamide) can promote stone formation by reducing urinary citrate excretion and by increasing urinary pH [see Warnings and Precautions (5.3)]. The concomitant use of topiramate with any other drug producing [[metabolic acidosis]], or potentially in patients on a ketogenic diet, may create a physiological environment that increases the risk of kidney stone formation, and should therefore be avoided. | ||
Increased fluid intake increases the urinary output, lowering the concentration of substances involved in stone formation. Hydration is recommended to reduce new stone formation. | Increased fluid intake increases the urinary output, lowering the concentration of substances involved in stone formation. Hydration is recommended to reduce new stone formation. | ||
====Hypothermia with Concomitant Valproic Acid (VPA) Use==== | |||
Hypothermia, defined as an unintentional drop in body core temperature to <35°C (95°F), has been reported in association with topiramate use with concomitant valproic acid (VPA) both in conjunction with hyperammonemia and in the absence of hyperammonemia. This adverse reaction in patients using concomitant topiramate and valproate can occur after starting topiramate treatment or after increasing the daily dose of topiramate [see Drug Interactions (7.1)]. Consideration should be given to stopping topiramate or valproate in patients who develop hypothermia, which may be manifested by a variety of clinical abnormalities including lethargy, confusion, coma, and significant alterations in other major organ systems such as the cardiovascular and respiratory systems. Clinical management and assessment should include examination of blood ammonia levels. | |||
[[Hypothermia]], defined as an unintentional drop in body core temperature to <35°C (95°F), has been reported in association with topiramate use with concomitant [[valproic acid]] (VPA) both in conjunction with [[hyperammonemia]] and in the absence of [[hyperammonemia]]. This adverse reaction in patients using concomitant topiramate and valproate can occur after starting topiramate treatment or after increasing the daily dose of topiramate [see Drug Interactions (7.1)]. Consideration should be given to stopping topiramate or [[valproate]] in patients who develop hypothermia, which may be manifested by a variety of clinical abnormalities including lethargy, [[confusion]], [[coma]], and significant alterations in other major organ systems such as the cardiovascular and respiratory systems. Clinical management and assessment should include examination of blood ammonia levels. | |||
====Paresthesia==== | |||
[[Paresthesia]] (usually tingling of the extremities), an effect associated with the use of other carbonic anhydrase inhibitors, appears to be a common effect of topiramate. [[Paresthesia]] was more frequently reported in the monotherapy epilepsy trials and trials for another indication than in the adjunctive therapy epilepsy trials. In the majority of instances, [[paresthesia]] did not lead to treatment discontinuation. | |||
Paresthesia (usually tingling of the extremities), an effect associated with the use of other carbonic anhydrase inhibitors, appears to be a common effect of topiramate. Paresthesia was more frequently reported in the monotherapy epilepsy trials and trials for another indication than in the adjunctive therapy epilepsy trials. In the majority of instances, paresthesia did not lead to treatment discontinuation. | |||
====Adjustment of Dose in Renal Failure==== | |||
The major route of elimination of unchanged topiramate and its metabolites is via the kidney. Dosage adjustment may be required in patients with reduced renal function [see Dosage and Administration (2.4)]. | The major route of elimination of unchanged topiramate and its metabolites is via the kidney. Dosage adjustment may be required in patients with reduced renal function [see Dosage and Administration (2.4)]. | ||
====Decreased Hepatic Function==== | |||
In hepatically impaired patients, topiramate should be administered with caution as the clearance of topiramate may be decreased [see Dosage and Administration (2.7)]. | In hepatically impaired patients, topiramate should be administered with caution as the clearance of topiramate may be decreased [see Dosage and Administration (2.7)]. | ||
====Monitoring: Laboratory Tests==== | |||
