Wolff-Parkinson-White syndrome resident survival guide: Difference between revisions
Rim Halaby (talk | contribs) No edit summary |
|||
| (221 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}}; {{AE}} {{Hilda}}; | {{CMG}}; {{AE}} {{Alonso}}; {{Hilda}}; {{AL}} | ||
<div style="width: | <div style="width: 90%;"> | ||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | {| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | ||
| Line 12: | Line 12: | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Causes|Causes]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Causes|Causes]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide# | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide# | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagstic Approach|Diagsis]] | ||
:[[Wolff-Parkinson-White syndrome resident survival guide# | |- | ||
:[[Wolff-Parkinson-White syndrome resident survival guide#Wolff-Parkinson-White syndrome | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Treatment|Treatment]] | ||
: [[Wolff-Parkinson-White syndrome resident survival guide#Initial Treatment|Initial]] | |||
: [[Wolff-Parkinson-White syndrome resident survival guide#Long-Term Treatment|Long-term]] | |||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Do's|Do's]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Wolff-Parkinson-White syndrome resident survival guide#Do's|Do's]] | ||
| Line 23: | Line 25: | ||
|} | |} | ||
== Overview== | ==Overview== | ||
[[Wolff-Parkinson-White | [[Wolff-Parkinson-White]] (WPW) [[syndrome]] is a condition of [[pre-excitation]] of the [[Ventricle (heart)|ventricles]] of the [[heart]] due to the presence of an [[accessory pathway]] known as the [[Bundle of Kent]] through which the electrical impulses bypass the [[AV node]]. The difference between [[WPW]] pattern and [[WPW]] [[syndrome]] is that [[WPW]] pattern is characterized by the presence of characteristic [[ECG]] findings, such as a short [[PR interval]] and a [[delta wave]], whereas [[WPW]] [[syndrome]] is the occurrence of [[tachycardia]] with or without associated [[symptoms]] in a subject with existing [[WPW]] pattern.<ref>{{Cite web | last = | first = | title = Wolff-Parkinson-White Syndrome and Accessory Pathways | url = http://circ.ahajournals.org/content/122/15/e480.full | publisher = | date = | accessdate = 1 April 2014 }}</ref> The treatment of [[WPW]] [[syndrome]] is targeted towards the restoration of the [[sinus rhythm]], usually by the administration of either [[ibutilide]] or [[procainamide]]. The most common type of [[arrhythmia]] in [[WPW syndrome]] is [[AV reentrant tachycardia]].<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> [[Atrial fibrillation]] in a patient with [[WPW]] is life threatening and should be managed urgently. [[Atrial fibrillation]] in a patient with [[WPW]] should be suspected when there is [[ECG]] findings suggestive of [[atrial fibrillation]] in the context of a [[heart rate]] higher than 220 [[beats per minute]]. | ||
==Causes== | ==Causes== | ||
| Line 30: | Line 32: | ||
[[Wolff-Parkinson-White syndrome]] can be a life-threatening condition and must be treated as such irrespective of the underlying cause. | [[Wolff-Parkinson-White syndrome]] can be a life-threatening condition and must be treated as such irrespective of the underlying cause. | ||
*[[ | ===Common Causes=== | ||
* [[Congenital]] | |||
==FIRE: Focused Initial Rapid Evaluation== | |||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref><ref name="ACLS">{{Cite web | last = | first = | title = Part 8: Adult Advanced Cardiovascular Life Support | url = http://circ.ahajournals.org/content/122/18_suppl_3/S729.full | publisher = | date = | accessdate = 3 April 2014 }}</ref> <br> <span style="font-size:85%">Boxes in red signify that an urgent management is needed.</span> | |||
<span style="font-size:85%"> '''Abbreviations:''' '''AF:''' [[atrial fibrillation]]; '''AVRT''': [[AV reentrant tachycardia]]; '''BP:''' [[blood pressure]]; '''ECG:''' [[electrocardiography]]; '''HF:''' [[heart failure]]; '''LVH:''' [[left ventricular hypertrophy]]; '''WPW:''' [[WPW|Wolff-Parkinson-White pattern]]</span> | |||
{{Family tree/start}} | |||
{{familytree | | | | | | | | A00 | | | | | | | | | A00= <div style="float: left; text-align: left; width: 28em; padding:1em;">'''Identify cardinal findings that increase the pretest probability of [[Wolff-Parkinson-White syndrome]]'''<br> | |||
❑ Baseline [[ECG]] findings suggestive of [[WPW]] pattern ([[pre-excitation]]) | |||
: ❑ [[Short PR interval|PR interval (<120 ms)]] | |||
: ❑ [[Delta wave]] <br> [[File:WPW EKG leadV2.png|100px]] | |||
'''AND'''<br> | |||
❑ [[Tachyarrhythmia]]<br> | |||
'''''[[ECG]] findings suggestive of orthodromic [[AVRT]]''''' | |||
: ❑ Ventricular rate usually 200–300 bpm | |||
: ❑ Regular, narrow [[QRS complex]] (usually <120 ms unless pre-existing [[bundle branch block]] or [[aberrant conduction]]) | |||
: ❑ [[P wave]]s may be buried in the [[QRS complex|QRS]] or [[retrograde P wave|retrograde]] | |||
: ❑ [[Delta wave]] may be lost during [[NSR]] in case of participating concealed bypass tract | |||
'''''[[ECG]] findings suggestive of antidromic [[AVRT]]''''' | |||
: ❑ Ventricular rate usually 200–300 bpm | |||
: ❑ Regular, [[wide QRS complex]] | |||
: ❑ [[Delta wave]] is observed during [[NSR]] | |||
'''''[[ECG]] findings suggestive of [[AF]] with [[WPW]]''''' | |||
: ❑ Ventricular rate usually >200 bpm | |||
: ❑ Irregularly irregular, [[wide QRS complex]] with varying morphology | |||
: ❑ Absence of [[P waves]]</div>}} | |||
{{familytree | | | | | | | | |!| | | | | | | | | | }} | |||
