Turner syndrome echocardiography and ultrasound: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Prenatal ultrasounds | [[Prenatal]] [[ultrasounds]] may show a left-sided [[cardiac]] defect, [[renal]] anomalies, growth retardation, relatively short limbs, [[fetal edema]], [[cystic hygroma]], [[polyhydramnios]] and [[brachycephaly]]. [[Echocardiographies]] and renal ultrasounds help detect structural defects. | ||
==Echocardiography/Ultrasound== | ==Echocardiography/Ultrasound== | ||
*Turner syndrome may be diagnosed or suspected prenatally because of an ultrasonography showing a left-sided cardiac defect, renal anomalies, growth retardation, relatively short limbs, fetal edema, cystic hygroma, polyhydramnios and brachycephaly. | *[[Turner syndrome]] may be diagnosed or suspected prenatally because of an ultrasonography showing a left-sided cardiac defect, renal anomalies, growth retardation, relatively short limbs, [[fetal edema]], [[cystic hygroma]], [[polyhydramnios]] and [[brachycephaly]]. | ||
*Echocardiography for cardiac structural abnormalities especially aortic dilation that predisposes the individual to aortic dissection and sudden cardiac death. <ref name="pmid16929365">{{cite journal| author=Gravholt CH| title=Clinical practice in Turner syndrome. | journal=Nat Clin Pract Endocrinol Metab | year= 2005 | volume= 1 | issue= 1 | pages= 41-52 | pmid=16929365 | doi=10.1038/ncpendmet0024 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16929365 }} </ref> | *Echocardiography for cardiac structural abnormalities especially [[aortic dilation]] that predisposes the individual to [[aortic dissection]] and sudden [[cardiac death]]. <ref name="pmid16929365">{{cite journal| author=Gravholt CH| title=Clinical practice in Turner syndrome. | journal=Nat Clin Pract Endocrinol Metab | year= 2005 | volume= 1 | issue= 1 | pages= 41-52 | pmid=16929365 | doi=10.1038/ncpendmet0024 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16929365 }} </ref> | ||
**The aortic severity index is a useful prognostic indicator when assessing for the risk of aortic dilatation. <ref name="pmid20081420">{{cite journal| author=Wolff DJ, Van Dyke DL, Powell CM, Working Group of the ACMG Laboratory Quality Assurance Committee| title=Laboratory guideline for Turner syndrome. | journal=Genet Med | year= 2010 | volume= 12 | issue= 1 | pages= 52-5 | pmid=20081420 | doi=10.1097/GIM.0b013e3181c684b2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20081420 }} </ref> | **The [[aortic severity index]] is a useful prognostic indicator when assessing for the risk of [[aortic dilatation]]. <ref name="pmid20081420">{{cite journal| author=Wolff DJ, Van Dyke DL, Powell CM, Working Group of the ACMG Laboratory Quality Assurance Committee| title=Laboratory guideline for Turner syndrome. | journal=Genet Med | year= 2010 | volume= 12 | issue= 1 | pages= 52-5 | pmid=20081420 | doi=10.1097/GIM.0b013e3181c684b2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20081420 }} </ref> | ||
**It is the aortic diameter corrected for body surface area and a score of more than 2.3cm/m2 indicates a high risk of aortic dissection (2-2.3cm/m2 is considered as moderate risk). | **It is the aortic diameter corrected for body surface area and a score of more than 2.3cm/m2 indicates a high risk of [[aortic dissection]] (2-2.3cm/m2 is considered as moderate risk). | ||
**The advice offered to moderate risk patients is restriction of activities and that offered to high risk patients is that they should completely