Topiramate treatment was associated with changes in several clinical laboratory analytes in randomized, double-blind, placebo-controlled studies. | Topiramate treatment was associated with changes in several clinical laboratory analytes in randomized, double-blind, placebo-controlled studies. | ||
Topiramate treatment causes non-anion gap, hyperchloremic metabolic acidosis manifested by a decrease in serum bicarbonate and an increase in serum chloride. Measurement of baseline and periodic serum bicarbonate during topiramate treatment is recommended [see Warnings and Precautions (5.3)]. | Topiramate treatment causes non-anion gap, hyperchloremic [[metabolic acidosis]] manifested by a decrease in serum bicarbonate and an increase in serum chloride. Measurement of baseline and periodic serum [[bicarbonate]] during topiramate treatment is recommended [see Warnings and Precautions (5.3)]. | ||
Controlled trials of adjunctive topiramate treatment of adults for partial onset seizures showed an increased incidence of markedly decreased serum phosphorus (6% topiramate, 2% placebo),markedly increased serum alkaline phosphatase (3% topiramate, 1% placebo), and decreased serum potassium (0.4% topiramate, 0.1% placebo). The clinical significance of these abnormalities has not been clearly established. | Controlled trials of adjunctive topiramate treatment of adults for partial onset [[seizures]] showed an increased incidence of markedly decreased serum phosphorus (6% topiramate, 2% placebo),markedly increased serum alkaline phosphatase (3% topiramate, 1% placebo), and decreased serum potassium (0.4% topiramate, 0.1% placebo). The clinical significance of these abnormalities has not been clearly established. | ||
Changes in several clinical laboratory values (i.e., increased creatinine, BUN, alkaline phosphatase, total protein, total eosinophil count, and decreased potassium) have been observed in a clinical investigational program in very young (<2 years) pediatric patients who were treated with adjunctive topiramate for partial onset seizures [see Use in Specific Populations (8.4)]. | Changes in several clinical laboratory values (i.e., increased creatinine, [[BUN]], [[alkaline phosphatase]], total protein, total [[eosinophil]] count, and decreased potassium) have been observed in a clinical investigational program in very young (<2 years) pediatric patients who were treated with adjunctive topiramate for partial onset seizures [see Use in Specific Populations (8.4)]. | ||
Topiramate treatment produced a dose-related increased shift in serum creatinine from normal at baseline to an increased value at the end of 4 months treatment in adolescent patients (ages 12 to 16 years) who were treated for another indication in a double-blind, placebo-controlled study. | Topiramate treatment produced a dose-related increased shift in serum [[creatinine]] from normal at baseline to an increased value at the end of 4 months treatment in adolescent patients (ages 12 to 16 years) who were treated for another indication in a double-blind, placebo-controlled study. | ||
Topiramate treatment with or without concomitant valproic acid (VPA) can cause hyperammonemia with or without encephalopathy [see Warnings and Precautions (5.9)].<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = TOPIRAMATE (TOPIRAMATE ) TABLET, FILM COATED [AUROBINDO PHARMA LIMITED] | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=32b48ea0-a215-43b8-83b4-a5435a686d68 | publisher = | date = | accessdate = | Topiramate treatment with or without concomitant valproic acid (VPA) can cause [[hyperammonemia]] with or without [[encephalopathy]] [see Warnings and Precautions (5.9)].<ref name="dailymed.nlm.nih.gov">{{Cite web | last = | first = | title = TOPIRAMATE (TOPIRAMATE ) TABLET, FILM COATED [AUROBINDO PHARMA LIMITED] | url = http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=32b48ea0-a215-43b8-83b4-a5435a686d68 | publisher = | date = | accessdate = }}</ref> | ||
==References== | ==References== | ||
{{Reflist | {{Reflist}} | ||
{{FDA}} | |||
{{Antimigraine preparations}} | {{Antimigraine preparations}} | ||
[[Category:Antimigraine drugs]] | |||
[[Category:Drugs]] | [[Category:Drugs]] | ||
Latest revision as of 02:00, 9 February 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Pratik Bahekar, MBBS [2]
For patient information about topiramate, click here.