{{familytree | | | | | | | | A01 | | | | | | | | | | A01= <div style="float: left; text-align: left; width: 28em; padding:1em;">'''Does the patient have any of the following findings that require urgent [[cardioversion]]?''' <br> | |||
❑ Hemodynamic instability | |||
:❑ [[Hypotension]] | |||
:❑ [[Cold extremities]] | |||
:❑ [[Cyanosis|Peripheral cyanosis]] | |||
:❑ [[Mottling]] | |||
:❑ [[Altered mental status]] | |||
❑ [[Chest discomfort]] suggestive of [[ischemia]] <br> | |||
❑ [[Heart failure|Decompensated heart failure]]<br></div>}} | |||
{{familytree | | | | | |,|-|-|^|-|-|.| | | | |}} | |||
{{familytree |boxstyle=padding: 0px; | | | | | B01 | | | | B02 | | | |B01=<div style="text-align: center; background: #FA8072; color: #F8F8FF; padding: 5px; font-weight: bold;">YES</div>| B02=<div style="text-align: center; font-weight: bold;">NO</div>}} | |||
{{familytree |boxstyle=border-top: 0px; padding: 0px;| | | | | C01 | | | | C02 | | |C01=<div style="text-align: center; background: #FA8072; color: #F8F8FF; font-weight: bold; padding: 15px;">Perform <BR> electrical cardioversion</div>|C02=<div style="text-align: left">'''[[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|Continue with the complete diagnostic approach below]]''' </div>}} | |||
{{familytree | | | | | |!| | | |}} | |||
{{familytree |boxstyle=padding: 0px; | | | | | Y01 | | |Y01=<div style="text-align: left; background: #FA8072; color: #F8F8FF; padding: 5px; font-size:85%"> | |||
❑ <BIG>'''''Irregular wide QRS complex'''''</BIG> | |||
: ❑ Unsynchronized, biphasic 120–200 J '''''OR''''' | |||
: ❑ Unsynchronized, monophasic 360 J | |||
❑ <BIG>'''''Irregular narrow QRS complex'''''</BIG> | |||
: ❑ Synchronized, biphasic 120–200 J '''''OR''''' | |||
: ❑ Synchronized, monophasic 200 J | |||
❑ <BIG>'''''Regular wide QRS complex'''''</BIG> | |||
: ❑ Synchronized, biphasic or monophasic 100 J | |||
❑ <BIG>'''''Regular narrow QRS complex'''''</BIG> | |||
: ❑ Synchronized, biphasic or monophasic 50–100 J | |||
</div>}} | |||
{{familytree | | | | | |!| | | |}} | |||
{{familytree |boxstyle=padding: 0px; | | | | | Z01 | | |Z01=<div style="text-align: left; font-weight: bold; padding: 5px;">'''[[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|After stabilizing the patient, continue with the complete diagnostic approach below]]''' </div>}} | |||
{{familytree/end}} | |||
=== | ==Complete Diagnostic Approach== | ||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> | |||
'''AVRT''': [[AV reentrant tachycardia]] | <span style="font-size:85%"> '''Abbreviations:''' '''AF:''' [[atrial fibrillation]]; '''AVRT''': [[AV reentrant tachycardia]]; '''BP:''' [[blood pressure]]; '''ECG:''' [[electrocardiography]]; '''HF:''' [[heart failure]]; '''LVH:''' [[left ventricular hypertrophy]]</span> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | A01 | | A01=<div style="float: left; text-align: left; width: 27em; padding:1em;"> '''Characterize the symptoms:'''<br> | {{familytree | | | | | A01 | | A01=<div style="float: left; text-align: left; width: 27em; padding:1em;"> '''Characterize the symptoms:'''<br> | ||
❑ Asymptomatic <br> | ❑ [[Asymptomatic]] <br> | ||
❑ [[Palpitations]]<br> | ❑ [[Palpitations]]<br> | ||
❑ [[Dyspnea]] <br> | ❑ [[Dyspnea]] <br> | ||
| Line 51: | Line 110: | ||
'''Characterize the timing of the symptoms:'''<br> | '''Characterize the timing of the symptoms:'''<br> | ||
❑ Onset <br> | ❑ Onset <br> | ||
:❑ First episode | |||
:❑ Recurrent | |||
❑ Duration <br> | ❑ Duration <br> | ||
❑ Frequency | ❑ Frequency<br> | ||
❑ Termination of the episode | |||
:❑ Spontaneous | |||
:❑ [[Medication]] use | |||
:❑ Not terminated | |||
</div> }} | </div> }} | ||
{{familytree | | | | |!| | | }} | {{familytree | | | | | |!| | | }} | ||
{{familytree | | | | B01 | | | B01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Identify possible triggers:'''<br> | {{familytree | | | | | B01 | | | B01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Identify possible triggers:'''<br> | ||
❑ [[Infection]]<br> | ❑ [[Infection]]<br> | ||
❑ [[Caffeine]]<br> | ❑ [[Caffeine]]<br> | ||
| Line 78: | Line 143: | ||
❑ [[Trauma]] <br> | ❑ [[Trauma]] <br> | ||
</div>}} | </div>}} | ||
{{familytree | | | | |!| | | }} | {{familytree | | | | | |!| | | }} | ||
{{familytree | | | | C01 | | | C01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Examine the patient:'''<br> | {{familytree | | | | | C01 | | | C01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Examine the patient:'''<br> | ||
'''Appearance of the patient'''<br> | '''Appearance of the patient'''<br> | ||
❑ | ❑ Cool and [[diaphoresis|diaphoretic]] <br> | ||
'''Vitals''' <br> | '''Vitals''' <br> | ||
❑ [[Heart rate]]: | ❑ [[Heart rate]] | ||
❑ [[Blood pressure]]: | : ❑ [[Tachycardia]] (150-250 beats per minute)<br> | ||
: ❑ [[Rhythm]] | |||
:: ❑ Regular (most of the cases) | |||
:: ❑ Irregularly irregular (suggestive of [[AF]]) | |||
❑ [[Blood pressure]] | |||
: ❑ [[Hypotension]] | |||
: ❑ Normal [[BP]] <br> | |||
'''Cardiovascular'''<br> | '''Cardiovascular'''<br> | ||
❑ Normal heart examination in most cases <br> | ❑ Normal [[heart]] examination in most cases <br> | ||
❑ [[Tricuspid regurgitation]] characterized by a [[holosystolic murmur]] heard best along the left lower [[sternal border]] (suggestive of [[Ebstein's anomaly]]) <br> | |||
❑ [[S4]] (suggestive of [[LVH]]) | |||
'''Respiratory'''<br> | '''Respiratory'''<br> | ||
❑ | ❑ [[Rales]] (suggestive of [[HF]]) | ||
</div>}} | </div>}} | ||
{{familytree | | | | |!| | | }} | {{familytree | | | | | |!| | | }} | ||
