Opioid overdose
| Resident Survival Guide |
|
Opioid Microchapters |
|
Opioid overdose On the Web |
|---|
|
American Roentgen Ray Society Images of Opioid overdose |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vidit Bhargava, M.B.B.S [2]; Kiran Singh, M.D. [3]
Synonyms and keywords: Opioid intoxication
| Opioid overdose | |
| Classification and external resources | |
| ICD-10 | F11.0, T40.0-T40.2 |
|---|---|
| ICD-9 | 305.5, 965.0 |
Overview
An opioid overdose is an acute condition due to excessive use of narcotics. It should not be confused with opioid dependency. Prescription opioid overdose was responsible for more deaths in the United States from 1999-2008 than heroin or cocaine overdose combined.[1] Heroin overdose in a number of cases, can occur accidentally in a group of people called as 'body packers' and 'body stuffers'. Body packers swallow bags of heroin, to hide them in their gastrointestinal tract. While body stuffers, usually stuff their rectum or vagina with bags of heroin in an attempt to illegally smuggle them into a country. Since these bags are not specially designed to store drug in the body, there are chances that they might actually rupture leading to accidental poisoning/overdose.[2][3][4][5]
Epidemiology and Demographics
As per recent Center for disease control (CDC) data, it accounts for the largest percentage of substance abuse deaths in prescription drug category. Of the 22,134 deaths relating to prescription drug overdose in 2010, 16,651 (75%) involved opioid analgesics (also called opioid pain relievers or prescription painkillers), and 6,497 (30%) involved benzodiazepines.[6] In the year 2011, the most commonly involved drug was cocaine, with 162.1 visits per 100,000 population. This was closely followed by marijuana, which was involved in 146.2 visits per 100,000 population. Other drugs had lower rates: heroin (83.0 visits per 100,000 population), illicit stimulants (predominately amphetamines and methamphetamine; 51.3 visits per 100,000 population), and other illicit drugs (predominately PCP and various hallucinogens; 42.1 visits per 100,000 population).[7]
Commonly Abused Opioids
Although any opioid can by abused for recreational purposes, some of the most common ones are as follows:
For a more detailed description of one of these opioids click on the name.
- Heroin
- Morphine
- Oxycodone/oxycontin
- Buprenorphine
- Dextromethorphan
- Fentanyl
- Hydrocodone
- Meperidine
- Methadone
- Propoxyphene
- Tramadol
Co-Ingestion
Opioid overdoses associated with a conjunction of benzodiazepines or alcohol use leads to a contraindicated condition wherein higher instances of general negative overdose traits native to the overdose profile of opioid use alone but to a much greater extent.[8][9] Other CNS depressants, or "downers", muscle relaxers, pain relievers, anti-convulsants, anxiolytics (anti-anxiety drugs), treatment drugs of a psychoactive or epileptic variety or any other such drug with its active function meant to calm or mitigate neuronal signaling (barbiturates, etc.) can additionally cause a worsened condition with less likelihood of recovery cumulative to each added drug of a diverse or disparate hampering effect to the central or peripheral nervous system of the user. This includes drugs less immediately classed to a slowing of the metabolism such as with GABAergics like GHB or glutamatergic antagonists like PCP or Ketamine.
Differential Diagnosis
| Disease/Condition | Differentiating feature |
|---|---|
| Alcohol intoxication | Altered mental status without miosis and respiratory depression. |
| Sedative hypnotics | Miosis absent. |
| Phencyclidine (PCP) overdose | CNS depression and miosis are present. Nystagmus present and respiratory depression absent. |
| Ketamine overdose | CNS depression and miosis are present. Nystagmus present and respiratory depression absent. |
| Antipsychotic overdose | Hypotension and bradycardia are seen, but other features are absent. |
| Pontine hemorrhage | Miosis present, other features absent. |
| Gammahydroxybutyrate/gammabutyrolactone overdose | Most likely manifests as opioid overdose. Miosis may not be present. |
| Clonidine/imidazolines overdose | Profound bradycardia and hypotension. |
Additionally, none of these have a response to naloxone, as dramatic as in treating opioid overdose.
