Chancroid physical examination
|
Chancroid Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chancroid physical examination On the Web |
|
American Roentgen Ray Society Images of Chancroid physical examination |
|
calculators and risk factors for Chancroid physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yazan Daaboul, M.D.; Nate Michalak, B.A.; Serge Korjian M.D.
Overview
Patients may present with erythematous papules, pustules, or ulcers depending the stage of the chancroid. Ulcers are soft with irregular but sharp margins, and looks similar to a syphilitic chancre. Males typically have 1 ulcer while females typically have multiple. The most common location in males is the foreskin (prepuce). The most common location in females in the labia majora. Approximately 50% of patients may present with swollen inguinal lymph nodes.
Physical Examination
Vital Signs
Typically normal
Skin
A patient may present with either of the following types of lesions on the genitals (or extremities in cases of cutaneous limb ulcers[1][2]), depending on the stage of infection:[3]
Ulcer characteristics:[4]
- Ranges in size from 3 to 50 mm (1/8 to 2 inches) in diameter
- Tender
- Soft, nonindurated
- Irregular border
- Sharp margins
- Grey/yellow exudate
- Males typically have a single ulcer
- Females typically have multiplee ulcers
- May look similar to syphilitic chancre
Common locations in males
- Foreskin (prepuce) (most common)[5]
- Groove behind the head of the penis (coronal sulcus)
- Shaft of the penis
- Head of the penis (glans penis)
- Opening of the penis (urethral meatus)
- Scrotum (least common)
Common locations in females
- Labia majora (most common). "Kissing ulcers" may develop, defined as ulcers that occur on opposing surfaces of the labia.[5]
- Labia minora
- Perineal area
- Inner thighs (least common)
Other Signs
- Tender inguinal lymphadenitis in approximately 50% of patients, known as buboes (typically unilateral and predominantly in males)[6]
- Approximately 25% of patients with lymphadenopathy may present with abscesses in lymph nodes or ruptured buboes
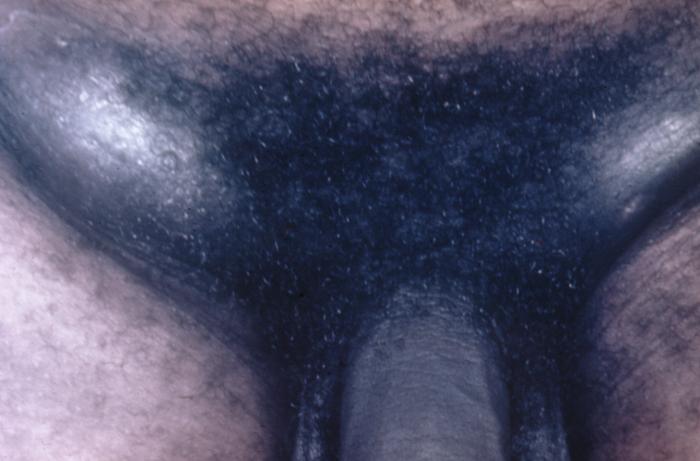
Gallery
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid. Adapted from Dermatology Atlas.[7]
-
Chancroid infection has spread to the inguinal lymph nodes, which have enlarged forming buboes.
-
Penile chancroid lesion.
References
- ↑ Marks M, Chi KH, Vahi V, Pillay A, Sokana O, Pavluck A; et al. (2014). "Haemophilus ducreyi associated with skin ulcers among children, Solomon Islands". Emerg Infect Dis. 20 (10): 1705–7. doi:10.3201/eid2010.140573. PMC 4193279. PMID 25271477.
- ↑ Gaston JR, Roberts SA, Humphreys TL (2015). "Molecular phylogenetic analysis of non-sexually transmitted strains of Haemophilus ducreyi". PLoS One. 10 (3): e0118613. doi:10.1371/journal.pone.0118613. PMC 4361675. PMID 25774793.
- ↑ Spinola, S. M. (2002). "Immunopathogenesis of Haemophilus ducreyi Infection (Chancroid)". Infection and Immunity. 70 (4): 1667–1676. doi:10.1128/IAI.70.4.1667-1676.2002. ISSN 0019-9567.
- ↑ Chancroid. Wikipedia (July 16, 2015). https://en.wikipedia.org/wiki/Chancroid Accessed January 15, 2016.
- ↑ 5.0 5.1 Chancroid. MedlinePlus (January 13, 2016). https://www.nlm.nih.gov/medlineplus/ency/article/000635.htm Accessed January 21, 2016.
- ↑ Lewis, D A (2003). "Chancroid: clinical manifestations, diagnosis, and management". Sexually Transmitted Infections. 79 (1): 68–71. doi:10.1136/sti.79.1.68. ISSN 1368-4973.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 "Dermatology Atlas".
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/6/6f/Chancroid01.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/c/c1/Chancroid02.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/1/1a/Chancroid03.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/7/70/Chancroid04.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/2/22/Chancroid05.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/d/d6/Chancroid06.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/1/19/Chancroid07.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/6/60/Chancroid08.jpg)
![Chancroid. Adapted from Dermatology Atlas.[7]](/images/4/4b/Chancroid09.jpg)