Bag-Valve-Mask Ventilation
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Umar Ahmad, M.D.[2]
Synonyms and keywords: BVM; ambu bag
Overview
A bag valve mask is a hand-held device used to provide ventilation to a patient who is not breathing or who is breathing inadequately. The device is a normal part of a resuscitation kit for trained professionals, such as emergency medical technicians. The BVM is frequently used in hospitals, and is an essential part of a crash cart. The device is used extensively in the operating room to ventilate an anesthetized patient in the minutes before an electric ventilator is attached. The device is self-filling with air, although additional oxygen (O2) can be added.
Use of the BVM to ventilate a patient is frequently called "bagging" the patient.[1] Bagging is regularly necessary in medical emergencies when the patient's breathing is insufficient (respiratory failure) or has ceased completely (respiratory arrest). The BVM resuscitator is used in order to manually provide mechanical ventilation in preference to mouth-to-mouth resuscitation (either direct or through an adjunct such as a pocket mask.
Components
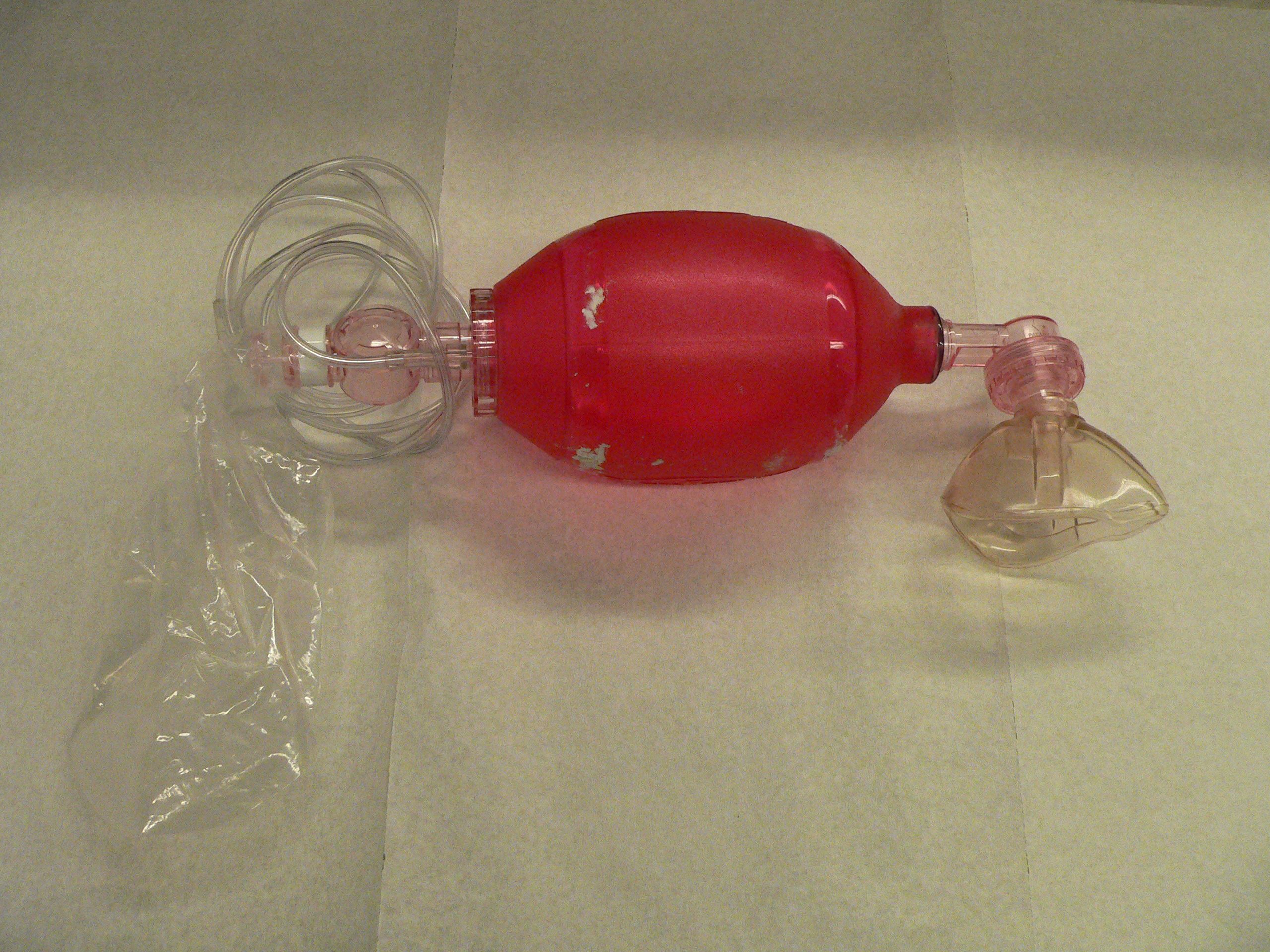
The BVM consists of a flexible air chamber, about the size of an American football, attached to a face mask via a shutter valve. When the air chamber or "bag" is squeezed, the device forces air into the patient's lungs; when the bag is released, it self-inflates, drawing in ambient air or oxygen supplied from a tank. A bag valve mask can be used without being attached to an oxygen tank to provide air to the patient, but supplemental oxygen is recommended since it increases the amount of oxygen reaching the patient. Some devices also have a reservoir which can fill with oxygen while the patient is exhaling (a process which happens passively), in order to increase the amount of oxygen that can be delivered to the patient by about twofold.[1] A BVM should have a valve which prevents the patient from rebreathing exhaled air and which can connect to tubing to allow oxygen to be provided through the mask.