Warnings and Precautions
- Acute myopia and secondary angle closure glaucoma: Untreated elevated intraocular pressure can lead to permanent visual loss. The primary treatment to reverse symptoms is discontinuation of topiramate as rapidly as possible.
- Oligohidrosis and hyperthermia: Monitor decreased sweating and increased body temperature, especially in pediatric patients .
- Metabolic acidosis: Baseline and periodic measurement of serum bicarbonate is recommended. Consider dose reduction or discontinuation of topiramate if clinically appropriate.
- Suicidal behavior and ideation: Antiepileptic drugs increase the risk of suicidal behavior or ideation.
- Cognitive/neuropsychiatric: Topiramate may cause cognitive dysfunction. Patients should use caution when operating machinery including automobiles. Depression and mood problems may occur in epilepsy and other populations.
- Fetal Toxicity: Topiramate use during pregnancy can cause cleft lip and/or palate .
- Withdrawal of AEDs: Withdrawal of topiramate should be done gradually .
- Hyperammonemia and encephalopathy associated with or without concomitant valproic acid use: Patients with inborn errors of metabolism or reduced mitochondrial activity may have an increased risk of hyperammonemia. Measure ammonia if encephalopathic symptoms occur.
- Kidney stones: Use with other carbonic anhydrase inhibitors, other drugs causing metabolic acidosis, or in patients on a ketogenic diet should be avoided .
- Hypothermia has been reported with and without hyperammonemia during topiramate treatment with concomitant valproic acid use.
Acute Myopia and Secondary Angle Closure Glaucoma
A syndrome consisting of acute myopia associated with secondary angle closure glaucoma has been reported in patients receiving topiramate. Symptoms include acute onset of decreased visual acuity and/or ocular pain. Ophthalmologic findings can include myopia, anterior chamber shallowing, ocular hyperemia (redness), and increased intraocular pressure. Mydriasis may or may not be present. This syndrome may be associated with supraciliary effusion resulting in anterior displacement of the lens and iris, with secondary angle closure glaucoma. Symptoms typically occur within 1 month of initiating topiramate therapy. In contrast to primary narrow angle glaucoma, which is rare under 40 years of age, secondary angle closure glaucoma associated with topiramate has been reported in pediatric patients as well as adults. The primary treatment to reverse symptoms is discontinuation of topiramate as rapidly as possible, according to the judgment of the treating physician. Other measures, in conjunction with discontinuation of topiramate, may be helpful.
Elevated intraocular pressure of any etiology, if left untreated, can lead to serious sequelae including permanent vision loss.
Oligohidrosis and Hyperthermia
Oligohidrosis (decreased sweating), infrequently resulting in hospitalization, has been reported in association with topiramate use. Decreased sweating and an elevation in body temperature above normal characterized these cases. Some of the cases were reported after exposure to elevated environmental temperatures.
The majority of the reports have been in pediatric patients. Patients, especially pediatric patients, treated with topiramate should be monitored closely for evidence of decreased sweating and increased body temperature, especially in hot weather. Caution should be used when topiramate is prescribed with other drugs that predispose patients to heat-related disorders; these drugs include, but are not limited to, other carbonic anhydrase inhibitors and drugs with anticholinergic activity.
Metabolic Acidosis
Hyperchloremic, non-anion gap, metabolic acidosis (i.e., decreased serum bicarbonate below the normal reference range in the absence of chronic respiratory alkalosis) is associated with topiramate treatment. This metabolic acidosis is caused by renal bicarbonate loss due to the inhibitory effect of topiramate on carbonic anhydrase. Such electrolyte imbalance has been observed with the use of topiramate in placebo-controlled clinical trials and in the postmarketing period. Generally, topiramate-induced metabolic acidosis occurs early in treatment although cases can occur at any time during treatment. Bicarbonate decrements are usually mild-moderate (average decrease of 4 mEq/L at daily doses of 400 mg in adults and at approximately 6 mg/kg/day in pediatric patients); rarely, patients can experience severe decrements to values below 10 mEq/L. Conditions or therapies that predispose patients to acidosis (such as renal disease, severe respiratory disorders, status epilepticus, diarrhea, ketogenic diet, or specific drugs) may be additive to the bicarbonate lowering effects of topiramate.
