Penbutolol
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2], Sheng Shi, M.D. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Penbutolol is a beta-adrenergic blocker that is FDA approved for the treatment of hypertension. Common adverse reactions include nausea, dizziness, headache and fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- The usual starting and maintenance dose of penbutolol, used alone or in combination with other antihypertensive agents, such as thiazide-type diuretics, is 20 mg given once daily.
- Doses of 40 mg and 80 mg have been well-tolerated but have not been shown to give a greater antihypertensive effect. The full effect of a 20- or 40-mg dose is seen by the end of 2 weeks. A dose of 10 mg also lowers blood pressure, but the full effect is not seen for 4 to 6 weeks.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Penbutolol in adult patients.
Non–Guideline-Supported Use
Angina Pectoris
- Dosing Information
- 40 mg/day.[1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Penbutolol FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Penbutolol in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Penbutolol in pediatric patients.
Contraindications
- Cardiogenic shock
- Sinus bradycardia
- Second degree heart block
- Third degree heart block
- Bronchial asthma
- Hypersensitivity to penbutolol
Warnings
Cardiac Failure
- Sympathetic stimulation may be essential for supporting circulatory function in patients with heart failure, and its inhibition by ß-adrenergic receptor blockade may precipitate more severe failure. Although ß-blockers should be avoided in overt congestive heart failure, penbutolol can, if necessary, be used with caution in patients with a history of cardiac failure who are well compensated, on treatment with vasodilators, digitalis and/or diuretics. Both digitalis and penbutolol slow AV conduction. Beta-adrenergic receptor antagonists do not inhibit the inotropic action of digitalis on heart muscle. If cardiac failure persists, treatment with penbutolol should be discontinued.
Patients Without History of Cardiac Failure
- Continued depression of the myocardium with ß-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first evidence of heart failure, patients receiving penbutolol should be given appropriate treatment, and the response should be closely observed. If cardiac failure continues despite adequate intervention with appropriate drugs, penbutolol should be withdrawn (gradually, if possible).
Exacerbation of Ischemic Heart Disease Following Abrupt Withdrawal
- Hypersensitivity to catecholamines has been observed in patients who were withdrawn from therapy with ß-blocking agents; exacerbation of angina and, in some cases, myocardial infarction have occurred after abrupt discontinuation of such therapy. When discontinuing penbutolol, particularly in patients with ischemic heart disease, the dosage should be reduced gradually over a period of 1 to 2 weeks and the patient should be monitored carefully. If angina becomes more pronounced or acute coronary insufficiency develops, administration of penbutolol should be reinstated promptly, at least on a temporary basis, and appropriate measures should be taken for the management of unstable angina. Patients should be warned against interruption or discontinuation of therapy without the physician’s advice. Because coronary artery disease is common and may not be recognized, it may not be prudent to discontinue penbutolol abruptly, even in patients who are being treated only for hypertension.
Nonallergic Bronchospasm (eg, chronic bronchitis,emphysema)
- Penbutolol is contraindicated in bronchial asthma. In general, patients with bronchospastic diseases should not receive ß-blockers. Penbutolol should be administered with caution because it may block bronchodilation produced by endogenous catecholamine stimulation of ß-2 receptors.
Major Surgery
- Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Diabetes Mellitus and Hypoglycemia
- Beta-adrenergic receptor blockade may prevent the appearance of signs and symptoms of acute hypoglycemia, such as tachycardia and blood pressure changes. This is especially important in patients with labile diabetes. Beta-blockade also reduces the release of insulin in response to hyperglycemia; therefore, it may be necessary to adjust the dose of hypoglycemic drugs. Beta-adrenergic blockade may also impair the homeostatic response to hypoglycemia; in that event, the spontaneous recovery from hypoglycemia may be delayed during treatment with ß-adrenergic receptor antagonists.
Thyrotoxicosis
- Beta-adrenergic blockade may mask certain clinical signs (eg, tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of ß-adrenergic receptor blockers that might precipitate a thyroid storm.
Adverse Reactions
Clinical Trials Experience
- Penbutolol is usually well tolerated in properly selected patients. Most adverse effects observed during clinical trials have been mild and reversible.