avoid competitive sports and intensive weight training. <ref name="pmid29344338">{{cite journal| author=Shankar RK, Backeljauw PF| title=Current best practice in the management of Turner syndrome. | journal=Ther Adv Endocrinol Metab | year= 2018 | volume= 9 | issue= 1 | pages= 33-40 | pmid=29344338 | doi=10.1177/2042018817746291 | pmc=5761955 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29344338 }} </ref> | **The advice offered to moderate risk patients is restriction of activities and that offered to high risk patients is that they should completely avoid competitive sports and intensive weight training. <ref name="pmid29344338">{{cite journal| author=Shankar RK, Backeljauw PF| title=Current best practice in the management of Turner syndrome. | journal=Ther Adv Endocrinol Metab | year= 2018 | volume= 9 | issue= 1 | pages= 33-40 | pmid=29344338 | doi=10.1177/2042018817746291 | pmc=5761955 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29344338 }} </ref> | ||
**Echocardiography is helpful in screening the following cardiac abnormalities: <ref name="pmid29344338">{{cite journal| author=Shankar RK, Backeljauw PF| title=Current best practice in the management of Turner syndrome. | journal=Ther Adv Endocrinol Metab | year= 2018 | volume= 9 | issue= 1 | pages= 33-40 | pmid=29344338 | doi=10.1177/2042018817746291 | pmc=5761955 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29344338 }} </ref> | **Echocardiography is helpful in screening the following cardiac abnormalities: <ref name="pmid29344338">{{cite journal| author=Shankar RK, Backeljauw PF| title=Current best practice in the management of Turner syndrome. | journal=Ther Adv Endocrinol Metab | year= 2018 | volume= 9 | issue= 1 | pages= 33-40 | pmid=29344338 | doi=10.1177/2042018817746291 | pmc=5761955 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29344338 }} </ref> | ||
*#Coarctation of aorta | *#[[Coarctation of aorta]] | ||
*#Ventricular septal defect | *#[[Ventricular septal defect]] | ||
*#Bicuspid aortic valve | *#[[Bicuspid aortic valve]] | ||
*#Aortic dissection | *#[[Aortic dissection]] | ||
*#Aortal dilation | *#[[Aortal dilation]] | ||
*#Aortic aneurysm | *#[[Aortic aneurysm]] | ||
*#Ischemic heart disease | *#[[Ischemic heart disease]] | ||
*#Atherosclerosis | *#[[Atherosclerosis]] | ||
*#Elongated transverse aortic arch | *#[[Elongated transverse aortic arch]] | ||
*#Pulmonary venous anomalies | *#[[Pulmonary venous anomalies]] | ||
*#Hypoplastic left heart syndrome | *#[[Hypoplastic left heart syndrome]] | ||
*#Infective endocarditis | *#[[Infective endocarditis]] | ||
*Renal Ultrasound is helpful in screening the following structural abnormalities: | *[[Renal]] Ultrasound is helpful in screening the following structural abnormalities: | ||
*#Horse shoe shaped kidney | *#[[Horse shoe shaped kidney]] | ||
*#Duplicate ureter | *#[[Duplicate ureter]] | ||
==2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guideline Recommendations: Diagnosis and Management of Patients with Thoracic Aortic Disease (DO NOT EDIT) <ref name="pmid20233780">{{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE et al.| title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. | journal=Circulation | year= 2010 | volume= 121 | issue= 13 | pages= e266-369 | pmid=20233780 | doi=10.1161/CIR.0b013e3181d4739e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20233780 }} </ref>== | ==2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guideline Recommendations: Diagnosis and Management of Patients with Thoracic Aortic Disease (DO NOT EDIT) <ref name="pmid20233780">{{cite journal| author=Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE et al.| title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. | journal=Circulation | year= 2010 | volume= 121 | issue= 13 | pages= e266-369 | pmid=20233780 | doi=10.1161/CIR.0b013e3181d4739e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20233780 }} </ref>== | ||