Mechanism of Death from Overdose
Heroin is a semisynthetic derivative of morphine, that has a high addictive potential. When used intravenously, it is even more potent. Similar to morphine and other analgesic opioids, heroin has mu, kappa, and delta receptor activity. Stimulation of the mu receptors results in analgesia, euphoria, CNS depression, respiratory depression, and miosis.[10]
Opioids can cause respiratory depression, due to their role in reducing brains response to changes in PaCO2 levels and hypoxia. Respiratory arrest is the most common cause of death in cases of opioid overdose. The effect on respiratory depression is more potent for pure agonists such as heroin and morphine, as compared to partial agonists such as burenorphine. It can also cause a mild hypotension by reducing the sympathetic tone in blood vessels, leading to vasodilation and facial flushing. opioids have inhibitory effects on baroreceptors as well as reduces gastric motility, leading further to bradycardia and constipation respectively.[10]
The onset of action, peak effects, and duration of action vary with the different methods of use, as well as the type of opioid used. On injecting, the onset of action is within 1-2 minutes when injected intravenous and within 15-30 minutes when injected intramuscular or snorted. Analgesic effects usually last for 3-5 hours.
Heroin is rapidly converted to 6-monoacetylmorphine (6-MAM) by the liver, brain, heart, and kidneys, which is further converted to morphine. Morphine has a longer half life as compared to heroin. However a small amount of 6-MAM is detectable in urine for a long time, which serves as the basis for its detection in toxicology screens.[11]
Risk Factors For Abuse
Several factors are thought to increase the risk of opioid overdose in a patient abusing these agents. These are described below:[12][13]
Demographic factors: Being a young, single male, without a stable employment is a high risk factor for overdose.
Resuming the behavior after a period of abstinence: The abstinence could be due to voluntary efforts to stop the abuse, medically induced withdrawal or imprisonment resulting in forced abstinence.
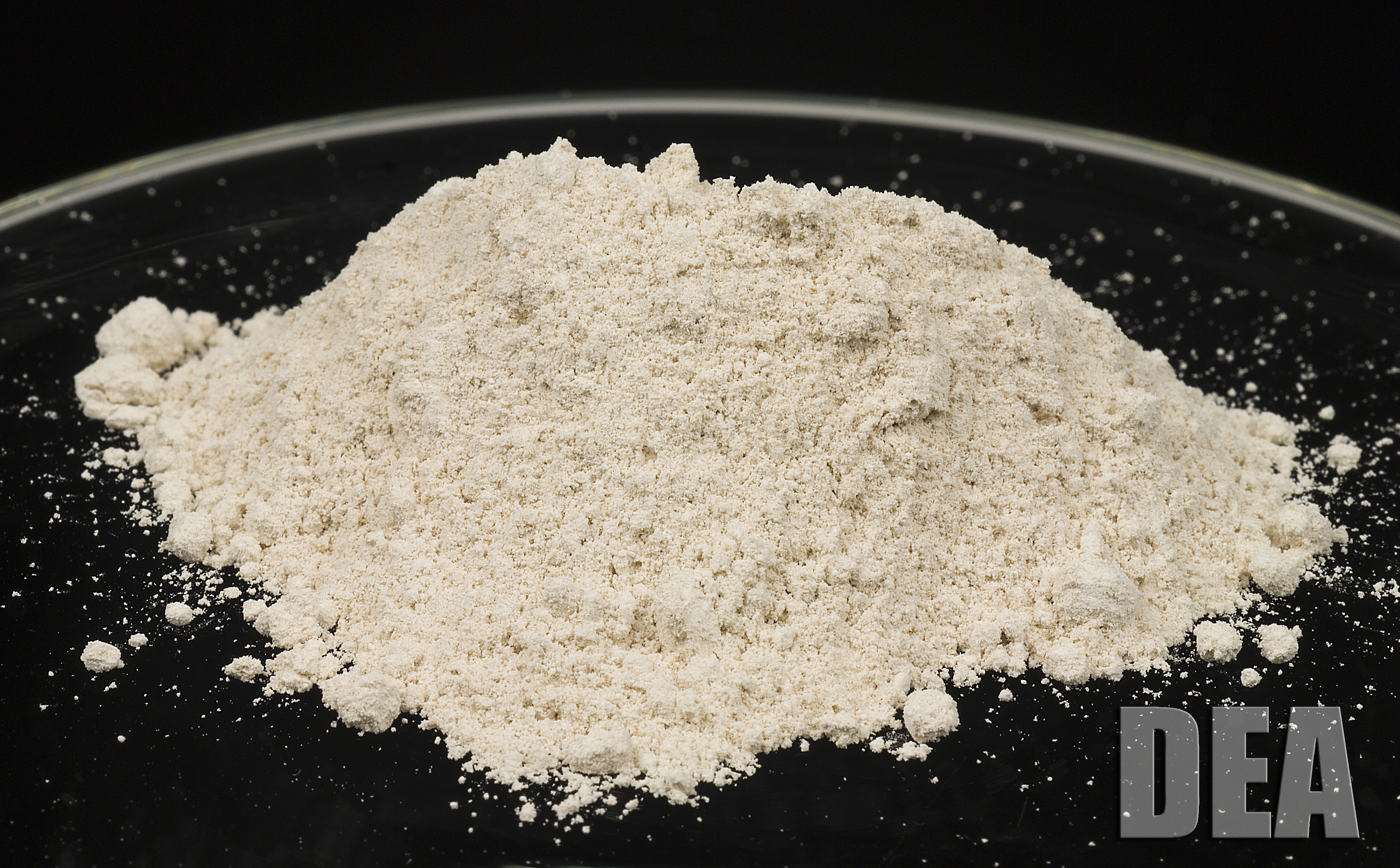
Inconsistency with the quality of the drugs: Most commonly these are sold on streets, the quality being unpredictable & inconsistent. A higher purity sample may cause overdose at doses to which the person was used to before.