Bag valve masks come in different sizes to fit infants, children, and adults. Some types of the device are disposable, while others are designed to be cleaned, disinfected, and reused.[1]
-
One type of bag valve mask. The part labelled 1 is a flexible mask designed to seal to the patient's face, and the part labelled 3 is a self-filling bag.
-
Different types of bag valve masks.
Use
The BVM directs the gas inside it via a one-way valve when compressed by a rescuer; the gas is then delivered through a mask and into the patient's trachea and into the lungs. In order to be effective, a bag valve mask must deliver between 700 and 1000 milliliters of air to the patient's lungs, but if oxygen is provided through the tubing and if the patient's chest rises with each inhalation (indicating that adequate amounts of air are reaching the lungs), 400 to 600 ml may still be adequate.[1] Squeezing the bag once every 5 seconds for an adult or once every 3 seconds for an infant or child provides an adequate respiratory rate (12 respirations per minute in an adult and 20 per minute in a child or infant).[2]
Professional rescuers are taught to ensure that the mask portion of the BVM is properly sealed around the patient's face (that is, to ensure proper "mask seal"); otherwise, air escapes from the mask and is not pushed into the lungs. In order to maintain this protocol, some protocols use a method of ventilation involving two rescuers: one rescuer to hold the mask to the patient's face with both hands and ensure a mask seal, while the other squeezes the bag.[3] However, as most ambulances have only two members of crew, the other crew member is likely to be doing compressions in the case of CPR, or may be performing other skills such as cannulation. In this case, or if no other options are available, the BVM can also be operated by a single rescuer who holds the mask to the patient's face with one hand, in the anaesthetists grip, and squeezes the bag with the other.
When using a BVM, as with other methods of insufflation, there is a risk of overinflating the lungs. This can lead to pressure damage to the lungs themselves, and can also cause air to enter the stomach, causing gastric distention which can make it more difficult to inflate the lungs and which can cause the patient to vomit. This can be avoided by care on behalf of the rescuer. Alternatively, some models of BVM are fitted with a valve which prevents overinflation, by blocking the outlet pipe when a certain pressure is reached.
An endotracheal tube (ETT) can be inserted by a trained practitioner and can substitute for the mask portion of the BVM. This provides a more secure fit and is easier to manage during emergency transport, since the ET tube is sealed with an inflatable cuff in the trachea, so that any regurgitation cannot enter the lungs. Such material can severely damage the lung tissue, and in the absence of an ET tube, could choke the patient by obstructing the airway. Inhalation of stomach contents can be fatal; the after effects can cause Mendelson's syndrome or aspiration pneumonia.
Some rescuers may also choose to use a different form of resuscitation adjunt, such as an oropharyngeal airway or Laryngeal mask airway, which would be inserted and then used with the BVM.
In a hospital, long-term mechanical ventilation is provided by using more complex devices such as an intensive care ventilator, rather than by a BVM, which requires at least one person to operate it constantly.
A flow-restricted, oxygen-powered ventilation device (FROPVD) is similar to a BVM in that oxygen is pushed through a mask into the patient's lungs, but unlike a BVM, in the FROPVD the pressure needed to push air into the patient's lungs is generated by oxygen from a tank rather than by squeezing a bag.
Ambu bag
One proprietary brand of a self-inflating BVM resuscitator, is called the ambu bag. The concept for the original ambu bag was developed in 1953 by the German engineer, Dr. Holger Hesse, and his partner, Danish anesthesialogist, Henning Ruben. In 1956, the world's first non-electric, self-inflating resuscitator was ready for production by their company, Ambu A/S, which still produces a wide range of single-patient and multi-use resuscitators.
Related Chapters
References