- Table 1 lists the adverse reactions reported from 4 controlled studies conducted in the United States involving once-a-day administration of penbutolol (at doses ranging from 10 to 120 mg) as monotherapy or in combination with hydrochlorothiazide. Penbutolol doses above 40 mg/day are not, however, recommended. The table includes only those events where the prevalence rate in the penbutolol group was at least 1.5%, or where the reaction is of particular interest.
Over a dose range from 10 to 40 mg, once a day, fatigue, nausea, and sexual impotence occurred at a greater frequency as the dose was increased.
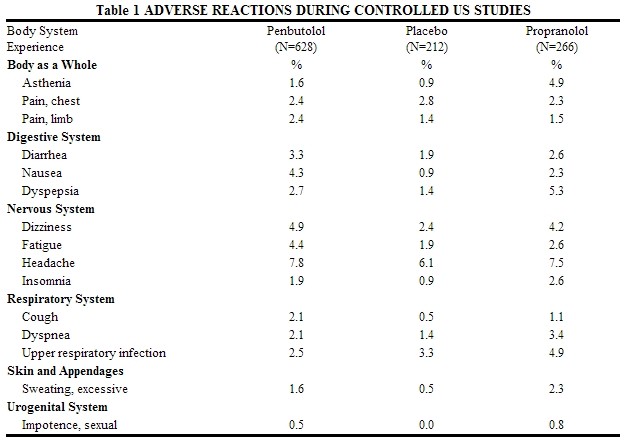
- In a double-blind clinical trial comparing In a double-blind clinical trial comparing penbutolol (40 mg and greater once a day) and propranolol (40 mg or more twice a day), heart rates of less than 60 beats/min. were recorded at least once in 25% of the patients in the group receiving penbutolol and in 37% of the patients in the propranolol group. Corresponding figures for heart rates of less than 50 beats/min. were 1.2% and 6% respectively. No symptoms associated with bradycardia were reported.
- Discontinuations of penbutolol because of adverse reactions have ranged between 2.4% and 6.9% of patients in double-blind, parallel, controlled clinical trials, as compared to 1.8% to 4.1% in the corresponding control groups that were given placebo. The frequency and severity of adverse reactions have not increased during long-term administration of penbutolol. The prevalence of adverse reactions reported from 4 controlled clinical trials (referred to in the table above) as reasons for discontinuation of therapy by>0.5% of the penbutolol group is listed in the table below.

Potential Adverse Effects
- In addition, certain adverse effects not listed above have been reported with other ß-blocking agents and should also be considered as potential adverse effects of penbutolol.
- Central Nervous System: Reversible mental depression progressing tocatatonia (an acute syndrome characterized by disorientation for time and place), short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance (neuropsychometrics).
- Cardiovascular: Intensification of AV block.
- Allergic: Erythematous rash, fever combined with aching and sore throat, laryngospasm, and respiratory distress.
- Hematologic: Agranulocytosis, nonthrombocytopenic and thrombocytopenic purpura.
- Gastrointestinal: Mesenteric arterial thrombosis and ischemic colitis.
- Miscellaneous: Reversible alopecia and Peyronie’s disease. The oculomucocutaneous syndrome associated with the ß-blocker practolol has not been reported with penbutolol during investigational use and extensive foreign clinical experience.
Postmarketing Experience
There is limited information regarding Penbutolol Postmarketing Experience in the drug label.
Drug Interactions
- Penbutalol has been used in combination with hydrochlorothiazide in at least 100 patients without unexpected adverse reactions.
- Penbutolol increases the volume of distribution of lidocaine in normal subjects. This could result in a requirement for higher loading doses of lidocaine.
- Cimetidine has no effect on the clearance of penbutolol. The major metabolite of penbutolol is a glucuronide, and it has been shown that cimetidine does not inhibit glucuronidation.
- Synergistic hypotensive effects, bradycardia, and arrhythmias have been reported in some patients receiving ß-adrenergic blocking agents when an oral calcium antagonist was added to the treatment regimen.
- Generally, penbutatol should not be used in patients receiving catecholamine-depleting drugs.
