Sumatriptan (injection): Difference between revisions
No edit summary |
No edit summary |
||
| Line 107: | Line 107: | ||
7.4 Selective Serotonin Reuptake Inhibitors/Serotonin Norepinephrine Reuptake Inhibitors and Serotonin Syndrome | 7.4 Selective Serotonin Reuptake Inhibitors/Serotonin Norepinephrine Reuptake Inhibitors and Serotonin Syndrome | ||
Cases of serotonin syndrome have been reported during coadministration of triptans and SSRIs, or SNRIs, TCAs, and MAO inhibitors [see Warnings and Precautions (5.7)]. | Cases of serotonin syndrome have been reported during coadministration of triptans and SSRIs, or SNRIs, TCAs, and MAO inhibitors [see Warnings and Precautions (5.7)]. | ||
|FDAPregCat=C | |||
|useInPregnancyFDA=There are no adequate and well-controlled trials of IMITREX Injection in pregnant women. IMITREX Injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | |||
When sumatriptan was administered intravenously to pregnant rabbits daily throughout the period of organogenesis, embryolethality was observed at doses at or close to those producing maternal toxicity. These doses were less than the maximum recommended human dose (MRHD) of 12 mg/day on a mg/m2 basis. Oral administration of sumatriptan to rabbits during organogenesis was associated with increased incidences of fetal vascular and skeletal abnormalities. The highest no-effect dose for these effects was 15 mg/kg/day. The intravenous administration of sumatriptan to pregnant rats throughout organogenesis at doses that are approximately 10 times the MRHD on a mg/m2 basis, did not produce evidence of embryolethality. The subcutaneous administration of sumatriptan to pregnant rats prior to and throughout pregnancy did not produce evidence of embryolethality or teratogenicity. | |||
|useInNursing=It is not known whether sumatriptan is excreted in human breast milk following subcutaneous administration. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from IMITREX, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. | |||
|useInPed=Safety and effectiveness of IMITREX Injection in pediatric patients under 18 years of age have not been established; therefore, IMITREX Injection is not recommended for use in patients under 18 years of age. | |||
Two controlled clinical trials evaluated IMITREX Nasal Spray (5 to 20 mg) in 1,248 adolescent migraineurs aged 12 to 17 years who treated a single attack. The trials did not establish the efficacy of IMITREX Nasal Spray compared with placebo in the treatment of migraine in adolescents. Adverse reactions observed in these clinical trials were similar in nature to those reported in clinical trials in adults. | |||
Five controlled clinical trials (2 single-attack trials, 3 multiple-attack trials) evaluating oral IMITREX (25 to 100 mg) in pediatric subjects aged 12 to 17 years enrolled a total of 701 adolescent migraineurs. These trials did not establish the efficacy of oral IMITREX compared with placebo in the treatment of migraine in adolescents. Adverse reactions observed in these clinical trials were similar in nature to those reported in clinical trials in adults. The frequency of all adverse reactions in these subjects appeared to be both dose- and age-dependent, with younger subjects reporting reactions more commonly than older adolescents. | |||