{{familytree | | | | | {{familytree | | | | | F01 | | | F01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Order studies:'''<br> | ||
❑ [[ECG]] <br> | ❑ [[ECG]] <br> | ||
❑ [[Echocardiography]] | ❑ [[Echocardiography]] screening for: <br> | ||
:❑ [[Hypertrophic cardiomyopathy]] | :❑ [[Hypertrophic cardiomyopathy]] | ||
:❑ [[Ebstein's anomaly of the tricuspid valve]] | :❑ [[Ebstein's anomaly of the tricuspid valve]] | ||
</div>}} | </div>}} | ||
{{familytree | |,|-|-| | {{familytree | |,|-|-|-|+|-|-|-|.| | | |}} | ||
{{familytree | D01 | | | | | {{familytree |boxstyle=vertical-align: top;| D01 | | D02 | | D03 | | | D01= <div style="float: left; text-align: left; width: 24em; padding:1em;">'''[[WPW]] with [[AF]]'''<br> | ||
❑ Suspect when [[AF]] appears with heart rates of 220 to 360<br> | |||
[[ | ❑ Irregularly irregular, [[wide QRS complex]] with varying morphology<br> | ||
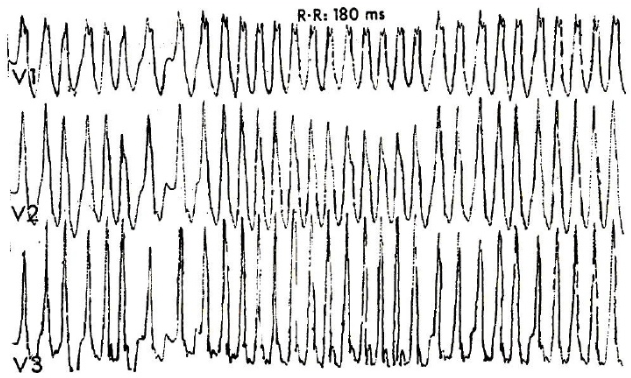
❑ Absence of [[P waves]]<ref name="FenglerBrady2007">{{cite journal|last1=Fengler|first1=Brian T.|last2=Brady|first2=William J.|last3=Plautz|first3=Claire U.|title=Atrial fibrillation in the Wolff-Parkinson-White syndrome: ECG recognition and treatment in the ED|journal=The American Journal of Emergency Medicine|volume=25|issue=5|year=2007|pages=576–583|issn=07356757|doi=10.1016/j.ajem.2006.10.017}}</ref><br>[[File:Wpw with afib.PNG|center|300px]] | |||
</div>| | </div>| | ||
D02= <div style="float: left; text-align: left; width: 24em; padding:1em;"> ''' | D02= <div style="float: left; text-align: left; width: 24em; padding:1em;"> '''Orthodromic AVRT''' <br> | ||
❑ Ventricular rate usually 200–300 bpm<br> | |||
[[File: | ❑ Regular, narrow [[QRS complex]] (usually <120 ms unless pre-existing [[bundle branch block]] or [[aberrant conduction]])<br> | ||
''' | ❑ [[P wave]]s may be buried in the [[QRS complex|QRS]] or [[retrograde P wave|retrograde]]<br> | ||
❑ | ❑ [[Delta wave]] may be lost during [[NSR]] in case of participating concealed bypass tract<br> | ||
❑ | [[File:SVT.jpg|300px|center]] | ||
</div> | | |||
D03= <div style="text-align: left; width: 24em; padding:1em;"> '''Antidromic AVRT'''<br> | |||
❑ Ventricular rate usually 200–300 bpm<br> | |||
❑ Regular, [[wide QRS complex]]<br> | |||
❑ [[Delta wave]] is observed during [[NSR]]<br> | |||
[[File:Wide complex tachy.jpg|300px|center]] | |||
</div> }} | </div> }} | ||
{{familytree/end}} | {{familytree/end}} | ||
== | ==Treatment== | ||
Shown below is an algorithm summarizing the initial approach to [[Wolff-Parkinson-White syndrome]] according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> | |||
===Initial Treatment=== | |||
Shown below is an algorithm summarizing the initial approach to [[Wolff-Parkinson-White syndrome]] according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref><ref name="ACLS">{{Cite web | last = | first = | title = Part 8: Adult Advanced Cardiovascular Life Support | url = http://circ.ahajournals.org/content/122/18_suppl_3/S729.full | publisher = | date = | accessdate = 3 April 2014 }}</ref> | |||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | {{familytree | | | | A01 | | | A01= <div style="text-align: left; padding:1em;">'''Does the patient have any of the following findings that require urgent cardioversion?''' <br> | ||
❑ | ❑ Hemodynamic instability | ||
:❑ [[Hypotension]] | |||
:❑ [[Cold extremities]] | |||
:❑ [[Cyanosis|Peripheral cyanosis]] | |||
:❑ [[Mottling]] | |||
:❑ [[Altered mental status]] | |||
❑ [[Chest discomfort]] suggestive of [[ischemia]] <br> | |||
❑ [[Heart failure|Decompensated heart failure]]<br> | |||
</div>}} | </div>}} | ||
{{familytree | {{familytree | |,|-|-|^|-|-|.| | | | |}} | ||
{{familytree | {{familytree | D01 | | | | D02 | | | | D01= '''Yes'''| D02= '''No'''}} | ||
{{familytree | {{familytree | |!| | | | | |!| | | | }} | ||
{{familytree | {{familytree | E01 | | | | E02 | | | | E01=<div style="text-align: left">❑ [[Direct current cardioversion]] (Urgent) <br> ''Check [[Wolff-Parkinson-White syndrome resident survival guide#FIRE:Focused Initial Rapid Evaluation|FIRE]] for details'' </div> | ||
E02= <div style=" | |E02=<div style="text-align: left"> '''What is the type of [[tachycardia]] according to the [[ECG]] findings?''' | ||
</div>}} | </div>}} | ||
{{familytree | |,|-|^|-|.| | | | | }} | {{familytree | | | | | | | |!| | | | }} | ||
{{familytree | F01 | | F02 | | | | | F01= '''Orthodromic AVRT'''| F02= '''Antidromic AVRT'''}} | {{familytree | |,|-|-|-|v|-|^|-|.| | | | | }} | ||
{{familytree | |!| | | |!| | | | | |}} | {{familytree | F00 | | F01 | | F02 | | | | | F00= '''WPW + AF (Stable)'''| F01= '''Orthodromic AVRT (Stable)'''| F02= '''Antidromic AVRT (Stable)'''}} | ||
{{familytree | G01 | | G02 | | | | | {{familytree | |!| | | |!| | | |!| | | | | |}} | ||
❑ Use [[vagal maneuvers]] ([[ACC AHA guidelines classification scheme| | {{familytree |boxstyle=vertical-align: top;| G00 | | G01 | | G02 | | | |G00=<div style="text-align: left; padding: 1em;"> | ||
:❑ [[Carotid sinus massage]] <br> | <span style="font-size: 100%; color: red;"> '''Avoid the use of AV node blocking agents such as digoxin, calcium channel blockers, beta blockers and adenosine.'''</span><br><br> | ||
❑ Administer [[procainamide]], 100 mg [[infusion]] diluted to 100mg/ml at a rate of 25-50 mg/min every 5 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence C]])<ref name="pmid23545139">{{cite journal| author=American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB et al.| title=Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. | journal=Circulation | year= 2013 | volume= 127 | issue= 18 | pages= 1916-26 | pmid=23545139 | doi=10.1161/CIR.0b013e318290826d | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23545139 }} </ref><br> | |||
