Achilles tendon rupture
| Achilles tendon rupture | |
 | |
|---|---|
| MRI: STIR: Achilles tendon rupture (Image courtesy of RadsWiki) | |
| ICD-10 | S86.0 |
| eMedicine | sports/1 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Kiran Singh, M.D. [2]
Overview
Achilles tendon rupture is the most common injury involving a break in a tendon. It commonly occurs as a sports injury during explosive acceleration e.g. pushing off or jumping up.
History and Symptoms
Symptoms
- Acute pain
- Difficulty walking
- Referred stabbing pain in the posterior leg and ankle from muscle spasm[1]
Diagnosis
Diagnosis is made by clinical history; typically people say it feels like being kicked or shot behind the ankle. Upon examination a gap may be felt just above the heel unless swelling has filled the gap and the Simmonds' test (aka Thompson test) will be positive; squeezing the calf muscles of the affected side while the patient lies prone, face down, with his feet hanging loose results in no movement (no passive planter flexion) of the foot, while movement is expected with an intact Achilles tendon and should be observable upon manipulation of the uninvolved calf.
An O'Brien test can also be performed which entails placing a sterile needle through the skin and into the tendon. If the needle hub moves in the opposite direction of the tendon and the same direction as the toes when the foot is moved up and down then the tendon is at least partially intact.
MRI
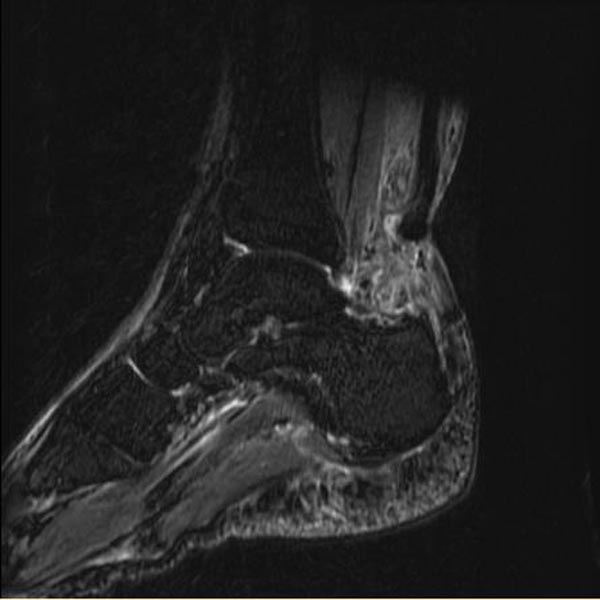
-
STIR: MRI; Achilles tendon rupture
-
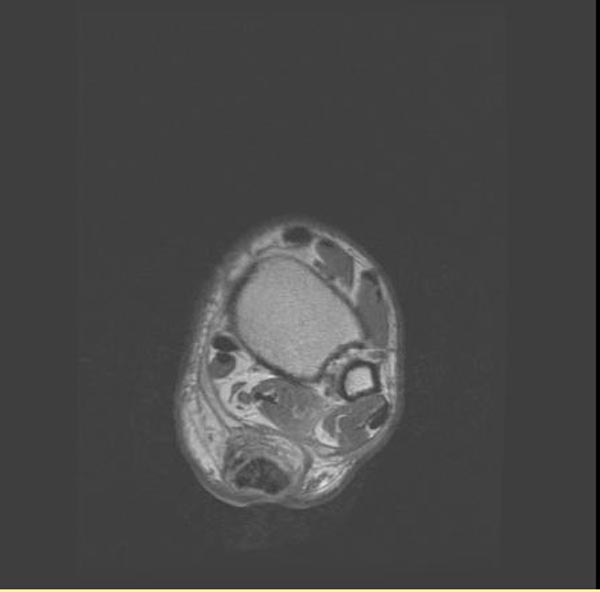
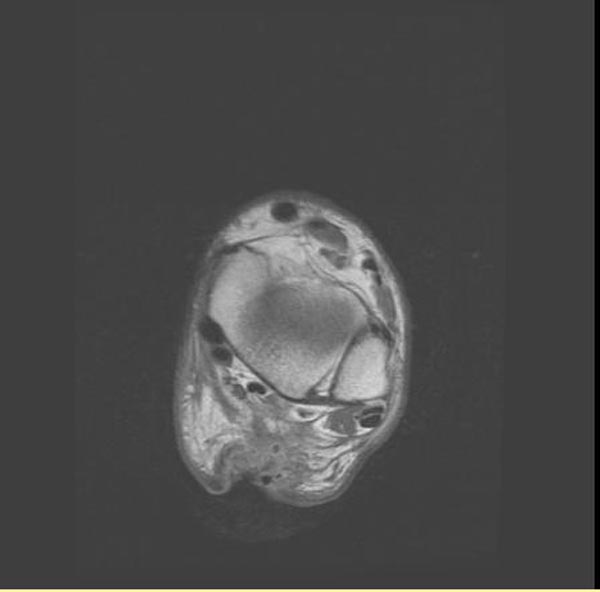
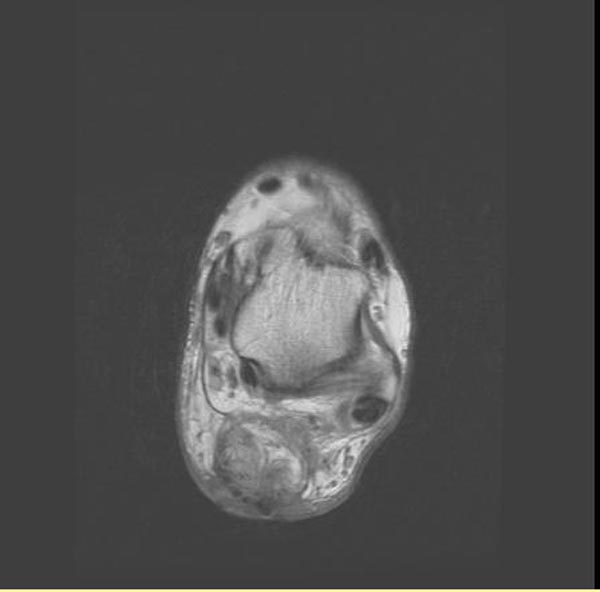
Proton density: MRI; Achilles tendon rupture
-