In adults, the incidence of persistent treatment-emergent decreases in serum bicarbonate (levels of <20 mEq/L at two consecutive visits or at the final visit) in controlled clinical trials for adjunctive treatment of epilepsy was 32% for 400 mg/day, and 1% for placebo. Metabolic acidosis has been observed at doses as low as 50 mg/day. The incidence of persistent treatment-emergent decreases in serum bicarbonate in adults in the epilepsy controlled clinical trial for monotherapy was 15% for 50 mg/day and 25% for 400 mg/day. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in the adjunctive therapy trials was 3% for 400 mg/day, and 0% for placebo and in the monotherapy trial was 1% for 50 mg/day and 7% for 400 mg/day. Serum bicarbonate levels have not been systematically evaluated at daily doses greater than 400 mg/day.
In pediatric patients (2 to 16 years of age), the incidence of persistent treatment-emergent decreases in serum bicarbonate in placebo-controlled trials for adjunctive treatment of Lennox-Gastaut syndrome or refractory partial onset seizures was 67% for topiramate (at approximately 6 mg/kg/day), and 10% for placebo. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in these trials was 11% for topiramate and 0% for placebo. Cases of moderately severe metabolic acidosis have been reported in patients as young as 5 months old, especially at daily doses above 5 mg/kg/day.
Although not approved for use in patients under 2 years of age with partial onset seizures, a controlled trial that examined this population revealed that topiramate produced a metabolic acidosis that is notably greater in magnitude than that observed in controlled trials in older children and adults. The mean treatment difference (25 mg/kg/day topiramate-placebo) was -5.9 mEq/L for bicarbonate. The incidence of metabolic acidosis (defined by a serum bicarbonate < 20 mEq/L) was 0% for placebo, 30% for 5 mg/kg/day, 50% for 15 mg/kg/day, and 45% for 25 mg/kg/day. The incidence of markedly abnormal changes (i.e., < 17 mEq/L and > 5 mEq/L decrease from baseline of ≥ 20 mEq/L) was 0% for placebo, 4% for 5 mg/kg/day, 5% for 15 mg/kg/day, and 5% for 25 mg/kg/day [see Use in Specific Populations (8.4)].
In pediatric patients (6 to 15 years of age), the incidence of persistent treatment-emergent decreases in serum bicarbonate in the epilepsy controlled clinical trial for monotherapy was 9% for 50 mg/day and 25% for 400 mg/day. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in this trial was 1% for 50 mg/day and 6% for 400 mg/day. In adult patients (≥ 16 years of age), the incidence of persistent treatment-emergent decreases in serum bicarbonate in the epilepsy controlled clinical trial for monotherapy was 14 % for 50 mg/day and 25% for 400 mg/day. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in this trial for adults was 1% for 50 mg/day and 6% for 400 mg/day.
The incidence of persistent treatment-emergent decreases in serum bicarbonate in placebo-controlled trials for adults for another indication was 44% for 200 mg/day, 39% for 100 mg/day, 23% for 50 mg/day, and 7% for placebo. The incidence of a markedly abnormally low serum bicarbonate (i.e., absolute value <17 mEq/L and >5 mEq/L decrease from pretreatment) in these trials was 11% for 200 mg/day, 9% for 100 mg/day, 2% for 50 mg/day, and <1% for placebo.