:❑ Administer until the [[arrhythmia]] is suppressed or until 500 mg has been administered<br> | |||
:❑ Wait 10 minutes or longer to administer new [[dosage]] | |||
:[[Contraindication|<span style="font-size:85%;color:red">Contraindications:</span>]] [[Third degree AV block|<span style="font-size:85%;color:red">third degree AV block</span>]], [[Systemic lupus erythematosus|<span style="font-size:85%;color:red">lupus erythematosus</span>]], [[Hypersensitivity|<span style="font-size:85%;color:red">idiosyncratic hypersensitivity</span>]], [[Torsades de pointes|<span style="font-size:85%;color:red">torsades de pointes</span>]]<br> | |||
<CENTER>'''''OR'''''</CENTER> | |||
❑ Administer [[ibutilide]] 1 mg IV [[infusion]] over 10 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence C]])<ref name="pmid23545139">{{cite journal| author=American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB et al.| title=Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. | journal=Circulation | year= 2013 | volume= 127 | issue= 18 | pages= 1916-26 | pmid=23545139 | doi=10.1161/CIR.0b013e318290826d | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23545139 }} </ref><br> | |||
:❑ Repeat the [[dosage]] if the [[tachycardia]] continues <br> | |||
:<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] [[Hypersensitivity|<span style="color:red">hypersensitivity</span>]] to [[Ibutilide|<span style="color:red">ibutilide</span>]] or any component of the formulation, [[QT interval|<span style="color:red">QTc</span>]] >440 msec</span><br> | |||
<CENTER>'''''OR'''''</CENTER> | |||
❑ Administer [[flecainide]] 50 mg every 12 hours ([[ACC AHA guidelines classification scheme|Class IIa, Level of Evidence B]])<ref name="pmid23545139">{{cite journal| author=American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB et al.| title=Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. | journal=Circulation | year= 2013 | volume= 127 | issue= 18 | pages= 1916-26 | pmid=23545139 | doi=10.1161/CIR.0b013e318290826d | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23545139 }} </ref> | |||
:❑ Increase 50mg BID every four days until efficacy is achieved <br> | |||
:❑ Maximum [[dose]] recommended for [[SVT]] is 300 mg/day<br> | |||
:<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] pre-existing [[Second degree AV block|<span style="color:red">second degree AV block</span>]] or [[Third degree AV block|<span style="color:red">third degree AV block</span>]] , [[Right bundle brnach block|<span style="color:red">right bundle branch block</span>]] associated with a left hemiblock unless a [[Artificial pacemaker|<span style="color:red">pacemaker</span>]] is present, [[Shock|<span style="color:red">cardiogenic shock</span>]], [[Hypersensitivity|<span style="color:red">hypersensitivity</span>]] to the drug</span><br> | |||
</div> | |||
|G01= <div style="text-align: left; padding: 1em;">❑ Use [[vagal maneuvers]] ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]])<br> | |||
:❑ [[Carotid sinus massage]] <br> | |||
:❑ [[Valsalva maneuver]] <br> | :❑ [[Valsalva maneuver]] <br> | ||
<br>''If not effective initiate IV AV nodal blocking agent''<br><br> | <br>''If not effective initiate IV AV nodal blocking agent''<br><br> | ||
❑ Administer [[adenosine]] | ❑ Administer [[adenosine]] 6 mg IV (bolus) ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence A]])<br> | ||
: ❑ If initial [[dose]] is not effective, administer a second [[dose]] of 12 mg, repeated a second time if required<br> | |||
:<span style="font-size:85%;color:red">Contraindications: second | :<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] [[Second degree AV block|<span style="color:red">second degree AV block</span>]] or [[Third degree AV block|<span style="color:red">third degree AV block</span>]] unless a [[Artificial pacemaker|<span style="color:red">pacemaker</span>]] is present</span><br> | ||
<br>''If not effective''<br><br> | ''If not effective''<br><br> | ||
❑ Administer [[verapamil]] | ❑ Administer [[verapamil]] 5 to 10 mg (0.075 to 0.15 mg/kg body weight) IV [[Bolus|boluses]] of over 2 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence A]])<br> | ||
:❑ | : ❑ Give 30% of the [[dose]] in case of [[hepatic impairment]]<br> | ||
:❑ | : ❑ Monitor for [[prolonged PR interval]] in case of [[renal impairment]]<br> | ||
:<span style="font-size:85%;color:red">Contraindications: hypotension | :<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] [[Congestive heart failure|<span style="color:red">severe left ventricular dysfunction</span>]], [[Hypotension|<span style="color:red">hypotension</span>]] or [[Shock|<span style="color:red">cardiogenic shock</span>]]</span><br> | ||
<br>''If not effective''<br><br> | ''If not effective''<br><br> | ||
❑ Administer [[procainamide]], | ❑ Administer [[procainamide]], 100 mg [[infusion]] diluted to 100mg/ml at a rate of 25-50 mg/min every 5 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]])<br> | ||
:❑ Give until the [[arrhythmia]] is suppressed or up to 500 mg <br> | |||
:❑ | :❑ Wait 10 minutes or longer to administer new dosage <br> | ||
:❑ | :❑ [[Dosage]] should be adjusted for the individual patient in case of [[renal impairment]]<br> | ||
:<span style="font-size:85%;color:red">Contraindications: | :[[Contraindication|<span style="font-size:85%;color:red">Contraindications:</span>]] [[Third degree AV block|<span style="font-size:85%;color:red">third degree AV block</span>]], [[Systemic lupus erythematosus|<span style="font-size:85%;color:red">lupus erythematosus</span>]], [[Hypersensitivity|<span style="font-size:85%;color:red">idiosyncratic hypersensitivity</span>]], [[Torsades de pointes|<span style="font-size:85%;color:red">torsades de pointes</span>]]</div> | ||