Mixing different type of drugs: Mixing drugs that have a brain and respiratory function depressing action similar to opioids, may lead to an overdose even at smaller doses. This may include drugs such as sedative-hypnotic (diazepam, clonazepam, lorazepam etc), H1 antihistaminics such as chlorpheniramine or promethazine or even alcohol. Different drugs will potentiate the effect of opioids differently.[14] [15]
Physical illness or recent infections: During states of metabolic stress, especially when a person is severely ill or dehydrated, even smaller doses may cause overdose.
Mental health: A person suffering from mental illnesses such as depression, schizophrenia or bipolar disorder may use opioid overdose as a means of committing suicide.
Past overdose events: Recent research has shown that people who have overdosed in the past are at much greater risk of future overdose.
Diagnosis
Diagnostic Criteria
DSM-V Diagnostic Criteria for Opioid Intoxication[16]
| “ |
AND
AND
AND
Specify if:
|
” |
Symptoms
Opiate overdose symptoms and signs include: decreased level of consciousness and pinpoint pupils.[17] Heart rate and breathing slow down, sometimes to a stop. Blue lips and nails are caused by insufficient oxygen in the blood. Other symptoms include seizures and muscle spasms. A person experiencing an opiate overdose usually will not wake up even if their name is called or if they are shaken vigorously. The following list summarizes the most commonly experienced symptoms with opioid overdose.[18]
- Airways and lungs
- No breathing
- Shallow breathing
- Slow and difficult breathing
- Eyes, ears, nose, and throat
- Dry mouth
- Miosis (Extremely small pupils 'pinpoint pupils')
- Tongue discoloration
- Heart and blood
- Low blood pressure
- Weak pulse
- Skin
- Bluish-colored nails and lips (cyanosis)
- Compartment syndrome
- Stomach and intestines
- Constipation
- Spasms of the stomach and intestinal tract
- Nervous system
- Renal system
Treatment
Naloxone is very effective at reversing the cause, rather than just the symptoms, of an opioid overdose.[19] A longer-acting variant is naltrexone. Naltrexone is primarily meant to treat opioid and alcohol dependence. Diprenorphine (Revivon) is similar in action to naloxone, only it is significantly stronger and is reserved for acting as an antagonist to the strongest, non-human opioids, such as carfentanyl (in fact, carfentanyl, and other opioids for usage on large animals such as elephants, often come packaged with Revivon to be used after carfentanyl is no longer needed in the animal).