Postmarketing experience documents that serious adverse reactions have occurred in the pediatric population after use of subcutaneous, oral, and/or intranasal IMITREX. These reports include reactions similar in nature to those reported rarely in adults, including stroke, visual loss, and death. A myocardial infarction has been reported in a 14-year-old male following the use of oral IMITREX; clinical signs occurred within 1 day of drug administration. Since clinical data to determine the frequency of serious adverse reactions in pediatric patients who might receive subcutaneous, oral, or intranasal IMITREX are not presently available, the use of IMITREX in patients under 18 years of age is not recommended. | |||
|useInGeri=Clinical trials of IMITREX Injection did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. | |||
A cardiovascular evaluation is recommended for geriatric patients who have other cardiovascular risk factors (e.g., diabetes, hypertension, smoking, obesity, strong family history of CAD) prior to receiving IMITREX Injection [see Warnings and Precautions (5.1)]. | |||
|overdose=No gross overdoses in clinical practice have been reported. Coronary vasospasm was observed after intravenous administration of IMITREX Injection [see Contraindications (4)]. Overdoses would be expected from animal data (dogs at 0.1 g/kg, rats at 2 g/kg) to possibly cause convulsions, tremor, inactivity, erythema of the extremities, reduced respiratory rate, cyanosis, ataxia, mydriasis, injection site reactions (desquamation, hair loss, and scab formation), and paralysis. | |||
The elimination half-life of sumatriptan is about 2 hours [see Clinical Pharmacology (12.3)], and therefore monitoring of patients after overdose with IMITREX Injection should continue for at least 10 hours or while symptoms or signs persist. | |||
It is unknown what effect hemodialysis or peritoneal dialysis has on the serum concentrations of sumatriptan. | |||
|drugBox={{Drugbox2 | |||
| Watchedfields = changed | |||
| verifiedrevid = 477173943 | |||
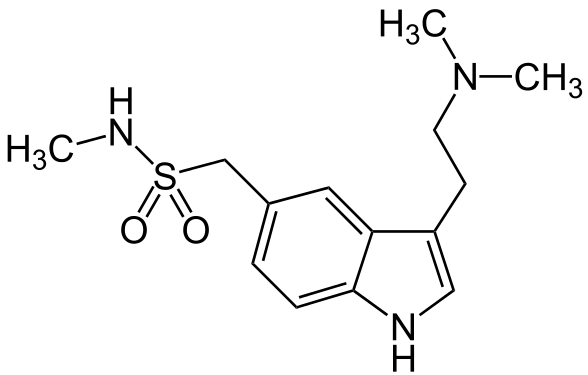
| IUPAC_name = 1-[3-(2-Dimethylaminoethyl)-1''H''-indol-5-yl]-''N''-methyl-methanesulfonamide | |||
| image = Sumatriptan_Structural_Formula_V.1.png | |||
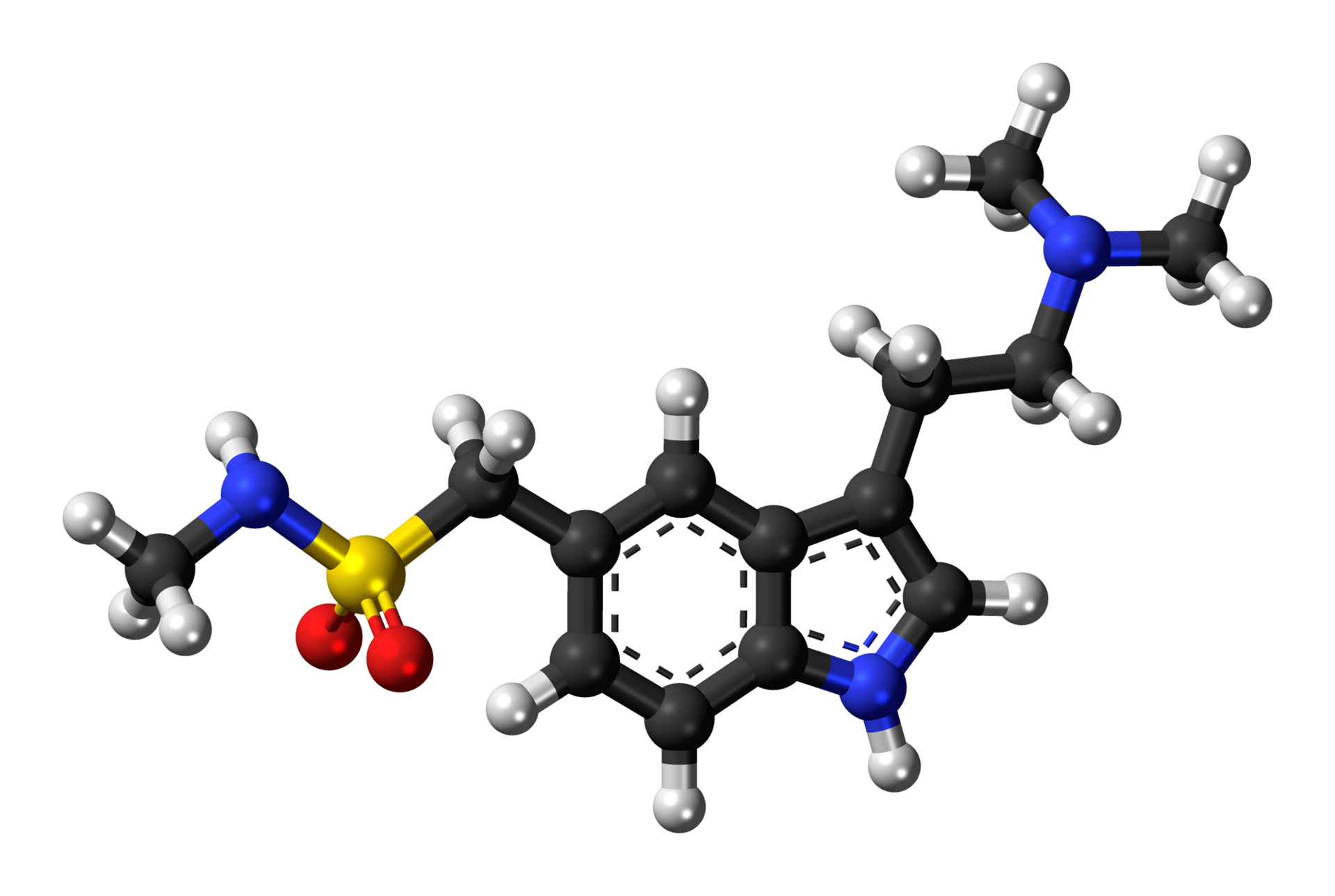
| image2 = Sumatriptan-3D-balls.png | |||
| alt2 = Sumatriptan molecule | |||
<!--Clinical data--> | |||
| tradename = Imitrex, Imigran,Treximet | |||
| Drugs.com = {{drugs.com|monograph|sumatriptan}} | |||
| licence_US = Sumatriptan | |||
| pregnancy_category = C | |||
| legal_AU = <!-- S2, S3, S4, S5, S6, S7, S8, S9 or Unscheduled--> | |||
| legal_CA = <!-- OTC, Rx-only, Schedule I, II, III, IV, V, VI, VII, VIII --> | |||
| legal_UK = <!-- GSL, P, POM, CD, CD Lic, CD POM, CD No Reg POM, CD (Benz) POM, CD (Anab) POM or CD Inv POM --> | |||
| legal_US = Rx-only | |||
| routes_of_administration = tablet, subcutaneous injection, nasal spray | |||
<!--Pharmacokinetic data--> | |||
| bioavailability = 15% (oral)/ 96% (s.c) | |||
| protein_bound = 14–21% | |||
| metabolism = [[Monoamine oxidase|MAO]] | |||
| elimination_half-life = 2.5 hours | |||
| excretion = 60% [[urine]]; 40% [[feces]] | |||
<!--Identifiers--> | |||
| CASNo_Ref = {{cascite|correct|CAS}} | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 103628-46-2 | |||