</div> | | | G02= <div style="text-align: left; padding: 1em;"><span style="font-size:100%;color:red"> '''Avoid the use of AV node blocking agents such as digoxin, calcium channel blockers, beta blockers and adenosine.'''</span><br><br> | ||
G02= <div style=" | ❑ Administer [[procainamide]], 100 mg [[infusion]] diluted to 100mg/ml at a rate of 25-50 mg/min every 5 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]])<br> | ||
❑ Administer | :❑ Give until the [[arrhythmia]] is suppressed or until 500 mg has been administered<br> | ||
:❑ Wait 10 minutes or longer to administer new [[dosage]] | |||
:[[Contraindication|<span style="font-size:85%;color:red">Contraindications:</span>]] [[Third degree AV block|<span style="font-size:85%;color:red">third degree AV block</span>]], [[Systemic lupus erythematosus|<span style="font-size:85%;color:red">lupus erythematosus</span>]], [[Hypersensitivity|<span style="font-size:85%;color:red">idiosyncratic hypersensitivity</span>]], [[Torsades de pointes|<span style="font-size:85%;color:red">torsades de pointes</span>]]<br> | |||
::<span style="font-size:85%;color:red">Contraindications: | <CENTER>'''''OR'''''</CENTER> | ||
:: | |||
: | |||
</ | |||
=== | ❑ Administer [[ibutilide]] 1 mg IV infusion over 10 minutes ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]])<br> | ||
:❑ Repeat the [[dosage]] if the [[tachycardia]] continues <br> | |||
:<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] [[Hypersensitivity|<span style="color:red">hypersensitivity</span>]] to [[Ibutilide|<span style="color:red">ibutilide</span>]] or any component of the formulation, [[QT interval|<span style="color:red">QTc</span>]] >440 msec</span><br> | |||
<CENTER>'''''OR'''''</CENTER> | |||
❑ Administer [[flecainide]] 50 mg every 12 hours | |||
:❑ Increase 50mg BID every four days until efficacy is achieved <br> | |||
:❑ Maximum [[dose]] recommended for [[SVT]] is 300 mg/day<br> | |||
:<span style="font-size:85%;color:red">[[Contraindication|<span style="color:red">Contraindications:</span>]] pre-existing [[Second degree AV block|<span style="color:red">second degree AV block</span>]] or [[Third degree AV block|<span style="color:red">third degree AV block</span>]] , [[Right bundle brnach block|<span style="color:red">right bundle branch block</span>]] associated with a left hemiblock unless a [[Artificial pacemaker|<span style="color:red">pacemaker</span>]] is present, [[Shock|<span style="color:red">cardiogenic shock</span>]], [[Hypersensitivity|<span style="color:red">hypersensitivity</span>]] to the drug</span><br> | |||
❑ | |||
❑ | |||
❑ [[ | |||
< | |||
</ | |||
</ | |||
</div>}} | </div>}} | ||
{{familytree/end}} | {{familytree/end}} | ||
=== | ===Long-Term Treatment=== | ||
Shown below is an algorithm summarizing the | Shown below is an algorithm summarizing the long-term treatment of [[Wolff-Parkinson-White syndrome]].<ref name="circ.ahajournals.org">{{Cite web | last = | first = | title = ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary | url = http://circ.ahajournals.org/content/108/15/1871 | publisher = | date = | accessdate = 15 August 2013 }}</ref> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | A01 | | | | | | | | | | {{familytree | | | | | | A01 | | | | | A01= '''Does the patient with pre-excitation have symptomatic arrhythmia?'''}} | ||
❑ | {{familytree | | | | |,|-|^|-|.| | | | }} | ||
{{familytree | | | | B01 | | B02 | | B01= '''Yes'''| B02= '''No'''}} | |||
{{familytree | | | | |!| | | |!| | | }} | |||
</div>}} | {{familytree | | | | C01 | | C02 | | C01= '''Is the arrhythmia poorly tolerated, OR''' <br>'''is atrial fibrillation with rapid conduction present?'''|C02= <div style="text-align: left; padding: 1em;"> | ||
{{familytree | |,|-|-| | ❑ No treatment ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence C]]) <br><CENTER>'''''OR'''''</CENTER> | ||
{{familytree | | ❑ [[Catheter ablation]] ([[ACC AHA guidelines classification scheme|Class IIa, Level of Evidence B]]) </div>}} | ||
{{familytree | |! | {{familytree | | |,|-|^|-|.| | | | | |}} | ||
{{familytree | | {{familytree | | D01 | | D02 | | | | |D01= '''Yes''' | D02= '''No'''}} | ||
❑ | {{familytree | | |!| | | |!| | | }} | ||
:❑ [[ | {{familytree | | E01 | | E02 | | E01= <div style="float: left; text-align: left; width: 24em; padding:1em;"> ❑ [[Catheter ablation]] ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]]) </div> | ||
| E02=<div style="text-align: left; padding: 1em;"> | |||
❑ [[Catheter ablation]] ([[ACC AHA guidelines classification scheme|Class I, Level of Evidence B]])<br><CENTER>'''''OR'''''</CENTER> | |||
: | ❑ [[Antiarrhythmic agents|Class I C antiarrhythmic agents]] such as: [[flecainide]], [[propafenone]] ([[ACC AHA guidelines classification scheme|Class IIa, Level of Evidence C]])<br><CENTER>'''''OR'''''</CENTER> | ||
❑ [[Sotalol]], [[amiodarone]] or [[beta blockers]] ([[ACC AHA guidelines classification scheme|Class IIa, Level of Evidence C]])<br> | |||
<span style="font-size:100%;color:red">Avoid AV blocking agents such as: digoxin, verapamil, dialtizem</span> ([[ACC AHA guidelines classification scheme|Class III, Level of Evidence C]])<br> | |||
</div> }} | |||
</ | |||
</div>}} | |||
{{familytree/end}} | {{familytree/end}} | ||
==Do's== | ==Do's== | ||
* Perform [[catheter ablation]] of the [[accessory pathway]] if possible ([[ACC AHA guidelines classification scheme|Class I, Level of evidence B]]). | |||