Initial adult dose for patient experiencing respiratory depression is 0.04 mg IV, while the initial pediatric dose is 0.1 mg/Kg IV. If the respiratory rate doesn't increase in next 2-3 minutes a second dose of 0.5 mg is given. If further there is no increase in respiratory rate, following doses can be administered after every 2-3 minutes till an increase in respiratory rate is obtained, 2 mg, 4 mg, 10 mg, 15 mg.
Shown below is a management protocol for treating opioid overdose.[20]
| Opioid overdose: Respiratory rate < 12/min | |||||||||||||||||||||||||||||
| Oxygenate with bag and mask, administer naloxone with a gradually increasing dose till reversal of respiratory depression is seen | |||||||||||||||||||||||||||||
| History of use of morphine, fentanyl or other long acting opioids? | |||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||
| Admit to ICU | Observe for 4-6 hours after last naloxone dose | ||||||||||||||||||||||||||||
| Patient fully awake and alert ? | |||||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||||
| Perform intubation, begin a continuous naloxone infusion | Admit to ICU | ||||||||||||||||||||||||||||
| Continue infusion till respiratory depression reversed, observe 4-6 hours after naloxone infusion is stopped | Discharge patient, when awake & alert with stable vital signs | ||||||||||||||||||||||||||||
Intra-nasal administration: In recent years, there has been an emphasis on studying the efficacy of intra-nasal administration of naloxone, to treat opioid overdose in community. The studies have all converged to the fact that, the efficacy and safety are comparable to other routes of administration, that it is likely to reduce blood exposure in paramedics and can be successfully given even by bystanders.[21] [22] [23]
The U.S. Centers for Disease Control and Prevention (CDC) estimates that US programs for drug users and their caregivers prescribing take-home doses of naloxone and training on its utilization are estimated to have reversed 10,000 opioid overdose deaths.[24][25] Healthcare institution-based naloxone prescription programs have also helped reduce rates of opioid overdose in the US state of North Carolina, and have been replicated in the US military.[26][27] Nevertheless, scale-up of healthcare-based opioid overdose interventions is limited by providers’ insufficient knowledge and negative attitudes towards prescribing take-home naloxone to prevent opioid overdose.[28] Programs training police and fire personnel in opioid overdose response using naloxone have also shown promise in the US.[29][30]
Prevention
Although opioid overdose accounts for the leading cause of accidental death, it can be prevented and often in primary care settings.[31][32] Providers should routinely screen patients using tools such as the CADE-AID and the Drug Abuse Screening Test (DAST-10) to screen adults and the CRAFT to screen adolescents aged 14–18 years.[31] Other “drug seeking” behaviors as well as physical indications of drug use should be used as clues to perform formal screenings.[31] Individuals diagnosed with opioid dependence should be prescribed naloxone to prevent overdose and/or should be directed to one of the many intervention/treatment options available, such as needle exchange programs and treatment centers.[31][32] Brief motivational interviewing can also be performed by the clinician during patient visits and has been shown to improve patient motivation to change their behavior.[31][33] Despite these opportunities, the dissemination of prevention interventions in the US has been hampered by the lack of coordination and sluggish federal government response.[32]