| Line 53: | Line 53: | ||
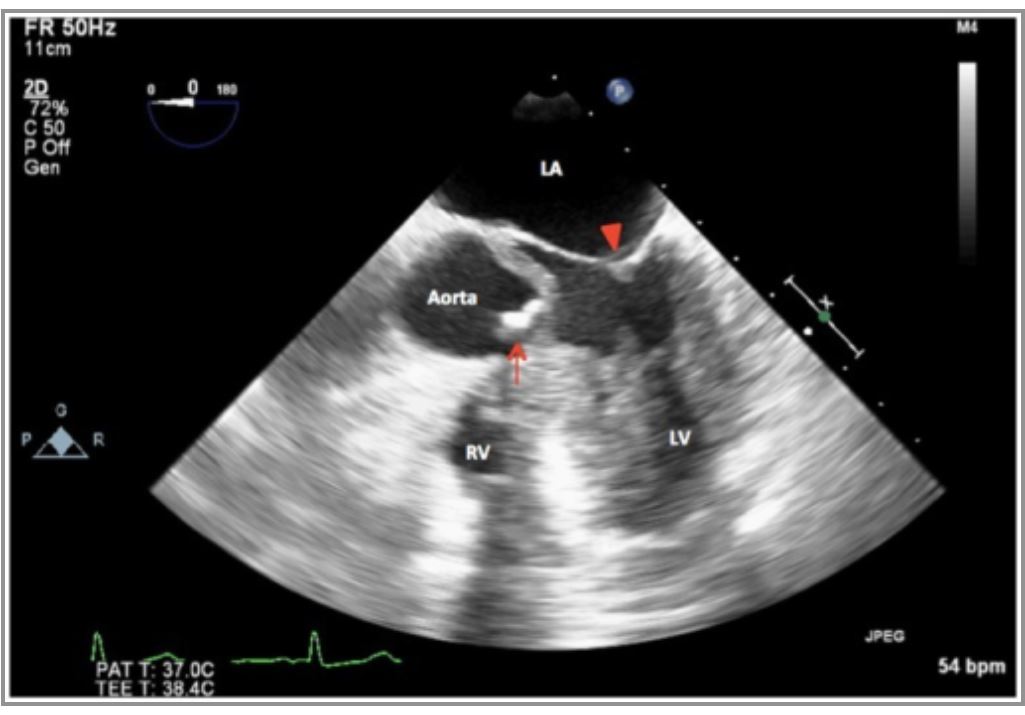
'''Echocardiography showing aortic stenosis in Turner Syndrome''' | '''Echocardiography showing aortic stenosis in Turner Syndrome''' | ||
*Severely calcified and restricted unicuspid aortic valve in systole | *Severely calcified and restricted [[unicuspid aortic valve]] in [[systole]] | ||
*May have occurred secondary to a bicuspid aortic valve. | *May have occurred secondary to a [[bicuspid aortic valve]]. | ||
[[Image: Echo Aortic Stenosis seen in Turner Syndrome.JPG| centre| thumb| 500px |<ref name="pmid26664864">{{cite journal| author=Essandoh M, Castellon-Larios K, Zuleta-Alarcon A, Portillo JG, Crestanello JA| title=Unicuspid Aortic Stenosis in a Patient with Turner Syndrome: A Case Report. | journal=Front Cardiovasc Med | year= 2014 | volume= 1 | issue= | pages= 14 | pmid=26664864 | doi=10.3389/fcvm.2014.00014 | pmc=4668843 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26664864 }} </ref>]] | [[Image: Echo Aortic Stenosis seen in Turner Syndrome.JPG| centre| thumb| 500px |<ref name="pmid26664864">{{cite journal| author=Essandoh M, Castellon-Larios K, Zuleta-Alarcon A, Portillo JG, Crestanello JA| title=Unicuspid Aortic Stenosis in a Patient with Turner Syndrome: A Case Report. | journal=Front Cardiovasc Med | year= 2014 | volume= 1 | issue= | pages= 14 | pmid=26664864 | doi=10.3389/fcvm.2014.00014 | pmc=4668843 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26664864 }} </ref>]] | ||
| Line 61: | Line 61: | ||
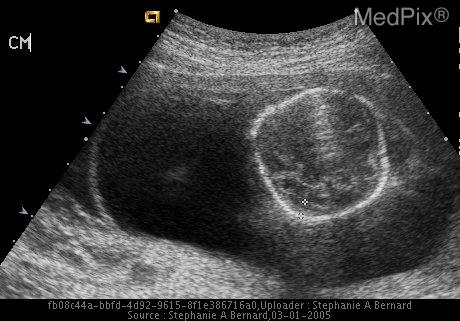
*A dilated cystic like structure is seen on the back of the neck of a 23 year old female. | *A dilated cystic like structure is seen on the back of the neck of a 23 year old female. | ||
*On ultrasound, a cystic hygroma is seen on the posterior aspect of the skull and cervical spine. | *On ultrasound, a [[cystic hygroma]] is seen on the posterior aspect of the [[skull]] and [[cervical spine]]. | ||
[[Image: Ultrasound Cystic Hygroma with hydrops fetalis Turner Syndrome.jpg|thumb|centre|500px| Cystic hygroma in the ammniotic cavity| https://medpix.nlm.nih.gov/topic?id=0a506c76-6043-49ab-8116-a991a8401570]] | [[Image: Ultrasound Cystic Hygroma with hydrops fetalis Turner Syndrome.jpg|thumb|centre|500px| Cystic hygroma in the ammniotic cavity| https://medpix.nlm.nih.gov/topic?id=0a506c76-6043-49ab-8116-a991a8401570]] | ||
Latest revision as of 12:29, 15 September 2020
|
Turner syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Turner syndrome echocardiography and ultrasound On the Web |
|
American Roentgen Ray Society Images of Turner syndrome echocardiography and ultrasound |
|
Risk calculators and risk factors for Turner syndrome echocardiography and ultrasound |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2] Akash Daswaney, M.B.B.S[3]
Overview
Prenatal ultrasounds may show a left-sided cardiac defect, renal anomalies, growth retardation, relatively short limbs, fetal edema, cystic hygroma, polyhydramnios and brachycephaly. Echocardiographies and renal ultrasounds help detect structural defects.