* Consider [[propafenone]] over [[flecainide]] for the prevention of recurrence of orthodromic [[AVRT]] because [[propafenone]] it has also a mild beta blocking activity. | |||
* Schedule [[exercise stress test]] and [[electrophysiology]] tests for the [[sudden cardiac death]] stratification ([[ACC AHA guidelines classification scheme|Class IIa, Level of evidence B]]). | |||
* Consider [[catheter ablation]] in [[asymptomatic]] patients with [[structural heart disease]] ([[ACC AHA guidelines classification scheme|Class IIb, Level of evidence C]]). | |||
* Administer IV [[procainamide]] ([[ACC AHA guidelines classification scheme|Class I, Level of evidence C]]), [[ibutilide]] ([[ACC AHA guidelines classification scheme|Class I, Level of evidence C]]) or [[flecainide]] ([[ACC AHA guidelines classification scheme|Class IIa, Level of evidence B]]) among [[WPW syndrome]] patients who present with [[atrial fibrillation]] . Intravenous [[quinidine]], [[procainamide]], [[disopyramide]], [[ibutilide]], or [[amiodarone]] can also be considered ([[ACC AHA guidelines classification scheme|Class IIb, Level of evidence B]]).<ref name="pmid23545139">{{cite journal| author=American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB et al.| title=Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. | journal=Circulation | year= 2013 | volume= 127 | issue= 18 | pages= 1916-26 | pmid=23545139 | doi=10.1161/CIR.0b013e318290826d | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23545139 }} </ref> | |||
==Don'ts== | ==Don'ts== | ||
* Don't administer AV blocking agents in patients with [[WPW]] and antidromic AVRT as it will promote conduction down the accessory pathway ([[ACC AHA guidelines classification scheme|Class III, Level of evidence C]]).<ref name="Garratt-1989">{{Cite journal | last1 = Garratt | first1 = C. | last2 = Antoniou | first2 = A. | last3 = Ward | first3 = D. | last4 = Camm | first4 = AJ. | title = Misuse of verapamil in pre-excited atrial fibrillation. | journal = Lancet | volume = 1 | issue = 8634 | pages = 367-9 | month = Feb | year = 1989 | doi = | PMID = 2563516 }}</ref><ref name="Gulamhusein-1982">{{Cite journal | last1 = Gulamhusein | first1 = S. | last2 = Ko | first2 = P. | last3 = Carruthers | first3 = SG. | last4 = Klein | first4 = GJ. | title = Acceleration of the ventricular response during atrial fibrillation in the Wolff-Parkinson-White syndrome after verapamil. | journal = Circulation | volume = 65 | issue = 2 | pages = 348-54 | month = Feb | year = 1982 | doi = | PMID = 7053894 }}</ref><ref name="McGovern-1986">{{Cite journal | last1 = McGovern | first1 = B. | last2 = Garan | first2 = H. | last3 = Ruskin | first3 = JN. | title = Precipitation of cardiac arrest by verapamil in patients with Wolff-Parkinson-White syndrome. | journal = Ann Intern Med | volume = 104 | issue = 6 | pages = 791-4 | month = Jun | year = 1986 | doi = | PMID = 3706931 }}</ref> | |||
<ref name="Gulamhusein-1982">{{Cite journal | last1 = Gulamhusein | first1 = S. | last2 = Ko | first2 = P. | last3 = Carruthers | first3 = SG. | last4 = Klein | first4 = GJ. | title = Acceleration of the ventricular response during atrial fibrillation in the Wolff-Parkinson-White syndrome after verapamil. | journal = Circulation | volume = 65 | issue = 2 | pages = 348-54 | month = Feb | year = 1982 | doi = | PMID = 7053894 }}</ref> | * Don't administer AV blocking agents in patients with [[WPW]] and [[AF]] ([[ACC AHA guidelines classification scheme|Class III, Level of evidence B]]).<br> | ||
<ref name="McGovern-1986">{{Cite journal | last1 = McGovern | first1 = B. | last2 = Garan | first2 = H. | last3 = Ruskin | first3 = JN. | title = Precipitation of cardiac arrest by verapamil in patients with Wolff-Parkinson-White syndrome. | journal = Ann Intern Med | volume = 104 | issue = 6 | pages = 791-4 | month = Jun | year = 1986 | doi = | PMID = 3706931 }}</ref | * Don't administer AV blocking agents (such as [[digoxin]], [[verapamil]] or [[diltiazem]]) in the chronic treatment of [[WPW syndrome]] to prevent the recurrence of tachycardia ([[ACC AHA guidelines classification scheme|Class III, Level of evidence B]]).<br> | ||
==References== | ==References== | ||
{{reflist| | {{reflist|2}} | ||
[[Category:Help]] | [[Category:Help]] | ||
Latest revision as of 02:42, 26 October 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]; Hilda Mahmoudi M.D., M.P.H.[3]; Alejandro Lemor, M.D. [4]
| Wolff-Parkinson-White Syndrome Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagsis |
| Treatment |
| Do's |
| Don'ts |
Overview
Wolff-Parkinson-White (WPW) syndrome is a condition of pre-excitation of the ventricles of the heart due to the presence of an accessory pathway known as the Bundle of Kent through which the electrical impulses bypass the AV node. The difference between WPW pattern and WPW syndrome is that WPW pattern is characterized by the presence of characteristic ECG findings, such as a short PR interval and a delta wave, whereas WPW syndrome is the occurrence of tachycardia with or without associated symptoms in a subject with existing WPW pattern.[1] The treatment of WPW syndrome is targeted towards the restoration of the sinus rhythm, usually by the administration of either ibutilide or procainamide. The most common type of arrhythmia in WPW syndrome is AV reentrant tachycardia.[2] Atrial fibrillation in a patient with WPW is life threatening and should be managed urgently. Atrial fibrillation in a patient with WPW should be suspected when there is ECG findings suggestive of atrial fibrillation in the context of a heart rate higher than 220 beats per minute.
