Tibial plateau fracture pathophysiology: Difference between revisions
(Created page with "__NOTOC__ {{Tibial plateau fracture}} {{CMG}}; {{AE}} {{Rohan}} ==Overview== ==Pathophysiology== *The fracture pattern and severity of comminution depends on multiple...") |
|||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
The pattern of fracture and degree of [[comminution]] are the resultant of several factors or variables such as the nature of [[injury]], the bone quality, the [[age]] and [[weight]] of the patient, the [[energy]] involved, and the position of the [[knee]] and [[leg]] at the time of impact. Various combinations of these variables lead to a variety of different [[Bone fracture|fracture]] patterns. | |||
==Pathophysiology== | ==Pathophysiology== | ||
*The fracture pattern and severity of [[comminution]] depends on multiple factors including: | *The fracture pattern and severity of [[comminution]] depends on multiple factors including:<ref>{{cite book | last = Azar | first = Frederick | title = Campbell's operative orthopaedics | publisher = Elsevier | location = Philadelphia, PA | year = 2017 | isbn = 9780323374620 }}</ref> | ||
**Nature of the fall | **Nature of the fall | ||
**[[Bone]] quality | **[[Bone]] quality | ||
**Age of the patient | **[[Age]] of the patient | ||
**Weight of the patient | **[[Weight]] of the patient | ||
**Energy involved | **[[Energy]] involved | ||
**Position of the [[knee]] and [[leg]] at the time of impact | **Position of the [[knee]] and [[leg]] at the time of impact | ||
* Decrease in bone mass density involves following process:<ref name="pmid23645674">{{cite journal| author=Onal M, Piemontese M, Xiong J, Wang Y, Han L, Ye S et al.| title=Suppression of autophagy in osteocytes mimics skeletal aging. | journal=J Biol Chem | year= 2013 | volume= 288 | issue= 24 | pages= 17432-40 | pmid=23645674 | doi=10.1074/jbc.M112.444190 | pmc=3682543 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23645674 }} </ref> | * Decrease in [[Bone density|bone mass density]] involves following process:<ref name="pmid23645674">{{cite journal| author=Onal M, Piemontese M, Xiong J, Wang Y, Han L, Ye S et al.| title=Suppression of autophagy in osteocytes mimics skeletal aging. | journal=J Biol Chem | year= 2013 | volume= 288 | issue= 24 | pages= 17432-40 | pmid=23645674 | doi=10.1074/jbc.M112.444190 | pmc=3682543 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23645674 }} </ref> | ||
**[[Autophagy]] is the mechanism through which [[Osteocyte|osteocytes]] evade [[oxidative stress]]. | **[[Autophagy]] is the mechanism through which [[Osteocyte|osteocytes]] evade [[oxidative stress]]. | ||
**The capability of [[autophagy]] in cells decreases as they age, a major factor of [[Ageing|aging]]. | **The capability of [[autophagy]] in cells decreases as they age, a major factor of [[Ageing|aging]]. | ||
| Line 23: | Line 23: | ||
{| align="right" | {| align="right" | ||
| | | | ||
[[File:Gray257.png|300px|thumb|Anatomy of tibial plateau.[https://upload.wikimedia.org/wikipedia/commons/8/8b/Gray257.png Source: Case courtesy of Henry Vandyke Carter | [[File:Gray257.png|300px|thumb|Anatomy of tibial plateau.[https://upload.wikimedia.org/wikipedia/commons/8/8b/Gray257.png Source: Case courtesy of Henry Vandyke Carter]]] | ||
|} | |} | ||
*Majority of the weight in the lower leg is transmitted through tibia. | *Majority of the [[weight]] in the [[lower leg]] is transmitted through [[tibia]].<ref>{{cite book | last = Rockwood | first = Charles | title = Rockwood and Green's fractures in adults | publisher = Wolters Kluwer Health/Lippincott Williams & Wilkins | location = Philadelphia, PA | year = 2010 | isbn = 9781605476773 }}</ref><ref>{{cite book | last = Azar | first = Frederick | title = Campbell's operative orthopaedics | publisher = Elsevier | location = Philadelphia, PA | year = 2017 | isbn = 9780323374620 }}</ref> | ||
*The tibial plateau is the proximal portion of the tibia and forms the part of the knee joint. | *The tibial plateau is the [[proximal]] portion of the [[tibia]] and forms the part of the [[knee joint]]. | ||
*The stronger of the two articular surfaces is the medial tibial condyle whereas the lateral tibial condyle is a weaker portion of the joint. | *The stronger of the two [[Articular surface|articular surfaces]] is the medial [[tibial condyle]] whereas the lateral [[tibial condyle]] is a weaker portion of the joint. | ||
*The medial from the lateral tibial condyle are separated by the intercondylar eminence which serves as the attachment for the anterior cruciate ligament (ACL). | *The medial from the lateral [[tibial condyle]] are separated by the intercondylar eminence which serves as the attachment for the [[anterior cruciate ligament]] (ACL). | ||