Some manifestations of acute or chronic metabolic acidosis may include hyperventilation, nonspecific symptoms such as fatigue and anorexia, or more severe sequelae including cardiac arrhythmias or stupor. Chronic, untreated metabolic acidosis may increase the risk for nephrolithiasis or nephrocalcinosis, and may also result in osteomalacia (referred to as rickets in pediatric patients) and/or osteoporosis with an increased risk for fractures. Chronic metabolic acidosis in pediatric patients may also reduce growth rates. A reduction in growth rate may eventually decrease the maximal height achieved. The effect of topiramate on growth and bone-related sequelae has not been systematically investigated in long-term, placebo-controlled trials. Long-term, open-label treatment of infants/toddlers, with intractable partial epilepsy, for up to 1 year, showed reductions from baseline in Z SCORES for length, weight, and head circumference compared to age and sex-matched normative data, although these patients with epilepsy are likely to have different growth rates than normal infants. Reductions in Z SCORES for length and weight were correlated to the degree of acidosis [see Use in Specific Populations (8.4)]. Topiramate treatment that causes metabolic acidosis during pregnancy can possibly produce adverse effects on the fetus and might also cause metabolic acidosis in the neonate from possible transfer of topiramate to the fetus [see Warnings and Precautions (5.6) and Use in Specific Populations (8.1)].
Measurement of baseline and periodic serum bicarbonate during topiramate treatment is recommended. If metabolic acidosis develops and persists, consideration should be given to reducing the dose or discontinuing topiramate (using dose tapering). If the decision is made to continue patients on topiramate in the face of persistent acidosis, alkali treatment should be considered.
Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including topiramate, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 4 shows absolute and relative risk by indication for all evaluated AEDs.
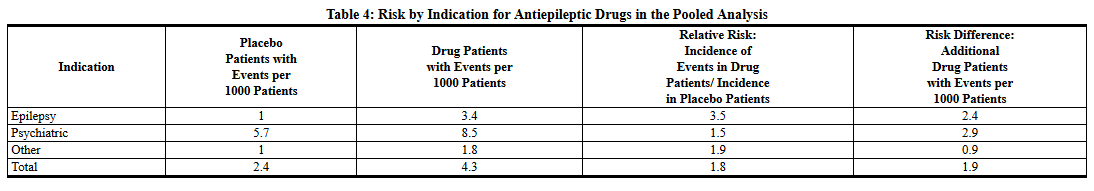 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing topiramate or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior or the emergence of suicidal thoughts, behavior or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Cognitive/Neuropsychiatric Adverse Reactions
Adverse reactions most often associated with the use of topiramate were related to the central nervous system and were observed in the epilepsy and other populations. In adults, the most frequent of these can be classified into three general categories: 1) Cognitive-related dysfunction (e.g., confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems, particularly word-finding difficulties); 2) Psychiatric/behavioral disturbances (e.g., depression or mood problems); and 3) Somnolence or fatigue.
Adult Patients
Cognitive-Related Dysfunction
The majority of cognitive-related adverse reactions were mild to moderate in severity, and they frequently occurred in isolation. Rapid titration rate and higher initial dose were associated with higher incidences of these reactions. Many of these reactions contributed to withdrawal from treatment [see Adverse Reactions.
In the add-on epilepsy controlled trials (using rapid titration such as 100 to 200 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 42% for 200 mg/day, 41% for 400 mg/day, 52% for 600 mg/day, 56% for 800 and 1,000 mg/day, and 14% for placebo. These dose-related adverse reactions began with a similar frequency in the titration or in the maintenance phase, although in some patients the events began during titration and persisted into the maintenance phase. Some patients who experienced one or more cognitive-related adverse reactions in the titration phase had a dose-related recurrence of these reactions in the maintenance phase.
In the monotherapy epilepsy controlled trial, the proportion of patients who experienced one or more cognitive-related adverse reactions was 19% for topiramate 50 mg/day and 26% for 400 mg/day.