| ATC_prefix = N02 | |||
| ATC_suffix = CC01 | |||
| PubChem = 5358 | |||
| IUPHAR_ligand = 54 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00669 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 5165 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = 8R78F6L9VO | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D00451 | |||
| ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| ChEBI = 10650 | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 128 | |||
<!--Chemical data--> | |||
| C=14 | H=21 | N=3 | O=2 | S=1 | |||
| molecular_weight = 295.402 g/mol | |||
| smiles = O=S(=O)(NC)Cc1cc2c(cc1)ncc2CCN(C)C | |||
| InChI = 1/C14H21N3O2S/c1-15-20(18,19)10-11-4-5-14-13(8-11)12(9-16-14)6-7-17(2)3/h4-5,8-9,15-16H,6-7,10H2,1-3H3 | |||
| InChIKey = KQKPFRSPSRPDEB-UHFFFAOYAF | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C14H21N3O2S/c1-15-20(18,19)10-11-4-5-14-13(8-11)12(9-16-14)6-7-17(2)3/h4-5,8-9,15-16H,6-7,10H2,1-3H3 | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = KQKPFRSPSRPDEB-UHFFFAOYSA-N | |||
}} | |||
|mechAction=Sumatriptan binds with high affinity to human cloned 5-HT1B/1D receptors. IMITREX presumably exerts its therapeutic effects in the treatment of migraine headache by binding to 5-HT1B/1D receptors located on intracranial blood vessels and sensory nerves of the trigeminal system. | |||
Current theories proposed to explain the etiology of migraine headache suggest that symptoms are due to local cranial vasodilatation and/or to the release of sensory neuropeptides (including substance P and calcitonin gene-related peptide) through nerve endings in the trigeminal system. The therapeutic activity of IMITREX for the treatment of migraine and cluster headaches is thought to be due to the agonist effects at the 5-HT1B/1D receptors on intracranial blood vessels (including the arterio-venous anastomoses) and sensory nerves of the trigeminal system, which result in cranial vessel constriction and inhibition of pro-inflammatory neuropeptide release. | |||
|structure=IMITREX Injection contains sumatriptan succinate, a selective 5-HT1B/1D receptor agonist. Sumatriptan succinate is chemically designated as 3-[2-(dimethylamino)ethyl]-N-methyl-indole-5-methanesulfonamide succinate (1:1), and it has the following structure: | |||
[[File:IMITREXn2.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
The empirical formula is C14H21N3O2S•C4H6O4, representing a molecular weight of 413.5. Sumatriptan succinate is a white to off-white powder that is readily soluble in water and in saline. | |||
IMITREX Injection is a clear, colorless to pale yellow, sterile, nonpyrogenic solution for subcutaneous injection. Each 0.5 mL of IMITREX Injection 8 mg/mL solution contains 4 mg of sumatriptan (base) as the succinate salt and 3.8 mg of sodium chloride, USP in Water for Injection, USP. Each 0.5 mL of IMITREX Injection 12 mg/mL solution contains 6 mg of sumatriptan (base) as the succinate salt and 3.5 mg of sodium chloride, USP in Water for Injection, USP. The pH range of both solutions is approximately 4.2 to 5.3. The osmolality of both injections is 291 mOsmol. | |||
|PD=Blood Pressure: Significant elevation in blood pressure, including hypertensive crisis, has been reported in patients with and without a history of hypertension [see Warnings and Precautions (5.8)]. | |||
