Tabes Dorsalis physical examination
|
Tabes Dorsalis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tabes Dorsalis physical examination On the Web |
|
American Roentgen Ray Society Images of Tabes Dorsalis physical examination |
|
Risk calculators and risk factors for Tabes Dorsalis physical examination |
Physical Examination
Physical examination may show:
- Damage to the spinal cord (myelopathy)
- Pupils that react abnormally to light
- Reduced or absent reflexes due to nerve damage
References
s s s s
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Mohamadmostafa Jahansouz M.D.[2]
Overview
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Physical Examination
- Physical examination of patients with [disease name] is usually normal.
OR
- Physical examination of patients with [disease name] is usually remarkable for:[finding 1], [finding 2], and [finding 3].
- The presence of [finding(s)] on physical examination is diagnostic of [disease name].
- The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Appearance of the Patient
- Patients with [disease name] usually appear [general appearance].
Vital Signs
- Usually vital ital signs are normal in tabes dorsal.[1]
Skin
- In patients with tabes dorsalis some granulomatous skin lesions which are one of the late manifestations of tertiary syphilis called gumma may be present. Gummas, are granulomatous reactions to long-term smoldering infection with Treponema pallidum and its residual antigens.[2]
- Jaundice may be seen.
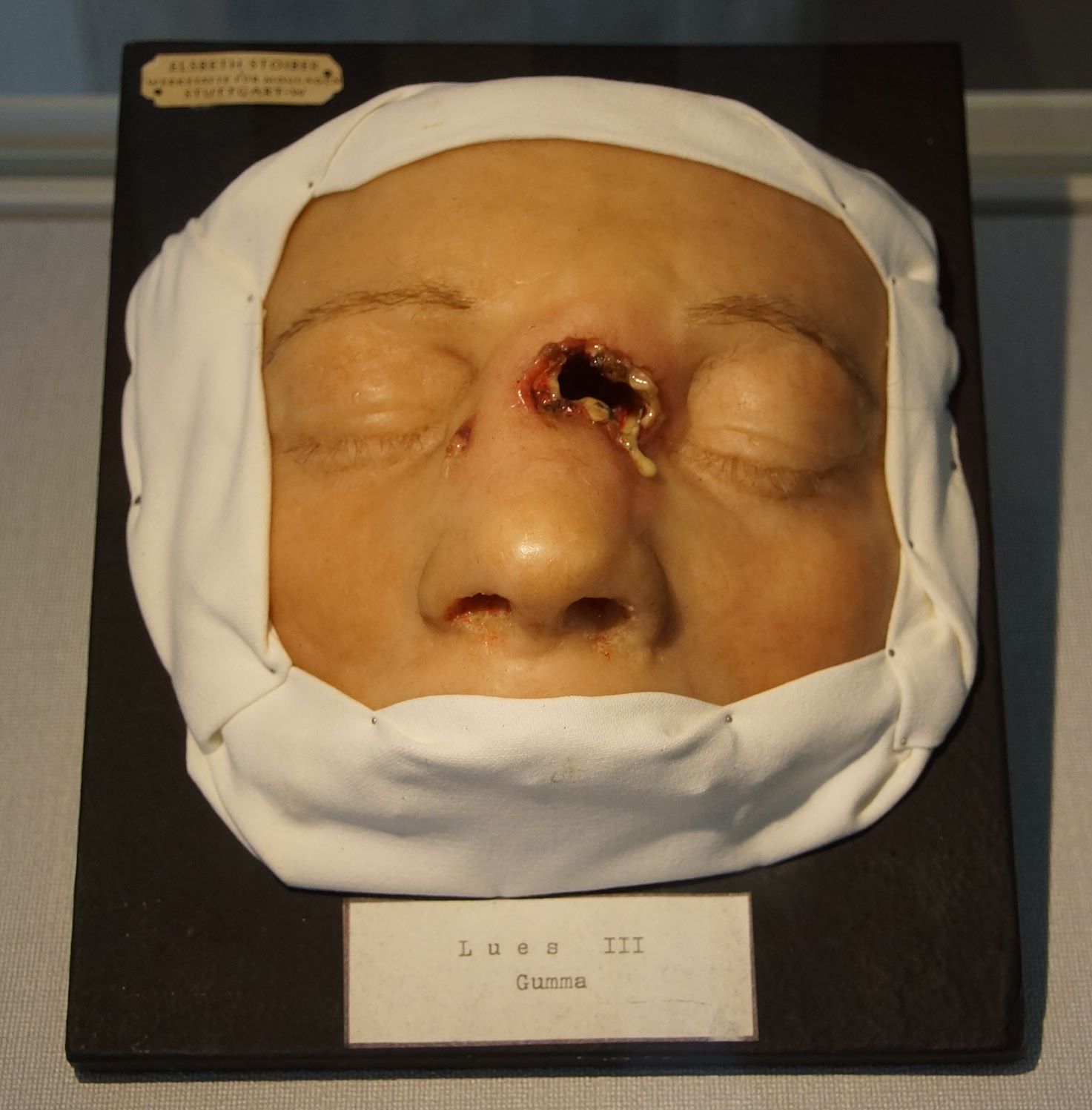
Source:By NearEMPTiness (Wie Schönes Wissen schafft im MUT) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons, rID: 51340
HEENT
- Abnormalities of the head/hair may include:[3]
- Icteric sclera may be present
- Argyll Robertson pupils may be present
- Hearing acuity may be reduced[4]
Neck
- Nontender, mobile, small, cervical lymphadenopathy may be present
Lungs
- In patients with tabes dorsalis some granulomatous lung lesions which are one of the late manifestations of tertiary syphilis called gumma may be present. Gummas, are granulomatous reactions to long-term smoldering infection with Treponema pallidum and its residual antigens.[5]
- Bilaterally coarse crackles upon auscultation of the lung may be present
Neuromuscular
- Positive romberg sign is one of the most important findings in physical examination of patients with tabes dorsalis[6]
- Patient is usually oriented to persons, place, and time
- Altered mental status may be present
- Hhyporeflexia or areflexia may be seen[7]