Famous People Death From Overdose
Philip Seymour Hoffman (2014), Anna Nicole Smith (2007), Anna Nicole Smith (1999), River Phoenix (1993), Heath Ledger (2008), Janis Joplin (1970), Corey Haim (2010), Whitney Houston (2012), John Belushi (1982), Chris Farley (1997), Elvis Presley (1977), Judy Garland (1969), Hillel Slovak (1988), Jimi Hendrix (1969), Paula Yates (2000), Billie Holiday (1959), Jim Morrison (1971), Lenny Bruce (1966), Peter Farndon (1983), Kurt Cobain (1994), Dee Dee Ramone (2002), Sid Vicious (1979), Corey Monteith (2013), Chris Kelly (2013), Michael Carl Baze (2011), Derek Boogaard (2011), Erica Blasberg (2010), Andy Irons (2010), Edward Fatu “Umaga” (2009), Billy Mays (2009), Christopher Bowman (2008), Scott Charles (“Bam Bam”) Bigelow (2007), Chris Mainwaring (2007), Ike Turner (2008), Anthony Durante (2003), Howie Epstein (2003), Elisa Bridges (2002), John Entwistle (2002), Darrell Porter (2002), Peter Jackson (1997), David Waymer (1993), Paul Hayward (1992), Chet Baker (1988), David Croudip (1988), Len Bias (1986), Don Rogers (1986), David Kennedy (1984)
Street Names
Heroin
Aunt Hazel, birdie powder, Black, Black Eagle, Black Pearl, Black Stuff, Black Tar, Boy, Brown, Brown Crystal, Brown Rhine, Brown Sugar Junk, Brown Tape, Chiba or Chiva, China White, dog food, Dope White, Dr. Feelgood, Dragon, H, He, hong-yen, Junk, lemonade, Mexican Brown, Mexican Horse, Mexican Mud, Mexican mud, Mud, Number 4, Number 8, old Steve, pangonadalot, Sack, Skag, Skunk Number 3, Smac, Snow, Snowball Scat, Tar, White Boy, White Girl, White Horse, White Lady, White Nurse, White Stuff, witch hazel
| Type of drug combination | Street name |
|---|---|
| Heroin and Marijuana | Atom Bomb, Canade, Woola, Woolie, Woo-Woo |
| Heroin and Cold Medicine | Cheese |
| Heroin and Ecstacy | Chocolate Chip Cookies, H Bomb |
| Heroin and Alprazolam | Bars |
| Heroin and LSD | Beast, LBJ |
| Heroin and Cocaine | Belushi, Boy-Girl, He-She, Dynamite, Goofball, H&C, Primo, Snowball, speedball |
| Heroin and Crack | Chocolate Rock, Dragon Rock, Moonrock |
| Heroin and Ritalin | Pineapple |
Slang Terms for Heroin Use and Abuse
Channel Swimmer, Chasing the Dragon, Daytime (being high), Dip and Dab, Do Up, Evening (coming off the high), Firing the Ack Ack Gun, Give Wings, Jolly Pop, Paper Boy
Codeine
Ac for Robitussin AC, C-plain for Corex Plain, Captain Cody, Cody, Decaprin for Mercodol Decaprin, Deka for Deka Syrup, Drank, Endo for Endotussin, Lean, Lotpurple, Slow, Syrup, Tikoy for Trecodin, Tuss or tussio for Tussionex
Oxycodone/Oxycontin
Blue, Hillbilly Heroin, Kicker, OC, OX, Oxy, Oxycotton, Poor man’s heroin
Morphine
Dreamer, Duramorph, Emma, M, Miss Emma, Monkey, Morph, Roxanol, White stuff
Buprenorphine
Box or Boxes, Bupe, Oranges, Saboxin, Sobos, Stop signs, Stops, Sub or plural Subs
Dextromethorphan
CCC, DXM, Orange crush, Red devils, Robo, Robo-trippin, skittles, Triple C, Tussin
Fentanyl
Apache, Cash., China girl, China white, Dance fever, Friend, Goodfella, Jackpot, Murder 8, Tango, TNT
Hydrocodone
Footballs , Hydros, Pain killer, Percs, Perks, Pinks, Vikes
Meperidine
Demmies, Mapergan, Pethidine
Methadone
Amidone, Dollies, Dolls, Done, Jungle juice, Junk, Maria, Meth, Methadose, Metho, Pastora, Phizzies, Phy, Wafer
References
- ↑ Debono, DJ; Hoeksema, LJ; Hobbs, RD (August 2013). "Caring for Patients with Chronic Pain: Pearls and Pitfalls". Journal of the American Osteopathic Association. 113 (8): 620–627. doi:10.7556/jaoa.2013.023. PMID 23918913.
