Tick-borne disease: Difference between revisions
(→Viral) |
|||
| Line 122: | Line 122: | ||
|style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Tick-borne Meningoencephalitis''' | |style="background: #F5F5F5; padding: 5px; text-align: center;" | '''Tick-borne Meningoencephalitis''' | ||
|style="background: #DCDCDC; padding: 5px;" | ''TBEV virus'' | |style="background: #DCDCDC; padding: 5px;" | ''TBEV virus'' | ||
|style="background: #DCDCDC; padding: 5px;" | | |style="background: #DCDCDC; padding: 5px;" | Ixodes Scapularis, I. Ricinus, I.persulcatus | ||
| style="background: #DCDCDC; padding: 5px;" |'''Widespread:''' | | style="background: #DCDCDC; padding: 5px;" |'''Widespread:''' | ||
*Europe | *Europe | ||
| Line 129: | Line 129: | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Colorado Tick Fever''' | | style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Colorado Tick Fever''' | ||
|style="background: #DCDCDC; padding: 5px;" | ''CTF virus'' | |style="background: #DCDCDC; padding: 5px;" | ''CTF virus'' | ||
|style="background: #DCDCDC; padding: 5px;" | | |style="background: #DCDCDC; padding: 5px;" | ''Dermacentor andersoni'' | ||
|style="background: #DCDCDC; padding: 5px;" | '''United States:''' | |style="background: #DCDCDC; padding: 5px;" | '''United States:''' | ||
*Western Region | *Western Region | ||
| Line 135: | Line 135: | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Crimean-Congo Hemorrhagic Fever''' | | style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Crimean-Congo Hemorrhagic Fever''' | ||
|style="background: #DCDCDC; padding: 5px;" | ''CCHF virus'' | |style="background: #DCDCDC; padding: 5px;" | ''CCHF virus'' | ||
|style="background: #DCDCDC; padding: 5px;" | | |style="background: #DCDCDC; padding: 5px;" | '' Hyalomma marginatum, Rhipicephalus bursa'' | ||
|style="background: #DCDCDC; padding: 5px;" | '''Widespread:''' | |style="background: #DCDCDC; padding: 5px;" | '''Widespread:''' | ||
*South Asia | *South Asia | ||
| Line 143: | Line 143: | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Severe Febrile Illness''' | | style="background: #F5F5F5; padding: 5px; text-align: center;" |'''Severe Febrile Illness''' | ||
|style="background: #DCDCDC; padding: 5px;" | ''Heartland Virus'' | |style="background: #DCDCDC; padding: 5px;" | ''Heartland Virus'' | ||
|style="background: #DCDCDC; padding: 5px;" | | |style="background: #DCDCDC; padding: 5px;" | ''Lone Star Tick (amblyomma americanum)'' | ||
|style="background: #DCDCDC; padding: 5px;" |'''United States:''' | |style="background: #DCDCDC; padding: 5px;" |'''United States:''' | ||
*Missouri | *Missouri | ||
Revision as of 21:25, 28 December 2015
| Tick-borne diseases | |
 | |
|---|---|
| An eschar suggestive of tick bite |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
Overview
Tick-borne diseases are diseases or illnesses transmitted by ticks. As the incidence of tick-borne illnesses increases and the geographic areas in which they are found expand, it becomes increasingly important that health professionals be able to distinguish the diverse, and often overlapping, clinical presentations of these diseases.
Pathophysiology
Tick-borne illnesses are caused by infection with a variety of pathogens, including rickettsia and other types of bacteria, viruses, and protozoa. Because ticks can harbor more than one disease-causing agent, patients can be infected with more than one pathogen at the same time, compounding the difficulty in diagnosis and treatment.