Causes
Life Threatening Causes
Wolff-Parkinson-White syndrome can be a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[2][3]
Boxes in red signify that an urgent management is needed.
Abbreviations: AF: atrial fibrillation; AVRT: AV reentrant tachycardia; BP: blood pressure; ECG: electrocardiography; HF: heart failure; LVH: left ventricular hypertrophy; WPW: Wolff-Parkinson-White pattern
Identify cardinal findings that increase the pretest probability of Wolff-Parkinson-White syndrome ❑ Baseline ECG findings suggestive of WPW pattern (pre-excitation) AND ECG findings suggestive of orthodromic AVRT
ECG findings suggestive of antidromic AVRT
ECG findings suggestive of AF with WPW
| |||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings that require urgent cardioversion? ❑ Hemodynamic instability ❑ Chest discomfort suggestive of ischemia | |||||||||||||||||||||||||||||||||||||
YES | NO | ||||||||||||||||||||||||||||||||||||
Perform electrical cardioversion | |||||||||||||||||||||||||||||||||||||
❑ Irregular wide QRS complex
❑ Irregular narrow QRS complex
❑ Regular wide QRS complex
❑ Regular narrow QRS complex
| |||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2]
Abbreviations: AF: atrial fibrillation; AVRT: AV reentrant tachycardia; BP: blood pressure; ECG: electrocardiography; HF: heart failure; LVH: left ventricular hypertrophy
Characterize the symptoms: ❑ Asymptomatic
❑ Duration
| |||||||||||||||||||||||||||
Identify possible triggers: ❑ Infection | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vitals
Cardiovascular | |||||||||||||||||||||||||||
Order studies: ❑ ECG | |||||||||||||||||||||||||||
Orthodromic AVRT ❑ Ventricular rate usually 200–300 bpm 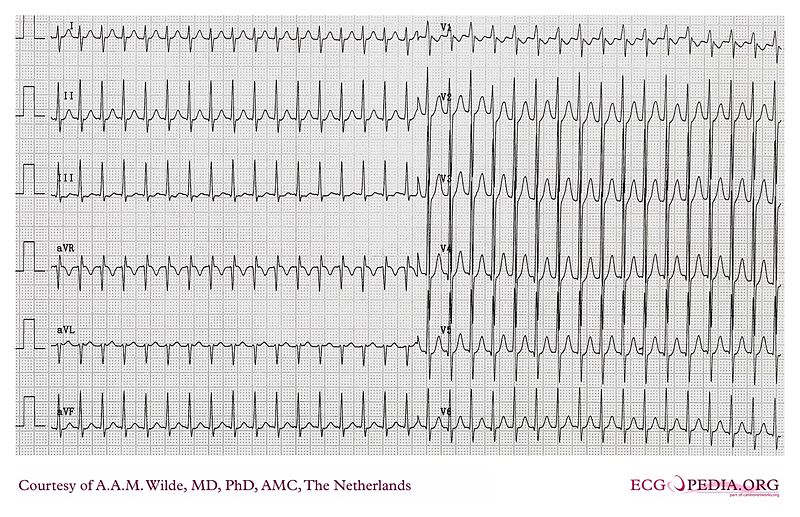 | Antidromic AVRT ❑ Ventricular rate usually 200–300 bpm 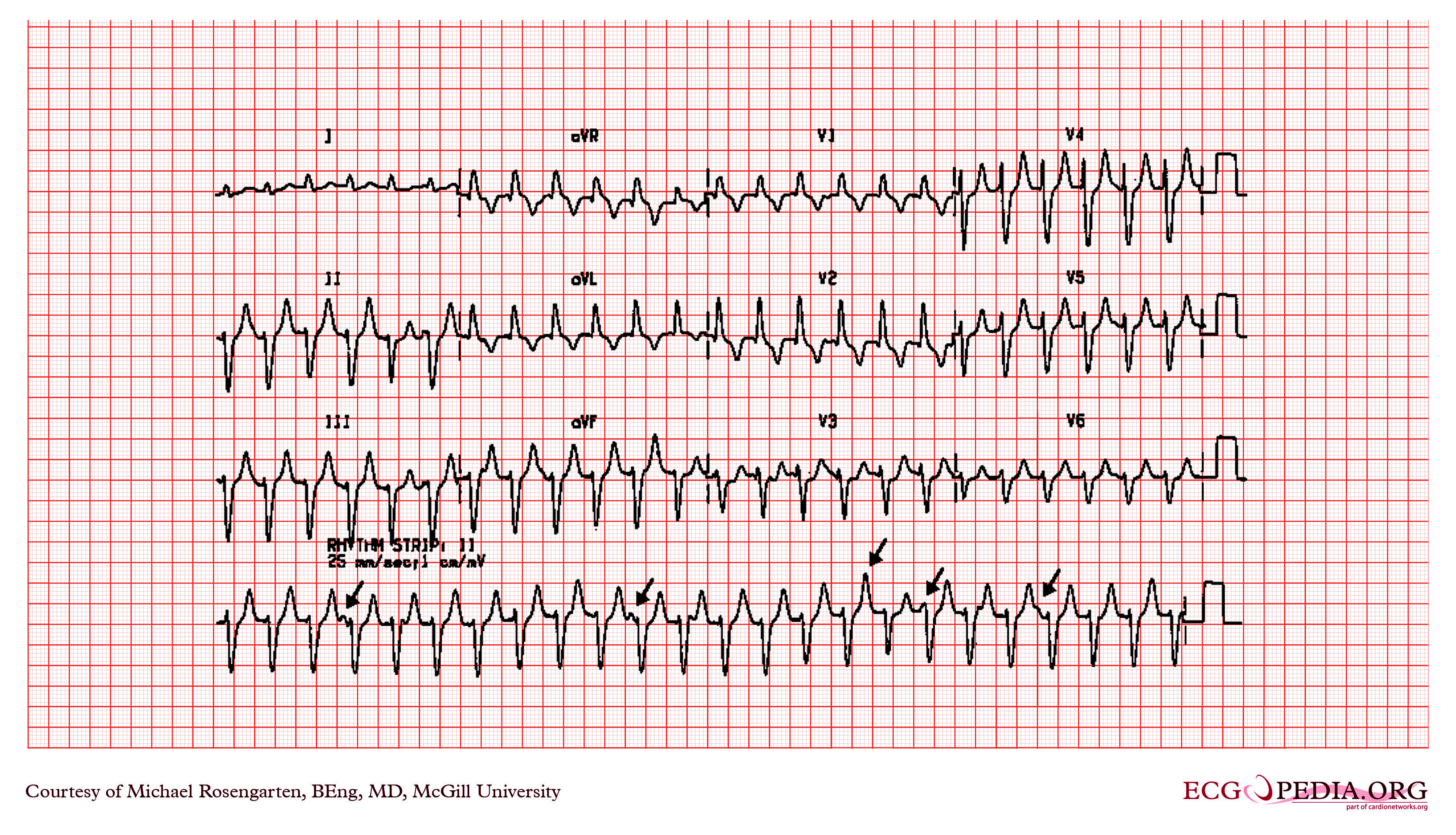 | ||||||||||||||||||||||||||
Treatment
Initial Treatment
Shown below is an algorithm summarizing the initial approach to Wolff-Parkinson-White syndrome according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.[2][3]
Does the patient have any of the following findings that require urgent cardioversion? ❑ Hemodynamic instability ❑ Chest discomfort suggestive of ischemia | |||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||
What is the type of tachycardia according to the ECG findings?