- Digoxin: Both digitalis glycosides and beta-blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia.
- Anesthesia: Care should be taken when using anesthetic agents that depress the myocardium, such as ether, cyclopropane, and trichloroethylene, and it is prudent to use the lowest possible dose of penbutolol. Penbutolol, like other beta-blockers, is a competitive inhibitor of beta-receptor agonists, and its effect on the heart can be reversed by cautious administration of such agents (eg, dobutamine or isoproterenol). Manifestations of excessive vagal tone (eg, profound bradycardia, hypotension) may be corrected with atropine 1 to 3 mg IV in divided doses.
Use in Specific Populations
Pregnancy
Teratogenic Effects
- Teratology studies in rats and rabbits revealed no teratogenic effects related to treatment with penbutolol at oral doses up to 200 mg/kg/day (250 times the MRHD). In rabbits, a slight increase in the intrauterine fetal mortality and a reduced 24-hour offspring survival rate were observed in the groups treated with 125 mg/kg/day (156 times the MRHD) but not in the groups treated with 0.2 and 5 mg (0.25 to 6 times the MRHD).
- There are no adequate and well-controlled studies in pregnant women. Penbutatol should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
- In a perinatal and postnatal study in rats, the pup body weight and pup survival rate were reduced at the highest dose level of 160 mg/kg/day (200 times the MRHD).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Penbutolol in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Penbutolol during labor and delivery.
Nursing Mothers
- It is not known whether penbutatol is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when penbutatol is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness of penbutatol in pediatric patients have not been established.
Geriatic Use
- Clinical studies of penbutatol did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
- This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Penbutolol with respect to specific gender populations.
Race
There is no FDA guidance on the use of Penbutolol with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Penbutolol in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Penbutolol in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Penbutolol in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Penbutolol in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
- There is limited information regarding Monitoring of Penbutolol in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Penbutolol and IV administrations.
Overdosage
- There is no actual experience with penbutatol overdose. The signs and symptoms that would be expected with overdosage of beeta-adrenergic receptor antagonists are symptomatic bradycardia, hypotension, bronchospasm, and acute cardiac failure. In addition to discontinuation of penbutatol, gastric emptying, and close observation of the patient, the following measures might be considered as appropriate:
- Excessive bradycardia: Administer atropine sulfate to induce vagal blockade. If bradycardia persists, intravenous isoproterenol hydrochloride may be administered cautiously; larger than usual doses may be needed. In refractory cases, the use of a transvenous cardiac pacemaker may be necessary.
- Hypotension: Sympathomimetic drug therapy, such as dopamine, dobutamine, or levarterenol, may be considered if hypotension persists despite correction of bradycardia. In refractory cases, administration of glucagon hydrochloride has been reported to be useful.
- Bronchospasm: A beta-2-agonist or Isoproterenol hydrochloride may be administered. Additional therapy with aminophylline may be considered.
- Acute Cardiac Failure: Institute conventional therapy immediately. Intravenous administration of dobutamine and glucagon hydrochloride has been reported to be useful.
- Heart Block (Second or Third Degree): Isoproterenol hydrochloride or a transvenous cardiac pacemaker may be used.
Pharmacology
| |
Penbutolol
| |
| Systematic (IUPAC) name | |
| (S)-1-(tert-butylamino)-3-(2-cyclopentylphenoxy)propan-2-ol | |
| Identifiers | |
| CAS number | |
| ATC code | C07 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 291.428 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
- The mechanisms of the antihypertensive actions of beta-receptor antagonists have not been established. However, factors that may be involved are:
- Competitive antagonism of catecholamines at peripheral adrenergic receptor sites (especially cardiac) that leads to decreased cardiac output.
- A central nervous system (CNS) action that results in a decrease in tonic sympathetic neural outflow to the periphery.
- A reduction of renin secretion through blockade of beta-receptors involved in release of renin from the kidneys.