In the 6-month controlled trials for another indication using a slower titration regimen (25 mg/day weekly increments), the proportion of patients who experienced one or more cognitive-related adverse reactions was 19% for topiramate 50 mg/day, 22% for 100 mg/day (the recommended dose), 28% for 200 mg/day, and 10% for placebo. These dose-related adverse reactions typically began in the titration phase and often persisted into the maintenance phase, but infrequently began in the maintenance phase. Some patients experienced a recurrence of one or more of these cognitive adverse reactions and this recurrence was typically in the titration phase. A relatively small proportion of topiramate-treated patients experienced more than one concurrent cognitive adverse reaction. The most common cognitive adverse reactions occurring together included difficulty with memory along with difficulty with concentration/attention, difficulty with memory along with language problems, and difficulty with concentration/attention along with language problems. Rarely, topiramate-treated patients experienced three concurrent cognitive reactions.
Psychiatric/Behavioral Disturbances
Psychiatric/behavioral disturbances (depression or mood) were dose-related for the epilepsy and other populations [see Warnings and Precautions (5.4)].
Somnolence/Fatigue
Somnolence and fatigue were the adverse reactions most frequently reported during clinical trials of topiramate for adjunctive epilepsy. For the adjunctive epilepsy population, the incidence of somnolence did not differ substantially between 200 mg/day and 1,000 mg/day, but the incidence of fatigue was dose-related and increased at dosages above 400 mg/day. For the monotherapy epilepsy population in the 50 mg/day and 400 mg/day groups, the incidence of somnolence was dose-related (9% for the 50 mg/day group and 15% for the 400 mg/day group) and the incidence of fatigue was comparable in both treatment groups (14% each). For another population, fatigue and somnolence were dose-related and more common in the titration phase.
Additional nonspecific CNS events commonly observed with topiramate in the add-on epilepsy population included dizziness or ataxia.
Pediatric Patients
In double-blind adjunctive therapy and monotherapy epilepsy clinical studies, the incidences of cognitive/neuropsychiatric adverse reactions in pediatric patients were generally lower than observed in adults. These reactions included psychomotor slowing, difficulty with concentration/attention, speech disorders/related speech problems, and language problems. The most frequently reported neuropsychiatric reactions in pediatric patients during adjunctive therapy double-blind studies were somnolence and fatigue. The most frequently reported neuropsychiatric reactions in pediatric patients in the 50 mg/day and 400 mg/day groups during the monotherapy double-blind study were headache, dizziness, anorexia, and somnolence.
No patients discontinued treatment due to any adverse reactions in the adjunctive epilepsy double-blind trials. In the monotherapy epilepsy double-blind trial, 1 pediatric patient (2%) in the 50 mg/day group and 7 pediatric patients (12%) in the 400 mg/day group discontinued treatment due to any adverse reactions. The most common adverse reaction associated with discontinuation of therapy was difficulty with concentration/attention; all occurred in the 400 mg/day group.
Fetal Toxicity
Topiramate can cause fetal harm when administered to a pregnant woman. Data from pregnancy registries indicate that infants exposed to topiramate in utero have an increased risk for cleft lip and/or cleft palate (oral clefts). When multiple species of pregnant animals received topiramate at clinically relevant doses, structural malformations, including craniofacial defects, and reduced fetal weights occurred in offspring [see Use in Specific Populations (8.1)].
Consider the benefits and the risks of topiramate when administering this drug in women of childbearing potential, particularly when topiramate is considered for a condition not usually associated with permanent injury or death [see Use in Specific Populations (8.9) and Patient Counseling Information (17.8)]. Topiramate should be used during pregnancy only if the potential benefit outweighs the potential risk. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1) and (8.9)].
Withdrawal of Antiepileptic Drugs (AEDs)
In patients with or without a history of seizures or epilepsy, antiepileptic drugs, including topiramate, should be gradually withdrawn to minimize the potential for seizures or increased seizure frequency [see Clinical Studies (14)]. In situations where rapid withdrawal of topiramate is medically required, appropriate monitoring is recommended.
Sudden Unexplained Death in Epilepsy (SUDEP)
During the course of premarketing development of topiramate tablets, 10 sudden and unexplained deaths were recorded among a cohort of treated patients (2796 subject years of exposure). This represents an incidence of 0.0035 deaths per patient year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with epilepsy not receiving topiramate (ranging from 0.0005 for the general population of patients with epilepsy, to 0.003 for a clinical trial population similar to that in the topiramate program, to 0.005 for patients with refractory epilepsy).
