Wilson's disease history and symptoms: Difference between revisions
| Line 17: | Line 17: | ||
About half the patients with Wilson's have neurological or psychiatric problems. Most patients initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms then follow, often in the form of[[parkinsonism]] (increased rigidity and slowing of routine movements) with or without a typical hand [[tremor]], [[ataxia]] (lack of coordination) or [[dystonia]] (twisting and repetitive movements of part of the body). [[Seizure]]s and [[migraine]] appear to be more common in Wilson's disease.<ref name=Ala/> | About half the patients with Wilson's have neurological or psychiatric problems. Most patients initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms then follow, often in the form of[[parkinsonism]] (increased rigidity and slowing of routine movements) with or without a typical hand [[tremor]], [[ataxia]] (lack of coordination) or [[dystonia]] (twisting and repetitive movements of part of the body). [[Seizure]]s and [[migraine]] appear to be more common in Wilson's disease.<ref name=Ala/> | ||
Psychiatric problems due to Wilson's disease may include behavioral changes, [[clinical depression|depression]], [[anxiety]] and[[psychosis]].<ref name=Ala/> | Psychiatric problems due to Wilson's disease may include behavioral changes, [[clinical depression|depression]], [[anxiety]] and [[psychosis]].<ref name=Ala/> | ||
===Other organ systems=== | ===Other organ systems=== | ||
Revision as of 19:48, 22 August 2012
|
Wilson's disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Wilson's disease history and symptoms On the Web |
|
American Roentgen Ray Society Images of Wilson's disease history and symptoms |
|
Risk calculators and risk factors for Wilson's disease history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
History and symptoms
The main sites of copper accumulation are the liver and the brain, and consequently liver disease and neuropsychiatric symptoms are the main features that lead to diagnosis.[1] Patients with liver problems tend to come to medical attention earlier, generally as children or teenagers, than those with neurological and psychiatric symptoms, who tend to be in their twenties or older. Some are identified only because relatives have been diagnosed with Wilson's disease; many of these patients, when tested, turn out to have been experiencing symptoms of the condition but haven't received a diagnosis.[2]
Liver disease
Liver disease may present as tiredness, increased bleeding tendency or confusion (due to hepatic encephalopathy) and portal hypertension. The latter, a condition in which the pressure on the portal vein is markedly increased, leads to esophageal varices (blood vessels in the esophagus) that may bleed in a life-threatening fashion, splenomegaly(enlargement of the spleen) and ascites (accumulation of fluid in the abdominal cavity). On examination, signs of chronic liver disease such as spider naevi (small distended blood vessels, usually on the chest) may be observed. Chronic active hepatitis has caused cirrhosis of the liver in most patients by the time they develop symptoms. While most people with cirrhosis have an increased risk of hepatocellular carcinoma (liver cancer), this risk is relatively very low in Wilson's disease.[1]
About 5% of all patients are diagnosed only when they develop fulminant acute liver failure, often in the context of a hemolytic anemia (anemia due to the destruction of red blood cells). This leads to abnormalities in protein production (identified by deranged coagulation) and metabolism by the liver. The deranged protein metabolism leads to the accumulation of waste products such as ammonia in the bloodsteam. When these irritate the brain, the patient develops hepatic encephalopathy (confusion, coma, seizures and finally life-threatening swelling of the brain).[1]
Neuropsychiatric symptoms
About half the patients with Wilson's have neurological or psychiatric problems. Most patients initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms then follow, often in the form ofparkinsonism (increased rigidity and slowing of routine movements) with or without a typical hand tremor, ataxia (lack of coordination) or dystonia (twisting and repetitive movements of part of the body). Seizures and migraine appear to be more common in Wilson's disease.[1]
Psychiatric problems due to Wilson's disease may include behavioral changes, depression, anxiety and psychosis.[1]
Other organ systems
Various medical conditions have been linked with copper accumulation in Wilson's disease:
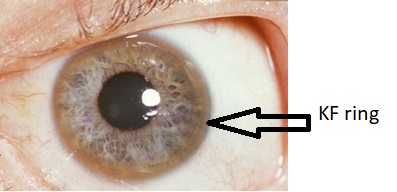
- Eyes: Kayser-Fleischer rings (KF rings) may be visible around the iris. They are due to copper deposition in Descemet's membrane of the cornea. They do not occur in all patients and may only be visible on slit lamp examination. Wilson's disease is also associated with sunflower cataracts, brown or green pigmentation of the anterior and posterior lens capsule. Neither cause significant visual loss.[1] KF rings occur in 66% of cases, more often in those with neurological than with liver problems.[2]
- Kidneys: renal tubular acidosis, a disorder of bicarbonate handling by theproximal tubules leads to nephrocalcinosis (calcium accumulation in the kidneys), weakening of the bone (due to calcium and phosphate loss) and occasionally aminoaciduria (loss of amino acids, needed for protein synthesis).[1]
- Heart: cardiomyopathy (weakness of the heart muscle) is a rare but recognized problem in Wilson's disease; it may lead toheart failure (fluid accumulation due to decreased pump function) and cardiac arrhythmias (episodes of irregular and/or abnormally fast or slow heart beat).[1]
- Hormones: hypoparathyroidism (failure of the parathyroid glands, leading to low calcium levels), infertility andhabitual abortion.[1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML (2007). "Wilson's disease". Lancet. 369 (9559): 397–408. doi:10.1016/S0140-6736(07)60196-2. PMID 17276780.
- ↑ 2.0 2.1 Merle U, Schaefer M, Ferenci P, Stremmel W (2007). "Clinical presentation, diagnosis and long-term outcome of Wilson's disease: a cohort study". Gut. 56 (1): 115–20. doi:10.1136/gut.2005.087262. PMID 16709660.