Peripheral (Small) Arteries: In healthy volunteers (N = 18), a trial evaluating the effects of sumatriptan on peripheral (small vessel) arterial reactivity failed to detect a clinically significant increase in peripheral resistance. | |||
Heart Rate: Transient increases in blood pressure observed in some subjects in clinical trials carried out during sumatriptan’s development as a treatment for migraine were not accompanied by any clinically significant changes in heart rate. | |||
|PK=Absorption and Bioavailability: The bioavailability of sumatriptan via subcutaneous site injection to 18 healthy male subjects was 97% ± 16% of that obtained following intravenous injection. | |||
After a single 6-mg subcutaneous manual injection into the deltoid area of the arm in 18 healthy males (age: 24 ± 6 years, weight: 70 kg), the maximum serum concentration (Cmax) of sumatriptan was (mean ± standard deviation) 74 ± 15 ng/mL and the time to peak concentration (Tmax) was 12 minutes after injection (range: 5 to 20 minutes). In this trial, the same dose injected subcutaneously in the thigh gave a Cmax of 61 ± 15 ng/mL by manual injection versus 52 ± 15 ng/mL by autoinjector techniques. The Tmax or amount absorbed was not significantly altered by either the site or technique of injection. | |||
Distribution: Protein binding, determined by equilibrium dialysis over the concentration range of 10 to 1,000 ng/mL, is low, approximately 14% to 21%. The effect of sumatriptan on the protein binding of other drugs has not been evaluated. | |||
Following a 6-mg subcutaneous injection into the deltoid area of the arm in 9 males (mean age: 33 years, mean weight: 77 kg) the volume of distribution central compartment of sumatriptan was 50 ± 8 liters and the distribution half‑life was 15 ± 2 minutes. | |||
Metabolism: In vitro studies with human microsomes suggest that sumatriptan is metabolized by MAO, predominantly the A isoenzyme. Most of a radiolabeled dose of sumatriptan excreted in the urine is the major metabolite indole acetic acid (IAA) or the IAA glucuronide, both of which are inactive. | |||
Elimination: After a single 6-mg subcutaneous dose, 22% ± 4% was excreted in the urine as unchanged sumatriptan and 38% ± 7% as the IAA metabolite. | |||
Following a 6-mg subcutaneous injection into the deltoid area of the arm, the systemic clearance of sumatriptan was 1,194 ± 149 mL/min and the terminal half-life was 115 ± 19 minutes. | |||
Special Populations:Age: The pharmacokinetics of sumatriptan in the elderly (mean age: 72 years, 2 males and 4 females) and in subjects with migraine (mean age: 38 years, 25 males and 155 females) were similar to that in healthy male subjects (mean age: 30 years). | |||
Renal Impairment: The effect of renal impairment on the pharmacokinetics of sumatriptan has not been examined. | |||
Hepatic Impairment: The effect of mild to moderate hepatic disease on the pharmacokinetics of subcutaneously administered sumatriptan has been evaluated. There were no significant differences in the pharmacokinetics of subcutaneously administered sumatriptan in moderately hepatically impaired subjects compared with healthy controls. The pharmacokinetics of subcutaneously administered sumatriptan in patients with severe hepatic impairment has not been studied. The use of IMITREX Injection in this population is contraindicated [see Contraindications (4)]. | |||