Life Cycle and Spread of Disease
General Tick Life Cycle
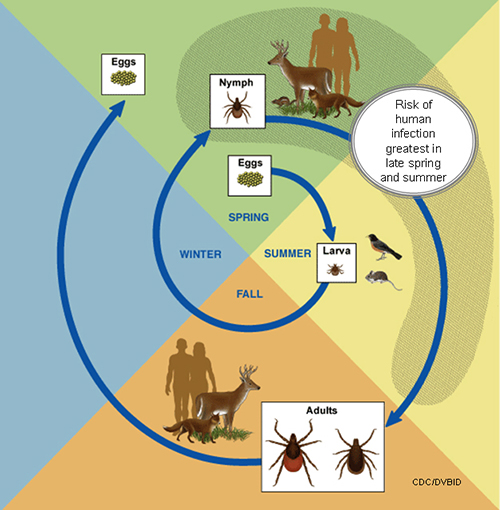
- A tick's life cycle is composed of four stages: hatching(egg), nymph (six legged), nymph (eight legged), and an adult.
- Ticks require blood meal to survive through their life cycle.
- Hosts for tick blood meals include mammals, birds, reptiles, and amphibians. Ticks will most likely transfer between different hosts during the different stages of their life cycle.
- Humans are most often targeted during the nymph and adult stages of the life cycle.
- Life cycle is also dependent on seasonal variation.
- Ticks will go from eggs to larva during the summer months, infecting bird of rodent host during the larval stage.
- Larva will infect the host from the summer until the following spring, at which point they will progress into the nymph stage.
- During the nymph stage, a tick will most likely seek a mammal host (including humans).
- A nymph will remain with the selected host until the following fall at which point it will progress an adult.
- As a adult, a tick will feed on a mammalian host. However unlike previous stages, ticks will prefer larger mammals over rodents.
- The average tick life cycle requires three years for completion.
- Different species will undergo certain variations within their individual life cycles.
Spread of Tick-borne Disease
- Ticks require blood meals in order to progress through their life cycles.
- The average tick requires 10 minutes to 2 hours when preparing a blood meal.
- Once feeding, releases anesthetic properties into its host, via its saliva.
- A feeding tube enters the host followed by an adhesive-like substance, attaching the tick to the host during the blood meal.
- A tick will feed for several days, feeding on the host blood and ingesting the host's pathogens.
- Once feeding is completed, the tick will seek a new host and transfer any pathogens during the next feeding process.
Tick-borne disease Epidemiology and Demographics
Tick-borne disease Classification
Bacterial
| Disease | Organism | Vector | Endemic Regions | |
|---|---|---|---|---|
| Borreliosis (Lyme Disease) | Borrelia burgdorferi sensu lato (bacterium) | Wood Tick (Dermacentor Variabilis), D. andersoni | United States:
| |
| Relapsing Fever | Borrelia Species; Borrelia hermsii, Borellia Parkeri, Borellia duttoni, Borrelia miyamotoi | Ornithodoros species | Widespread:
| |
| Typhus (Diseases associated with the transfer of Rickettsia Bacteria as listed below) | ||||
| Rocky Mountain Spotted Fever | Rickettsia Rickettsii | Wood Tick (Dermacentor Variabilis), D. andersoni | United States:
| |
| Helvetica Spotted Fever | Rickettsia Helvetica | Ixodes Ricinus (European) | Europe:
| |
| Ehrlichiosis Anaplasmosis | Ehrlichia Chaffeensis, E. Equi | Lone Star Tick (Amblyomma Americanum), Ixodes Scapularis | United States:
| |
| Tularemia | Francisella Tularensis | D. Andersoni, D. Variabilis | United States:
| |
Viral
| Disease | Organism | Vector | Endemic Regions |
|---|---|---|---|
| Tick-borne Meningoencephalitis | TBEV virus | Ixodes Scapularis, I. Ricinus, I.persulcatus | Widespread:
|
| Colorado Tick Fever | CTF virus | Dermacentor andersoni | United States:
|
| Crimean-Congo Hemorrhagic Fever | CCHF virus | Hyalomma marginatum, Rhipicephalus bursa | Widespread:
|
| Severe Febrile Illness | Heartland Virus | Lone Star Tick (amblyomma americanum) | United States:
|
Protozoan
| Disease | Organism | Vector | Endemic Regions |
|---|---|---|---|
| Babesiosis | style="font-style: italic;" | Babesia microti, B divergens, B.equi | style="font-style: italic;" | Ixodes Scapularis, I. pacificus | Widespread:
|
Differentiating Tick-Borne Disease
Bacterial
| Disease | Symptoms | Treatment | ||
|---|---|---|---|---|