| |||||||||||||||||||||||||||||||
| WPW + AF (Stable) | Orthodromic AVRT (Stable) | Antidromic AVRT (Stable) | |||||||||||||||||||||||||||||
Avoid the use of AV node blocking agents such as digoxin, calcium channel blockers, beta blockers and adenosine.
❑ Administer ibutilide 1 mg IV infusion over 10 minutes (Class I, Level of Evidence C)[5]
❑ Administer flecainide 50 mg every 12 hours (Class IIa, Level of Evidence B)[5]
| ❑ Use vagal maneuvers (Class I, Level of Evidence B)
If not effective
If not effective
| Avoid the use of AV node blocking agents such as digoxin, calcium channel blockers, beta blockers and adenosine. ❑ Administer procainamide, 100 mg infusion diluted to 100mg/ml at a rate of 25-50 mg/min every 5 minutes (Class I, Level of Evidence B)
❑ Administer ibutilide 1 mg IV infusion over 10 minutes (Class I, Level of Evidence B)
❑ Administer flecainide 50 mg every 12 hours
| |||||||||||||||||||||||||||||
Long-Term Treatment
Shown below is an algorithm summarizing the long-term treatment of Wolff-Parkinson-White syndrome.[2]
| Does the patient with pre-excitation have symptomatic arrhythmia? | |||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||
| Is the arrhythmia poorly tolerated, OR is atrial fibrillation with rapid conduction present? |
❑ No treatment (Class I, Level of Evidence C) | ||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||
❑ Catheter ablation (Class I, Level of Evidence B) ❑ Sotalol, amiodarone or beta blockers (Class IIa, Level of Evidence C) | |||||||||||||||||||||||||
Do's
- Perform catheter ablation of the accessory pathway if possible (Class I, Level of evidence B).
- Consider propafenone over flecainide for the prevention of recurrence of orthodromic AVRT because propafenone it has also a mild beta blocking activity.
- Schedule exercise stress test and electrophysiology tests for the sudden cardiac death stratification (Class IIa, Level of evidence B).
- Consider catheter ablation in asymptomatic patients with structural heart disease (Class IIb, Level of evidence C).
- Administer IV procainamide (Class I, Level of evidence C), ibutilide (Class I, Level of evidence C) or flecainide (Class IIa, Level of evidence B) among WPW syndrome patients who present with atrial fibrillation . Intravenous quinidine, procainamide, disopyramide, ibutilide, or amiodarone can also be considered (Class IIb, Level of evidence B).[5]
Don'ts
- Don't administer AV blocking agents in patients with WPW and antidromic AVRT as it will promote conduction down the accessory pathway (Class III, Level of evidence C).[6][7][8]
- Don't administer AV blocking agents in patients with WPW and AF (Class III, Level of evidence B).
- Don't administer AV blocking agents (such as digoxin, verapamil or diltiazem) in the chronic treatment of WPW syndrome to prevent the recurrence of tachycardia (Class III, Level of evidence B).
References
- ↑ "Wolff-Parkinson-White Syndrome and Accessory Pathways". Retrieved 1 April 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ 3.0 3.1 "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ Fengler, Brian T.; Brady, William J.; Plautz, Claire U. (2007). "Atrial fibrillation in the Wolff-Parkinson-White syndrome: ECG recognition and treatment in the ED". The American Journal of Emergency Medicine. 25 (5): 576–583. doi:10.1016/j.ajem.2006.10.017. ISSN 0735-6757.
- ↑ 5.0 5.1 5.2 5.3 American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB; et al. (2013). "Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines". Circulation. 127 (18): 1916–26. doi:10.1161/CIR.0b013e318290826d. PMID 23545139.
- ↑ Garratt, C.; Antoniou, A.; Ward, D.; Camm, AJ. (1989). "Misuse of verapamil in pre-excited atrial fibrillation". Lancet. 1 (8634): 367–9. PMID 2563516. Unknown parameter
|month=ignored (help) - ↑ Gulamhusein, S.; Ko, P.; Carruthers, SG.; Klein, GJ. (1982). "Acceleration of the ventricular response during atrial fibrillation in the Wolff-Parkinson-White syndrome after verapamil". Circulation. 65 (2): 348–54. PMID 7053894. Unknown parameter
|month=ignored (help) - ↑ McGovern, B.; Garan, H.; Ruskin, JN. (1986). "Precipitation of cardiac arrest by verapamil in patients with Wolff-Parkinson-White syndrome". Ann Intern Med. 104 (6): 791–4. PMID 3706931. Unknown parameter
|month=ignored (help)