Race: The systemic clearance and Cmax of sumatriptan were similar in black (n = 34) and Caucasian (n = 38) healthy male subjects. | |||
Drug Interaction Studies: Monoamine Oxidase-A Inhibitors:In a trial of 14 healthy females, pretreatment with an MAO-A inhibitor decreased the clearance of sumatriptan, resulting in a 2-fold increase in the area under the sumatriptan plasma concentration-time curve (AUC), corresponding to a 40% increase in elimination half-life. | |||
|nonClinToxic=13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility | |||
Carcinogenesis: In carcinogenicity studies, rats and mice were given sumatriptan by oral gavage. Mice were dosed for 78 weeks and rats were dosed for 104 weeks. Average exposures achieved in mice receiving the highest dose were approximately 110 times the exposure attained in humans after the maximum recommended single dose of 6 mg. The highest dose to rats was approximately 260 times the maximum single dose of 6 mg on a mg/m2 basis. There was no evidence of an increase in tumors in either species related to sumatriptan administration. | |||
Mutagenesis: Sumatriptan was not mutagenic in the presence or absence of metabolic activation when tested in 2 gene mutation assays (the Ames test and the in vitro mammalian Chinese hamster V79/HGPRT assay). It was not clastogenic in 2 cytogenetics assays (the in vitro human lymphocyte assay and the in vivo rat micronucleus assay). | |||
Impairment of Fertility: A fertility study (Segment I) by the subcutaneous route, during which male and female rats were dosed daily with sumatriptan prior to and throughout the mating period, has shown no evidence of impaired fertility at doses equivalent to approximately 100 times the maximum recommended single human dose of 6 mg on a mg/m2 basis. However, following oral administration, a treatment-related decrease in fertility, secondary to a decrease in mating, was seen for rats treated with 50 and 500 mg/kg/day. The no-effect dose for this finding was approximately 8 times the maximum recommended single human dose of 6 mg on a mg/m2 basis. It is not clear whether the problem is associated with the treatment of males or females or both. | |||
13.2 Animal Toxicology and/or Pharmacology | |||
Corneal Opacities: Dogs receiving oral sumatriptan developed corneal opacities and defects in the corneal epithelium. Corneal opacities were seen at the lowest dosage tested, 2 mg/kg/day, and were present after 1 month of treatment. Defects in the corneal epithelium were noted in a 60-week study. Earlier examinations for these toxicities were not conducted and no-effect doses were not established; however, the relative exposure at the lowest dose tested was approximately 5 times the human exposure after a 100-mg oral dose or 3 times the human exposure after a 6-mg subcutaneous dose. | |||
Melanin Binding: In rats with a single subcutaneous dose (0.5 mg/kg) of radiolabeled sumatriptan, the elimination half-life of radioactivity from the eye was 15 days, suggesting that sumatriptan and its metabolites bind to the melanin of the eye. The clinical significance of this binding is unknown. | |||