| Borreliosis (Lyme Disease) | Flu-like illness, fatigue, fever, arthritis, neuroborreliosis, cranial nerve palsy, carditis and erythema migrans. | Antibiotics
or
| ||
| Relapsing Fever | Consistently documented high fevers, flu-like illness, headaches, muscular soreness or joint pain, altered mental state, painful urination, rash, and rigors. | Antibiotics
| ||
| Typhus (Diseases associated with the transfer of Rickettsia Bacteria as listed below) | ||||
| Rocky Mountain Spotted Fever | Fever, alterations in mental state, myalgia, rash, and headaches. | Antibiotics
| ||
| Helvetica Spotted Fever | Rash: spotted, red dots. Respiratory issues, muscle pain, and headaches. | Antibiotics
| ||
| Ehrlichiosis Anaplasmosis | Fever, Headache, Chills, Malaise, Muscle Pain, Nausea, Confusion, Conjunctivitis, or Rash. (60% in children and 30% in adults.) | Antibiotics
| ||
| Tularemia | Ulceroglandular, Glandular, Oculoglandular, Oroglandular, Pneumonic, Typhoidal. | Antibiotics
| ||
Primary method of treatment**
Viral
| Disease | Symptoms | Treatment |
|---|---|---|
| Tick-borne Meningoencephalitis | Early Phase: Non-specific symptoms including fever, malaise, anorexia, muscle pains, headaches, nausea, and vomiting. Second Phase: Meningitis symptoms, headache, stiff neck, encephalitis, drowsiness, sensory disturbances, and potential paralysis. | No specific drug therapy. May require hospitalization and supportive care, including anti-inflammatory drugs, corticosteroids, or, if necessary, incubation and ventilator support. |
| Colorado Tick Fever | Common symptoms include fever, chills, headache, body aches, and lethargy. Other symptoms associated with the disease include sore throat, abdominal pain, vomiting, and a skin rash. A biphasic fever is a hallmark of Colorado Tick Fever and presents itself in nearly 50% of infected patients. | There are no current therapies associated with Colorado Tick Fever. The majority of patients exhibiting symptoms recover completely, however severe cases require hospitalization. |
| Crimean-Congo Hemorrhagic Fever | Initially infected patients will likely feel a few of the following symptoms; headache, high fever, back and joint pain, stomach pain, vomiting, flushed face, red throat petechiae of the palate, and potentially changes in mood as well as sensory perception. | Treatment for Crimean-Congo Hemorrhagic Fever is primarily supportive including balancing electrolytes, oxygen abnormalities, and if necessary, hemodynamic support. In vitro, Crimean-Congo Hemorrhagic Fever is responsive to an antiviral treatment with Ribavirin. |
| Severe Febrile Illness |
Protozoan
| Disease | Symptoms | Treatment |
|---|---|---|
| Babesiosis | Non-specific flu like symptoms. | Atovaquone combined with Azithromycin or Clindamycin combined with Quinine. |
Diagnosis
Physical Examination
A round red rash with a 2-5 mm central black area (eschar, an area of dead tissue)as shown in the photo is suggestive of a tick bite.
Laboratory Findings
In general, specific laboratory tests are not available to rapidly diagnose tick-borne diseases
Risk Factors
People who spend time outdoors and/or have pets that go outdoors are at risk for tick-borne disease.
Treatment
Medical Therapy
If there is a collection of pus, the area will need to be incised and drained. Antibiotic treatment is often justified based on clinical presentation alone. Doxycycline is often used to treat suspected tick borne-disease. Usually one dose is given to cover Lyme disase. An IV dose of a cephalosporin followed by Keflex 500 mg PO q 6 hours is given to treat the surrounding cellulitus. For hospital workers and others who have recently been in the hospital, bactrim twice a day is given to cover Methicillin resistant Staphylococcus Aureus (MRSA).