Hyperammonemia and Encephalopathy (Without and With Concomitant Valproic Acid [VPA] Use)
Hyperammonemia/Encephalopathy Without Concomitant Valproic Acid (VPA)
Topiramate treatment has produced hyperammonemia (in some instances dose-related) in clinical investigational programs of adolescents (12 to 16 years) who were treated with topiramate monotherapy for another indication (incidence above the upper limit of normal, 22% for placebo, 26% for 50 mg/day, 41% for 100 mg/day) and in very young pediatric patients (1 to 24 months) who were treated with adjunctive topiramate for partial onset epilepsy (8% for placebo, 10% for 5 mg/kg/day, 0% for 15 mg/kg/day, 9% for 25 mg/kg/day). Topiramate is not approved as monotherapy for another indication in adolescent patients or as adjunctive treatment of partial onset seizures in pediatric patients less than 2 years old. In some patients, ammonia was markedly increased (>50% above upper limit of normal). In adolescent patients, the incidence of markedly increased hyperammonemia was 6% for placebo, 6% for 50 mg, and 12% for 100 mg topiramate daily. The hyperammonemia associated with topiramate treatment occurred with and without encephalopathy in placebo-controlled trials and in an open-label, extension trial. Dose-related hyperammonemia was also observed in the extension trial in pediatric patients up to 2 years old. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting.
Hyperammonemia with and without encephalopathy has also been observed in postmarketing reports in patients who were taking topiramate without concomitant valproic acid (VPA).
Hyperammonemia/Encephalopathy With Concomitant Valproic Acid (VPA)
Concomitant administration of topiramate and valproic acid (VPA) has been associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone based upon postmarketing reports. Although hyperammonemia may be asymptomatic, clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting. In most cases, symptoms and signs abated with discontinuation of either drug. This adverse reaction is not due to a pharmacokinetic interaction.
Although topiramate is not indicated for use in infants/toddlers (1 to 24 months), topiramate with concomitant VPA clearly produced a dose-related increase in the incidence of treatment-emergent hyperammonemia (above the upper limit of normal, 0% for placebo, 12% for 5 mg/kg/day, 7% for 15 mg/kg/day, 17% for 25 mg/kg/day) in an investigational program. Markedly increased, dose-related hyperammonemia (0% for placebo and 5 mg/kg/day, 7% for 15 mg/kg/day, 8% for 25 mg/kg/day) also occurred in these infants/toddlers. Dose-related hyperammonemia was similarly observed in a long-term extension trial in these very young, pediatric patients [see Use in Specific Populations (8.4)].
Hyperammonemia with and without encephalopathy has also been observed in postmarketing reports in patients taking topiramate with VPA.
The hyperammonemia associated with topiramate treatment appears to be more common when topiramate is used concomitantly with VPA.
Monitoring for Hyperammonemia
Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at an increased risk for hyperammonemia with or without encephalopathy. Although not studied, topiramate treatment or an interaction of concomitant topiramate and valproic acid treatment may exacerbate existing defects or unmask deficiencies in susceptible persons.
In patients who develop unexplained lethargy, vomiting, or changes in mental status associated with any topiramate treatment, hyperammonemic encephalopathy should be considered and an ammonia level should be measured.
Kidney Stones
A total of 32/2086 (1.5%) of adults exposed to topiramate during its adjunctive epilepsy therapy development reported the occurrence of kidney stones, an incidence about 2 to 4 times greater than expected in a similar, untreated population. In the double-blind monotherapy epilepsy study, a total of 4/319 (1.3%) of adults exposed to topiramate reported the occurrence of kidney stones. As in the general population, the incidence of stone formation among topiramate-treated patients was higher in men. Kidney stones have also been reported in pediatric patients. During long-term (up to 1 year) topiramate treatment in an open-label extension study of 284 pediatric patients 1 to 24 months old with epilepsy, 7% developed kidney or bladder stones that were diagnosed clinically or by sonogram. Topiramate is not approved for pediatric patients less than 2 years old [see Use in Specific Populations (8.4)].