'''Medial Condyle''' | '''Medial Condyle''' | ||
*The medial condyle is larger than the lateral condyle. | *The medial [[condyle]] is larger than the lateral [[condyle]]. | ||
*The articular surface of medial condyle is oval and it is long axis is anteroposterior. | *The [[articular surface]] of medial [[condyle]] is oval and it is long axis is [[anteroposterior]]. | ||
*The central part of the medial condylar surface is slightly concave. | *The central part of the medial [[Condyle|condylar]] surface is slightly [[concave]]. | ||
*The peripheral part is | *The peripheral part is flat and separated from [[femoral]] [[condyle]] by the medial [[meniscus]]. | ||
'''Lateral Condyle''' | '''Lateral Condyle''' | ||
*The lateral condyle overhangs the shaft of tibia. | *The lateral [[condyle]] overhangs the [[shaft]] of [[tibia]]. | ||
*The articular surface is nearly circular. | *The [[articular surface]] is nearly circular. | ||
*The central part is slightly concave and comes in direct contact with femoral condyle. | *The central part is slightly [[concave]] and comes in direct contact with [[femoral]] [[condyle]]. | ||
*The peripheral part is flat and | *The peripheral part is flat and separated from [[femur]] by the lateral [[meniscus]]. | ||
===Mechanism of Fracture=== | ===Mechanism of Fracture=== | ||
*Proximal tibial injuries can occur due to direct trauma or indirect mechanisms such as axial compression. | *[[Proximal]] [[tibial]] injuries can occur due to direct [[trauma]] or indirect mechanisms such as [[axial]] compression.<ref name="pmid30059369">{{cite journal| author=Ramponi DR, McSwigan T| title=Tibial Plateau Fractures. | journal=Adv Emerg Nurs J | year= 2018 | volume= 40 | issue= 3 | pages= 155-161 | pmid=30059369 | doi=10.1097/TME.0000000000000194 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30059369 }} </ref> | ||
*The causes of most tibial plateau fractures are a valgus stress associated with an axial load. | *The causes of most tibial plateau fractures are a [[valgus]] stress associated with an [[axial]] load. | ||
*Most tibial plateau fractures result from motor vehicle-related injuries followed by sports-associated injuries. | *Most tibial plateau fractures result from motor vehicle-related injuries followed by sports-associated injuries. | ||
*The bumper of a car striking the lateral plateau during this vehicle–pedestrian-related injury causes a valgus mechanism of injury. | *The bumper of a car striking the lateral [[Condyle|plateau]] during this vehicle–pedestrian-related injury causes a [[valgus]] mechanism of injury. | ||
*Motor vehicle injuries are high energy and often result in splitting types of fractures as well as direct injury to the surrounding soft tissues. | *[[Motor vehicle accident|Motor vehicle injuries]] are high energy and often result in splitting types of fractures as well as direct [[injury]] to the surrounding [[Soft tissue|soft tissues]]. | ||
*Low-energy forces can cause a tibial plateau fracture usually in older patients with poor bone quality due to rotational forces. | *Low-energy forces can cause a tibial plateau fracture usually in [[Old age|older]] patients with poor bone quality due to rotational forces. | ||
*Such injuries are primarily seen in women >50 years with osteoporosis resulting in a depressed pattern plateau fracture. | *Such injuries are primarily seen in women >50 years with [[osteoporosis]] resulting in a depressed pattern plateau fracture. | ||
==References== | ==References== | ||
| Line 60: | Line 59: | ||
[[Category:Orthopedics]] | [[Category:Orthopedics]] | ||
[[Category:Orthopedic surgery]] | [[Category:Orthopedic surgery]] | ||
[[Category:Fractures]] | [[Category:Fractures]] | ||
[[Category:Bone fractures]] | [[Category:Bone fractures]] | ||
Latest revision as of 17:10, 10 October 2022
|
Tibial plateau fracture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tibial plateau fracture pathophysiology On the Web |
|
American Roentgen Ray Society Images of Tibial plateau fracture pathophysiology |
|
Risk calculators and risk factors for Tibial plateau fracture pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Overview
The pattern of fracture and degree of comminution are the resultant of several factors or variables such as the nature of injury, the bone quality, the age and weight of the patient, the energy involved, and the position of the knee and leg at the time of impact. Various combinations of these variables lead to a variety of different fracture patterns.