- ↑ McCarron, MM.; Wood, JD. (1983). "The cocaine 'body packer' syndrome. Diagnosis and treatment". JAMA. 250 (11): 1417–20. PMID 6887463. Unknown parameter
|month=ignored (help) - ↑ Traub, SJ.; Hoffman, RS.; Nelson, LS. (2003). "Body packing--the internal concealment of illicit drugs". N Engl J Med. 349 (26): 2519–26. doi:10.1056/NEJMra022719. PMID 14695412. Unknown parameter
|month=ignored (help) - ↑ Simson, LR. (1976). "Sudden death while attempting to conceal illegal drugs: laryngeal obstruction by a package of heroin". J Forensic Sci. 21 (2): 378–380. PMID 1262836. Unknown parameter
|month=ignored (help) - ↑ Roberts, JR.; Price, D.; Goldfrank, L.; Hartnett, L. (1986). "The bodystuffer syndrome: a clandestine form of drug overdose". Am J Emerg Med. 4 (1): 24–7. PMID 3947429. Unknown parameter
|month=ignored (help) - ↑ "CDC - Facts - Drug Overdose - Home and Recreational Safety - Injury Center". Retrieved 10 February 2014.
- ↑ "http://www.samhsa.gov/data/2k13/DAWN127/sr127-DAWN-highlights.htm". Retrieved 10 February 2014. External link in
|title=(help) - ↑ "BestBets: Concomitant use of benzodiazepines in opiate overdose and the association with a poorer outcome".
- ↑ "BestBets: Concomitant use of alcohol in opiate overdose and the association with a poorer outcome".
- ↑ 10.0 10.1 Snyder, SH.; Pasternak, GW. (2003). "Historical review: Opioid receptors". Trends Pharmacol Sci. 24 (4): 198–205. doi:10.1016/S0165-6147(03)00066-X. PMID 12707007. Unknown parameter
|month=ignored (help) - ↑ "[Japan children's cancer registry and strategy for children's cancer epidemiology]". Gan No Rinsho. 35 (2): 239–47. 1989. PMID 2704133. Unknown parameter
|month=ignored (help) - ↑ "http://www.unodc.org/documents/southasia/publications/sops/opioid-overdose-prevention-and-management-among-injecting-drug-users.pdf" (PDF). Retrieved 10 February 2014. External link in
|title=(help) - ↑ Mathers, BM.; Degenhardt, L.; Phillips, B.; Wiessing, L.; Hickman, M.; Strathdee, SA.; Wodak, A.; Panda, S.; Tyndall, M. (2008). "Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review". Lancet. 372 (9651): 1733–45. doi:10.1016/S0140-6736(08)61311-2. PMID 18817968. Unknown parameter
|month=ignored (help) - ↑ Coffin, PO.; Galea, S.; Ahern, J.; Leon, AC.; Vlahov, D.; Tardiff, K. (2003). "Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990-98". Addiction. 98 (6): 739–47. PMID 12780362. Unknown parameter
|month=ignored (help) - ↑ Darke, S.; Zador, D. (1996). "Fatal heroin 'overdose': a review". Addiction. 91 (12): 1765–72. PMID 8997759. Unknown parameter
|month=ignored (help) - ↑ Diagnostic and statistical manual of mental disorders : DSM-5. Washington, D.C: American Psychiatric Association. 2013. ISBN 0890425558.
- ↑ Chandler, Stephanie. "Symptoms of an opiate overdose". Live Strong. Retrieved 17 May 2012.
- ↑ "Heroin overdose: MedlinePlus Medical Encyclopedia". Retrieved 9 February 2014.