- Impaired balance bilateral Babinski's Reflex may be present[8]
- Bilateral muscle weakness mostly in lower limbs may be seen[9]
- Argyll Robertson pupils may be present[3]
- Bilateral sensory loss in the extremity mostly in lower limbs may be seen[1]
- broad base gate and Sensory ataxic gait is usually seen in patients with tabes dorsalis[1]
- Cranial nerve palsy caused by gummatous neurosyphilis may be seen[10]
- Finger-to-nose test is usually abnormal[11]
Extremities
- Extremities examination of patients with [disease name] is usually normal.
OR
- Clubbing
- Cyanosis
- Pitting/non-pitting edema of the upper/lower extremities
- Muscle atrophy
- Fasciculations in the upper/lower extremity
References
- ↑ 1.0 1.1 1.2 Tso MK, Koo K, Tso GY (2008). "Neurosyphilis in a non-HIV patient: more than a psychiatric concern". Mcgill J Med. 11 (2): 160–3. PMC 2582679. PMID 19148316.
- ↑ Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ 3.0 3.1 Thompson HS, Kardon RH (2006). "The Argyll Robertson pupil". J Neuroophthalmol. 26 (2): 134–8. doi:10.1097/01.wno.0000222971.09745.91. PMID 16845316.
- ↑ Nadol JB (1975). "Hearing loss of acquired syphilis: diagnosis confirmed by incudectomy". Laryngoscope. 85 (11 pt 1): 1888–97. doi:10.1288/00005537-197511000-00012. PMID 1195972.
- ↑ MORGAN AD, LLOYD WE, PRICE-THOMAS C (1952). "Tertiary syphilis of the lung and its diagnosis". Thorax. 7 (2): 125–33. PMC 1019150. PMID 14931376.
- ↑ French P (2007). "Syphilis". BMJ. 334 (7585): 143–7. doi:10.1136/bmj.39085.518148.BE. PMC 1779891. PMID 17235095.
- ↑ Pandey S (2011). "Magnetic resonance imaging of the spinal cord in a man with tabes dorsalis". J Spinal Cord Med. 34 (6): 609–11. doi:10.1179/2045772311Y.0000000041. PMC 3237288. PMID 22330117.
- ↑ Ahamed S, Varghese M, El Agib el N, Ganesa VS, Aysha M (2009). "Case of neurosyphilis presented as recurrent stroke". Oman Med J. 24 (2): 134–6. doi:10.5001/omj.2009.29. PMC 3273935. PMID 22334859.
- ↑ Matijosaitis V, Vaitkus A, Pauza V, Valiukeviciene S, Gleizniene R (2006). "Neurosyphilis manifesting as spinal transverse myelitis". Medicina (Kaunas). 42 (5): 401–5. PMID 16778468.
- ↑ Vogl T, Dresel S, Lochmüller H, Bergman C, Reimers C, Lissner J (1993). "Third cranial nerve palsy caused by gummatous neurosyphilis: MR findings". AJNR Am J Neuroradiol. 14 (6): 1329–31. PMID 8279327.
- ↑ Mehrabian S, Raycheva MR, Petrova EP, Tsankov NK, Traykov LD (2009). "Neurosyphilis presenting with dementia, chronic chorioretinitis and adverse reactions to treatment: a case report". Cases J. 2: 8334. doi:10.4076/1757-1626-2-8334. PMC 2769430. PMID 19918420.