Pathophysiology
- The fracture pattern and severity of comminution depends on multiple factors including:[1]
- Decrease in bone mass density involves following process:[2]
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Anatomy
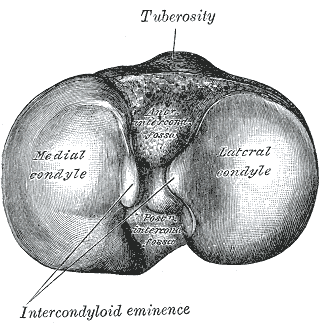 |
- Majority of the weight in the lower leg is transmitted through tibia.[3][4]
- The tibial plateau is the proximal portion of the tibia and forms the part of the knee joint.
- The stronger of the two articular surfaces is the medial tibial condyle whereas the lateral tibial condyle is a weaker portion of the joint.
- The medial from the lateral tibial condyle are separated by the intercondylar eminence which serves as the attachment for the anterior cruciate ligament (ACL).
Medial Condyle
- The medial condyle is larger than the lateral condyle.
- The articular surface of medial condyle is oval and it is long axis is anteroposterior.
- The central part of the medial condylar surface is slightly concave.
- The peripheral part is flat and separated from femoral condyle by the medial meniscus.
Lateral Condyle
- The lateral condyle overhangs the shaft of tibia.
- The articular surface is nearly circular.
- The central part is slightly concave and comes in direct contact with femoral condyle.
- The peripheral part is flat and separated from femur by the lateral meniscus.
Mechanism of Fracture
- Proximal tibial injuries can occur due to direct trauma or indirect mechanisms such as axial compression.[5]
- The causes of most tibial plateau fractures are a valgus stress associated with an axial load.
- Most tibial plateau fractures result from motor vehicle-related injuries followed by sports-associated injuries.
- The bumper of a car striking the lateral plateau during this vehicle–pedestrian-related injury causes a valgus mechanism of injury.
- Motor vehicle injuries are high energy and often result in splitting types of fractures as well as direct injury to the surrounding soft tissues.
- Low-energy forces can cause a tibial plateau fracture usually in older patients with poor bone quality due to rotational forces.
- Such injuries are primarily seen in women >50 years with osteoporosis resulting in a depressed pattern plateau fracture.
References
- ↑ Azar, Frederick (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. ISBN 9780323374620.
- ↑ Onal M, Piemontese M, Xiong J, Wang Y, Han L, Ye S; et al. (2013). "Suppression of autophagy in osteocytes mimics skeletal aging". J Biol Chem. 288 (24): 17432–40. doi:10.1074/jbc.M112.444190. PMC 3682543. PMID 23645674.
- ↑ Rockwood, Charles (2010). Rockwood and Green's fractures in adults. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781605476773.
- ↑ Azar, Frederick (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. ISBN 9780323374620.
- ↑ Ramponi DR, McSwigan T (2018). "Tibial Plateau Fractures". Adv Emerg Nurs J. 40 (3): 155–161. doi:10.1097/TME.0000000000000194. PMID 30059369.