Toxoplasmosis laboratory findings
|
Toxoplasmosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Toxoplasmosis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Toxoplasmosis laboratory findings |
|
Risk calculators and risk factors for Toxoplasmosis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Toxoplasma infection is diagnosed by the presence of parasite in the fluids such as blood, body fluids, or tissue by DNA amplification, microscopy or by isolation of the organism. The most commonly used diagnostic test is the PCR of the amniotic fluid and a positive test is diagnostic of congenital toxoplasmosis.[1]
Laboratory Findings
Initial tests
| Serological tests | Anti-Toxoplasma IgG | ||
| Anti-Toxoplasma IgM | |||
Interpretation of Serological Tests
| IgG/IgM(ideally performed in the first trimester | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Negative IgG and IgM | Positive IgG Negative IgM | Positive IgM Negative IgG | Positive IgG and IgM | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ No serologic evidence of Toxoplasma infection ❑ Risk of congenital Toxoplasmosis only if the woman aquires infection during the pregnancy ❑ Counsel about the preventive measures for T.gondii | <18 weeks of gestation Infection aquired in the past and prior to the pregnancy ❑ Risk of infection is zero unless the patient is immunocompromised ≥18 weeks of gestation ❑ It is difficult to establish the timing of infection | Repeat IgG and IgM in 1 to 3weeks | Serum should be sent to reference laboratory for confirmatory testing ❑ If the confirmatory test is positive initiate treatment and if negative follow up for 12 months | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Follow up testing is indicated during gestation to detect seroconversion | ≤ 18 weeks of gestation ❑ No further action indicated >18 weeks of gestation ❑ Compare to previous serological tests and send samples to a reference laboratory to confirm the timing of infection | ❑ Negative IgG and Positive IgM ❑ Does not have clinical relevance[2] | ❑ Positive IgG and IgM ❑ Seroconverted and fetus is at risk ❑ Initiate treatment and consider PCR | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table adopted from Management of Toxoplasma gondii Infection during Pregnancy[3]
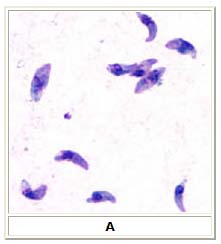
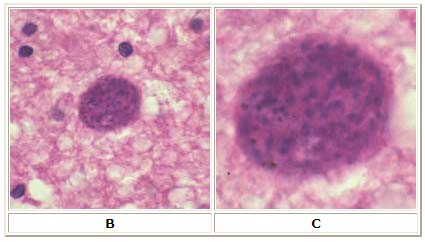
Microscopy
A: Toxoplasma gondii tachyzoites, stained with Giemsa, from a smear of peritoneal fluid obtained from a mouse inoculated with T. gondii. Tachyzoites are typically crescent shaped with a prominent, centrally placed nucleus.
B: Toxoplasma gondii cyst in brain tissue stained with hematoxylin and eosin (100×). C: Zoom of Image B, T. gondii cyst.
References
- ↑ Foulon W, Pinon JM, Stray-Pedersen B, Pollak A, Lappalainen M, Decoster A; et al. (1999). "Prenatal diagnosis of congenital toxoplasmosis: a multicenter evaluation of different diagnostic parameters". Am J Obstet Gynecol. 181 (4): 843–7. PMID 10521739.
- ↑ Liesenfeld O, Press C, Montoya JG, Gill R, Isaac-Renton JL, Hedman K; et al. (1997). "False-positive results in immunoglobulin M (IgM) toxoplasma antibody tests and importance of confirmatory testing: the Platelia Toxo IgM test". J Clin Microbiol. 35 (1): 174–8. PMC 229533. PMID 8968902.
- ↑ Montoya, Jose G.; Remington, Jack S. (2008). "Clinical Practice: Management ofToxoplasma gondiiInfection during Pregnancy". Clinical Infectious Diseases. 47 (4): 554–566. doi:10.1086/590149. ISSN 1058-4838.