Thymoma pathophysiology
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Thymoma pathophysiology |
|
Risk calculators and risk factors for Thymoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2]
Please help WikiDoc by adding more content here. It's easy! Click here to learn about editing.
Overview
Pathophysiology
Thymoma originates from the epithelial cell population in the thymus. Many subtypes are recognized, some of which have a better- or worse-than-general prognosis.[1]
Histopathology
Thymoma originates from the epithelial cell population in the thymus, and several microscopic subtypes are now recognized.There are three principal histological types of thymoma, depending on the appearance of the cells by microscopy:
- Type A if the epithelial cells have an oval or fusiform shape (less lymphocyte count);
- Type B if they have an epithelioid shape (Type B has three subtypes: B1 (lymphocyte-rich), B2 (cortical) and B3 (epithelial).);
- Type AB if the tumor contains a combination of both cell types.
Thymic cortical epithelial cells have abundant cytoplasm, vesicular nucleus with finely divided chromatin and small nucleoli and cytoplasmic filaments contact adjacent cells. Thymic medullary epithelial cells in contrast are spindle shaped with oval dense nucleus and scant cytoplasm thymoma if recapitulates cortical cell features more, is thought to be less benign.
-
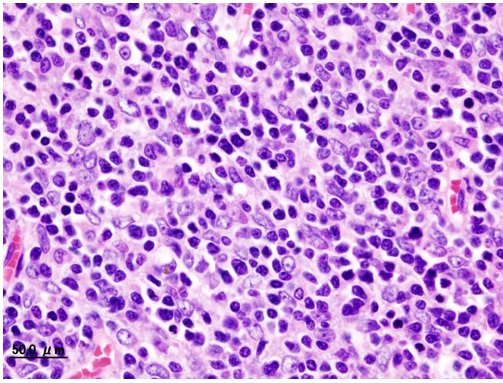
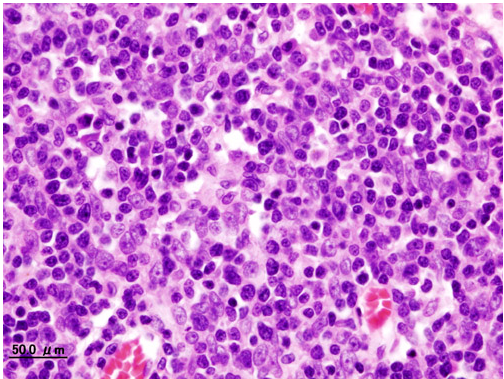
Histopathological image of Thymoma type B1. Anterior mediastinal mass surgically resected. Hematoxylin & eosin stain
-
Histopathological image representing a noninvasive Thymoma type B1, surgically resected. Hematoxylin & eosin
-
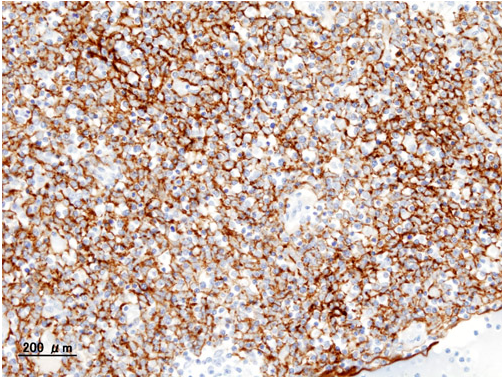
Histopathological image of Thymoma type B1. Anterior mediastinal mass surgically resected. Cytokeratin CAM5.2 immunostain
-
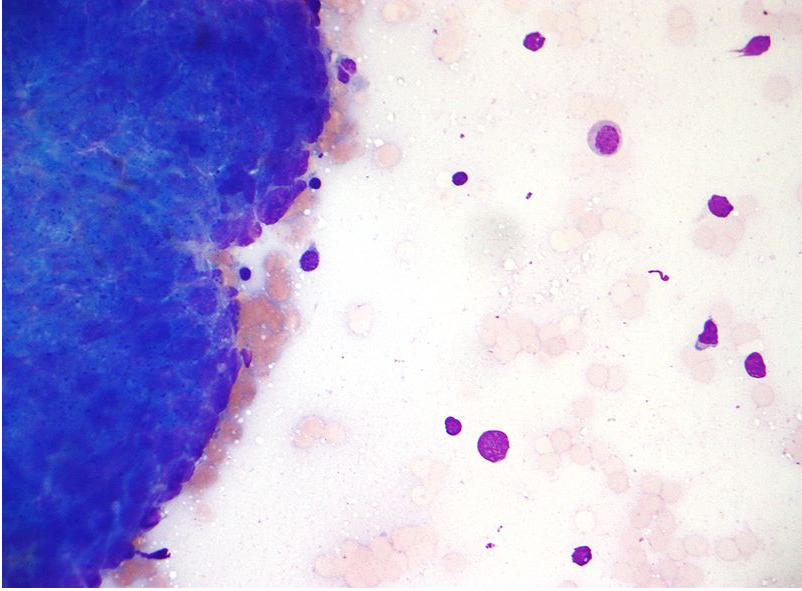
Micrograph of a Thymoma. FNA specimen. Field stain
-
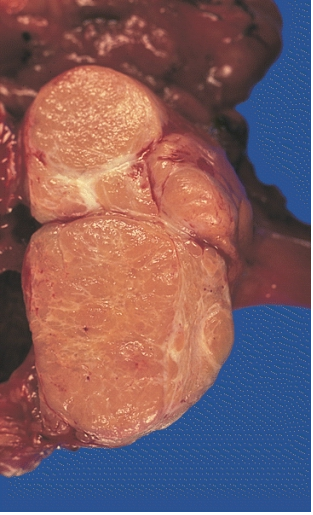
MEDIASTINUM: LOCALLY INVASIVE, CIRCUMSCRIBED THYMOMA (MIXED LYMPHOCYTIC AND EPITHELIAL AND MIXED POLYGONAL AND SPINDLE).Its cut surface bulges, and is pale tan and faintly lobulated. It invaded the capsule at a few points but still remained within the thymus
Associated Disorders
A third of the patients who have a thymoma detected because they have an associated autoimmune disorder. The most common condition in this group is myasthenia gravis (of which 25-50% are associated with a thymoma); patients with myasthenia are routinely screened for thymoma. Other associated autoimmune conditions are pure red cell aplasia and Good's syndrome (thymoma with combined immunodeficiency and hypoimmunoglobulinemia G). Rare associations that have been reported are: acute pericarditis, Addison's disease, agranulocytosis, alopecia areata, ulcerative colitis, Cushing's disease, hemolytic anemia, limbic encephalopathy, myocarditis, nephrotic syndrome, panhypopituitarism, pernicious anemia, polymyositis, rheumatoid arthritis, sarcoidosis, scleroderma, sensorimotor radiculopathy, stiff person syndrome, systemic lupus erythematosus and thyroiditis.[1]
References
- ↑ 1.0 1.1 Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 17 (7): 2280–9. PMID 10561285. Retrieved 2012-01-18. Unknown parameter
|month=ignored (help)