Structure
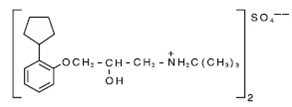
- Penbutolol sulfate is a synthetic beta-receptor antagonist for oral administration. The chemical name of penbutolol sulfate is (S)-1-tert-butylamino-3-(o-cyclopentylphenoxy)-2-propanol sulfate. It is provided as the levorotatory isomer. The empirical formula for penbutolol sulfate is C36H60N2O8S. Its molecular weight is 680.94. A dose of 20 mg is equivalent to 29.4 µmol. The structural formula is as follows:
- Penbutolol is a white, odorless, crystalline powder. Penbutatol is available as tablets for oral administration. Each tablet contains 20 mg of penbutolol sulfate. It also contains corn starch, D&C Yellow No. 10, lactose, magnesium stearate, povidone, silicon dioxide, talc, titanium dioxide, synthetic black iron oxide, hypromellose, simethicone and other inactive ingredients.
Pharmacodynamics
- Penbutolol is a beta-1, beta-2 (nonselective) adrenergic receptor antagonist. Experimental studies showed a dose-dependent increase in heart rate in reserpinized (norepinephrine-depleted) rats given penbutolol intravenously at doses of 0.25 to 1.0 mg/kg, suggesting that penbutolol has some intrinsic sympathomimetic activity. In human studies, however, heart rate decreases have been similar to those seen with propranolol.
- Penbutolol antagonizes the heart rate effects of exercise and infused isoproterenol. The beta-blocking potency of penbutolol is approximately 4 times that of propranolol. An oral dose of less than 10 mg will reduce exercise-induced tachycardia to one-half its usual level; maximum antagonism follows doses of 10 to 20 mg. The peak effect is between 1.5 and 3 hours after oral administration. The duration of effect exceeds 20 hours during a once-daily dosing regimen. During chronic administration of penbutolol, the duration of antihypertensive effects permits a once-daily dosage schedule.
- Acute hemodynamic effects of penbutolol have been studied following single intravenous doses between 0.1 and 4 mg. The cardiovascular responses included significant reductions in heart rate, left ventricular maximum dP/dt, cardiac output, stroke volume index, stroke work, and stroke work index. Systolic blood pressure and mean arterial pressure were reduced, and total peripheral resistance was increased.
- Chronic administration of penbutolol to hypertensive patients results in the hemodynamic pattern typical of beta-adrenergic blocking drugs: a reduction in cardiac index, heart rate, systolic blood pressure and diastolic blood pressure, and the product of heart rate and mean arterial pressure both at rest and with all levels of exercise, without significant change in total peripheral resistance. Penbutolol causes a reduction in left ventricular contractility. Penbutolol decreases glomerular filtration rate, but not significantly.
- Clinical trial doses of 10 to 80 mg per day in single daily doses have reduced supine and standing systolic blood pressures and diastolic blood pressure. In most studies, effects were small, generally a change in blood pressure 5 to 8/3 to 5 mm Hg greater than seen with a placebo measured 24 hours after dosing. It is not clear whether this relatively small effect reflects a characteristic of penbutolol or the particular population studied (the population had relatively mild hypertension but did not appear unusual in other respects). In a direct comparison of penbutolol with adequate doses of twice daily propranolol, no difference in blood pressure effect was seen. In a comparison of placebo and 10-, 20-, and 40-mg single daily doses of penbutolol, no significant dose-related difference was seen in response to active drug at 6 weeks, but, compared to the 10-mg dose, the two larger doses showed greater effects at 2 and 4 weeks and reached their maximum effect at 2 weeks. In several studies, dose increases from 40 to 80 mg were without additional effect on blood pressure. Response rates to penbutolol are unaffected by sex or age but are greater in caucasians than blacks.
- Penbutolol decreases plasma renin activity in normal subjects and in patients with essential and renovascular hypertension.
- Penbutolol dose dependently increases the RR and QT intervals. There is no influence on the PR]], QRS, or QT c (corrected) intervals.