Echocardiography/Ultrasound
- Turner syndrome may be diagnosed or suspected prenatally because of an ultrasonography showing a left-sided cardiac defect, renal anomalies, growth retardation, relatively short limbs, fetal edema, cystic hygroma, polyhydramnios and brachycephaly.
- Echocardiography for cardiac structural abnormalities especially aortic dilation that predisposes the individual to aortic dissection and sudden cardiac death. [1]
- The aortic severity index is a useful prognostic indicator when assessing for the risk of aortic dilatation. [2]
- It is the aortic diameter corrected for body surface area and a score of more than 2.3cm/m2 indicates a high risk of aortic dissection (2-2.3cm/m2 is considered as moderate risk).
- The advice offered to moderate risk patients is restriction of activities and that offered to high risk patients is that they should completely avoid competitive sports and intensive weight training. [3]
- Echocardiography is helpful in screening the following cardiac abnormalities: [3]
- Renal Ultrasound is helpful in screening the following structural abnormalities:
2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guideline Recommendations: Diagnosis and Management of Patients with Thoracic Aortic Disease (DO NOT EDIT) [4]
Aortic Imaging in Genetic Syndromes (DO NOT EDIT) [4]
| Class I |
| "1. Patients with Turner syndrome should undergo imaging of the heart and aorta for evidence of bicuspid aortic valve, coarctation of the aorta, or dilatation of the ascending thoracic aorta. If initial imaging is normal and there are no risk factors for aortic dissection, repeat imaging should be performed every 5 to 10 years or if otherwise clinically indicated. If abnormalities exist, annual imaging or follow-up imaging should be done. (Level of Evidence: C)" |
| Class IIb |
| "1. In patients with Turner syndrome with additional risk factors, including bicuspid aortic valve, coarctation of the aorta, and/or hypertension, and in patients who attempt to become pregnant or who become pregnant, it may be reasonable to perform imaging of the heart and aorta to help determine the risk of aortic dissection. (Level of Evidence: C)" |
Images
Echocardiography showing aortic stenosis in Turner Syndrome
- Severely calcified and restricted unicuspid aortic valve in systole
- May have occurred secondary to a bicuspid aortic valve.
Ultrasound showing a Cystic Hygroma with hydrops fetalis Turner Syndrome
- A dilated cystic like structure is seen on the back of the neck of a 23 year old female.
- On ultrasound, a cystic hygroma is seen on the posterior aspect of the skull and cervical spine.

References
- ↑ Gravholt CH (2005). "Clinical practice in Turner syndrome". Nat Clin Pract Endocrinol Metab. 1 (1): 41–52. doi:10.1038/ncpendmet0024. PMID 16929365.
- ↑ Wolff DJ, Van Dyke DL, Powell CM, Working Group of the ACMG Laboratory Quality Assurance Committee (2010). "Laboratory guideline for Turner syndrome". Genet Med. 12 (1): 52–5. doi:10.1097/GIM.0b013e3181c684b2. PMID 20081420.
- ↑ 3.0 3.1 Shankar RK, Backeljauw PF (2018). "Current best practice in the management of Turner syndrome". Ther Adv Endocrinol Metab. 9 (1): 33–40. doi:10.1177/2042018817746291. PMC 5761955. PMID 29344338.
- ↑ 4.0 4.1 Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE; et al. (2010). "2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine". Circulation. 121 (13): e266–369. doi:10.1161/CIR.0b013e3181d4739e. PMID 20233780.
- ↑ 5.0 5.1 Essandoh M, Castellon-Larios K, Zuleta-Alarcon A, Portillo JG, Crestanello JA (2014). "Unicuspid Aortic Stenosis in a Patient with Turner Syndrome: A Case Report". Front Cardiovasc Med. 1: 14. doi:10.3389/fcvm.2014.00014. PMC 4668843. PMID 26664864.