Proton density: MRI; Achilles tendon rupture
-
Proton density: MRI; Achilles tendon rupture
-
Proton density: MRI; Achilles tendon rupture
Sometimes an ultrasound scan may be required to clarify or confirm the diagnosis. MRI can also be used to confirm the diagnosis.
Risk factors
Most cases of Achilles tendon rupture are traumatic sports injuries. The average age of patients is 30-40 years with a male-to-female ratio of nearly 20:1. Fluoroquinolone antibiotics, such as ciprofloxacin, and glucocorticoids have been linked with an increased risk of Achilles tendon rupture. Direct steroid injections into the tendon have also been linked to rupture.
Treatment
Treatment remains divided between operative and non-operative management. Non-operative management traditionally consisted of restriction in an "equinus" plaster cast for six to eight weeks with the foot pointed downwards (to oppose the ends of the ruptured tendon).
Some surgeons feel an early surgical repair of the tendon is beneficial. The surgical option offers a significantly smaller risk of re-rupture compared to traditional non-operative management (5% vs 15%).[2] However surgery imposes much higher relative risks of perioperative mortality and morbidity e.g. infection including MRSA, bleeding, deep vein thrombosis, lingering anesthesia effects, etc.
References
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Richter J, Josten C, Dàvid A, Clasbrummel B, Muhr G (1994). "[Sports fitness after functional conservative versus surgical treatment of acute Achilles tendon ruptures]". Zentralbl Chir (in German). 119 (8): 538–44. PMID 7975942.
External links
- "Achilles tendon rupture". Mayo Clinic. Sep 26, 2007. Unknown parameter
|axxessdate=ignored (help)