Pharmacokinetics
- Following oral administration, penbutolol is rapidly and completely absorbed. Peak plasma concentrations of penbutolol occur between 2 and 3 hours after oral administration and are proportional to single and multiple doses between 10 and 40 mg once a day. The average plasma elimination half-life of penbutolol is approximately 5 hours in normal subjects. There is no significant difference in the plasma half-life of penbutolol in healthy elderly persons or patients on renal dialysis. Twelve to 24 hours after oral administration of doses up to 120 mg, plasma concentrations of parent drug are 0% to 10% of the peak level. No accumulation of penbutolol is observed in hypertensive patients after 8 days of therapy at doses of 40 mg daily or 20 mg twice a day. Penbutolol is approximately 80% to 98% bound to plasma proteins.
- The metabolism of penbutolol in humans involves conjugation and oxidation. The metabolites are excreted principally in the urine. When radiolabeled penbutolol was administered to humans, approximately 90% of the radioactivity was excreted in the urine. Approximately 1/6 of the dose of penbutolol was recovered as penbutolol conjugate while the remaining fraction was not identified. Conjugated penbutolol has a plasma elimination half-life of approximately 20 hours in healthy persons, 25 hours in healthy elderly persons, and 100 hours in patients on renal dialysis. Thus, accumulation of penbutolol conjugate may be expected upon multiple-dosing in renal insufficiency. An oxidative metabolite of penbutolol, 4-hydroxy penbutolol, has been identified in small quantities in plasma and urine. It is 1/8 to 1/15 times as active as the parent compound in blocking isoproterenol-induced ß-adrenergic receptor responses in isolated guinea-pig trachea and is 1/8 to 1 times as potent in anesthetized dogs.
Nonclinical Toxicology
- Studies in rats indicated that the combination of penbutolol, triamterene, and hydrochlorothiazide (up to 40, 50 and 25 mg/kg respectively) increased the incidence and severity of renal tubular dilation and regeneration when compared to that in rats treated only with triamterene and hydrochlorothiazide. Dogs administered the same doses of triamterene and hydrochlorothiazide alone and in combination with penbutolol had an increase in serum alkaline phosphatase and serum alanine transferase, but there were no gross or microscopic abnormalities observed. No significant toxicologic findings were observed in rats and dogs treated with a combination of penbutolol and hydrochlorothiazide.
Clinical Studies
- Clinical trial doses of 10 to 80 mg per day in single daily doses have reduced supine and standing systolic blood pressures and diastolic blood pressure. In most studies, effects were small, generally a change in blood pressure 5 to 8/3 to 5 mm Hg greater than seen with a placebo measured 24 hours after dosing. It is not clear whether this relatively small effect reflects a characteristic of penbutolol or the particular population studied (the population had relatively mild hypertension but did not appear unusual in other respects). In a direct comparison of penbutolol with adequate doses of twice daily propranolol, no difference in blood pressure effect was seen. In a comparison of placebo and 10-, 20-, and 40-mg single daily doses of penbutolol, no significant dose-related difference was seen in response to active drug at 6 weeks, but, compared to the 10-mg dose, the two larger doses showed greater effects at 2 and 4 weeks and reached their maximum effect at 2 weeks. In several studies, dose increases from 40 to 80 mg were without additional effect on blood pressure. Response rates to penbutolol are unaffected by sex or age but are greater in caucasians than blacks.
How Supplied
- Penbutolol sulfate 20 mg tablets are capsule-shaped, film-coated, yellow tablets scored on both sides and imprinted in black with “SP 22” on one side. They are supplied as follows: Bottles of 100 (NDC 52244-450-10)
Storage
- Store at 20°-25°C (68°-77°F); excursions permitted between 15°-30°C (59°-86°F).
- Keep tightly closed and protect from light.
Images
Drug Images
{{#ask: Page Name::Penbutolol |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Penbutolol |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
(Patient Counseling Information)
Precautions with Alcohol
- In one study, the combination of penbutolol and alcohol increased the number of errors in the eye-hand psychomotor function test.
Brand Names
- Levatol
Look-Alike Drug Names
There is limited information regarding Penbutolol Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Bowles MJ, Khurmi NS, Bala Subramanian V, Raftery EB (1984). "Efficacy of once daily penbutolol in chronic stable angina. An objective comparison with long-acting propranolol". Int J Cardiol. 5 (2): 131–42. PMID 6365803.