- ↑ Etherington, J; Christenson, J; Innes, G; Grafstein, E; Pennington, S; Spinelli, JJ; Gao, M; Lahiffe, B; Wanger, K (2000). "Is early discharge safe after naloxone reversal of presumed opioid overdose?". CJEM. 2 (3): 156–62. PMID 17621393.
- ↑ Boyer, EW. (2012). "Management of opioid analgesic overdose". N Engl J Med. 367 (2): 146–55. doi:10.1056/NEJMra1202561. PMID 22784117. Unknown parameter
|month=ignored (help) - ↑ Barton, ED.; Ramos, J.; Colwell, C.; Benson, J.; Baily, J.; Dunn, W. "Intranasal administration of naloxone by paramedics". Prehosp Emerg Care. 6 (1): 54–8. PMID 11789651.
- ↑ Robertson, TM.; Hendey, GW.; Stroh, G.; Shalit, M. "Intranasal naloxone is a viable alternative to intravenous naloxone for prehospital narcotic overdose". Prehosp Emerg Care. 13 (4): 512–5. doi:10.1080/10903120903144866. PMID 19731165.
- ↑ Loimer, N.; Hofmann, P.; Chaudhry, HR. (1994). "Nasal administration of naloxone is as effective as the intravenous route in opiate addicts". Int J Addict. 29 (6): 819–27. PMID 8034388. Unknown parameter
|month=ignored (help) - ↑ "OD Prevention Program Locator". Overdose Prevention Alliance. Retrieved 15 May 2012.
- ↑ Centers for Disease Control and Prevention (2012). "Community-Based Opioid Overdose Prevention Programs Providing Naloxone — United States, 2010". Morbidity and Mortality Weekly Report. 61 (6): 101–5. PMID 22337174.
- ↑ Albert, Su; Brason Ii, Fred W.; Sanford, Catherine K.; Dasgupta, Nabarun; Graham, Jim; Lovette, Beth (2011). "Project Lazarus: Community-Based Overdose Prevention in Rural North Carolina". Pain Medicine. 12: S77–85. doi:10.1111/j.1526-4637.2011.01128.x. PMID 21668761.
- ↑ Beletsky, Leo; Burris, Scott C.; Kral, Alex H. (July 21, 2009). "Closing Death's Door: Action Steps to Facilitate Emergency Opioid Drug Overdose Reversal in the United States". SSRN Electronic Journal. doi:10.2139/ssrn.1437163. SSRN 1437163.
- ↑ Beletsky, Leo; Ruthazer, Robin; MacAlino, Grace E.; Rich, Josiah D.; Tan, Litjen; Burris, Scott (2006). "Physicians' Knowledge of and Willingness to Prescribe Naloxone to Reverse Accidental Opiate Overdose: Challenges and Opportunities". Journal of Urban Health. 84 (1): 126–36. doi:10.1007/s11524-006-9120-z. PMC 2078257. PMID 17146712.
- ↑ Beletsky L, Moroz E. "The Quincy Police Department: Pioneering Naloxone Among First Responders". Overdose Prevention Alliance. Retrieved 15 May 2012.
- ↑ Lavoie D. (April 2012). "Naloxone: Drug-Overdose Antidote Is Put In Addicts' Hands". Huffington Post.
- ↑ 31.0 31.1 31.2 31.3 31.4 Bowman S, Eiserman J, Beletsky L, Stancliff S, Bruce RD. (2013). "Reducing the health consequences of opioid addiction in primary care". Am J Med. 126 (7): 565–71. doi:10.1016/j.amjmed.2012.11.031. PMID 23664112.In press
- ↑ 32.0 32.1 32.2 Beletsky L, Rich JD, Walley AY. (2012). "Prevention of Fatal Opioid Overdose". JAMA. 308 (18): 1863–1864. doi:10.1001/jama.2012.14205. PMC 3551246. PMID 23150005.
- ↑ Zahradnik A, Otto C, Crackau B; et al. (2009). "Randomized controlled trial of a brief intervention for problematic prescription drug use in non-treatment-seeking patients". 104 (1): 109–117. doi:10.1111/j.1360-0443.2008.02421.x. PMID 19133895.