An explanation for the association of topiramate and kidney stones may lie in the fact that topiramate is a carbonic anhydrase inhibitor. Carbonic anhydrase inhibitors (e.g., zonisamide, acetazolamide, or dichlorphenamide) can promote stone formation by reducing urinary citrate excretion and by increasing urinary pH [see Warnings and Precautions (5.3)]. The concomitant use of topiramate with any other drug producing metabolic acidosis, or potentially in patients on a ketogenic diet, may create a physiological environment that increases the risk of kidney stone formation, and should therefore be avoided.
Increased fluid intake increases the urinary output, lowering the concentration of substances involved in stone formation. Hydration is recommended to reduce new stone formation.
Hypothermia with Concomitant Valproic Acid (VPA) Use
Hypothermia, defined as an unintentional drop in body core temperature to <35°C (95°F), has been reported in association with topiramate use with concomitant valproic acid (VPA) both in conjunction with hyperammonemia and in the absence of hyperammonemia. This adverse reaction in patients using concomitant topiramate and valproate can occur after starting topiramate treatment or after increasing the daily dose of topiramate [see Drug Interactions (7.1)]. Consideration should be given to stopping topiramate or valproate in patients who develop hypothermia, which may be manifested by a variety of clinical abnormalities including lethargy, confusion, coma, and significant alterations in other major organ systems such as the cardiovascular and respiratory systems. Clinical management and assessment should include examination of blood ammonia levels.
Paresthesia
Paresthesia (usually tingling of the extremities), an effect associated with the use of other carbonic anhydrase inhibitors, appears to be a common effect of topiramate. Paresthesia was more frequently reported in the monotherapy epilepsy trials and trials for another indication than in the adjunctive therapy epilepsy trials. In the majority of instances, paresthesia did not lead to treatment discontinuation.
Adjustment of Dose in Renal Failure
The major route of elimination of unchanged topiramate and its metabolites is via the kidney. Dosage adjustment may be required in patients with reduced renal function [see Dosage and Administration (2.4)].
Decreased Hepatic Function
In hepatically impaired patients, topiramate should be administered with caution as the clearance of topiramate may be decreased [see Dosage and Administration (2.7)].
Monitoring: Laboratory Tests
Topiramate treatment was associated with changes in several clinical laboratory analytes in randomized, double-blind, placebo-controlled studies.
Topiramate treatment causes non-anion gap, hyperchloremic metabolic acidosis manifested by a decrease in serum bicarbonate and an increase in serum chloride. Measurement of baseline and periodic serum bicarbonate during topiramate treatment is recommended [see Warnings and Precautions (5.3)].
Controlled trials of adjunctive topiramate treatment of adults for partial onset seizures showed an increased incidence of markedly decreased serum phosphorus (6% topiramate, 2% placebo),markedly increased serum alkaline phosphatase (3% topiramate, 1% placebo), and decreased serum potassium (0.4% topiramate, 0.1% placebo). The clinical significance of these abnormalities has not been clearly established.
Changes in several clinical laboratory values (i.e., increased creatinine, BUN, alkaline phosphatase, total protein, total eosinophil count, and decreased potassium) have been observed in a clinical investigational program in very young (<2 years) pediatric patients who were treated with adjunctive topiramate for partial onset seizures [see Use in Specific Populations (8.4)].
Topiramate treatment produced a dose-related increased shift in serum creatinine from normal at baseline to an increased value at the end of 4 months treatment in adolescent patients (ages 12 to 16 years) who were treated for another indication in a double-blind, placebo-controlled study.
Topiramate treatment with or without concomitant valproic acid (VPA) can cause hyperammonemia with or without encephalopathy [see Warnings and Precautions (5.9)].[1]
References
Adapted from the FDA Package Insert.