|alcohol=Alcohol-Sumatriptan (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Sumatriptan (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 13:03, 13 May 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Sumatriptan (injection) is {{{aOrAn}}} {{{drugClass}}} that is FDA approved for the treatment of {{{indication}}}. Common adverse reactions include {{{adverseReactions}}}.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
IMITREX® Injection is indicated in adults for (1) the acute treatment of migraine, with or without aura, and (2) the acute treatment of cluster headache.
Limitations of Use:
Use only if a clear diagnosis of migraine or cluster headache has been established. If a patient has no response to the first migraine attack treated with IMITREX, reconsider the diagnosis of migraine before IMITREX is administered to treat any subsequent attacks. IMITREX is not indicated for the prevention of migraine attacks.
Dosage
2.1 Dosing Information The maximum single recommended adult dose of IMITREX Injection for the acute treatment of migraine or cluster headache is 6 mg injected subcutaneously. For the treatment of migraine, if side effects are dose limiting, lower doses (1 to 5 mg) may be used [see Clinical Studies (14.1)]. For the treatment of cluster headache, the efficacy of lower doses has not been established.
The maximum cumulative dose that may be given in 24 hours is 12 mg, two 6-mg injections separated by at least 1 hour. A second 6-mg dose should only be considered if some response to a first injection was observed.
2.2 Administration Using the IMITREX STATdose Pen ® An autoinjector device (IMITREX STATdose Pen) is available for use with 4- and 6-mg prefilled syringe cartridges. With this device, the needle penetrates approximately 1/4 inch (5 to 6 mm). The injection is intended to be given subcutaneously, and intramuscular or intravascular delivery must be avoided. Instruct patients on the proper use of IMITREX STATdose Pen and direct them to use injection sites with an adequate skin and subcutaneous thickness to accommodate the length of the needle.
2.3 Administration of Doses of IMITREX Other Than 4 or 6 mg In patients receiving doses other than 4 or 6 mg, use the 6-mg single-dose vial; do not use the IMITREX STATdose Pen. Visually inspect the vial for particulate matter and discoloration before administration. Do not use if particulates and discolorations are noted.
Dosage Forms and Strengths
- Injection: 4- and 6-mg single-dose prefilled syringe cartridges for use with the IMITREX STATdose Pen
Injection: 6-mg single-dose vial
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sumatriptan (injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sumatriptan (injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Sumatriptan (injection) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sumatriptan (injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sumatriptan (injection) in pediatric patients.
Contraindications
IMITREX Injection is contraindicated in patients with:
Ischemic coronary artery disease (CAD) (angina pectoris, history of myocardial infarction, or documented silent ischemia) or coronary artery vasospasm, including Prinzmetal’s angina [see Warnings and Precautions (5.1)]. Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders [see Warnings and Precautions (5.2)]. History of stroke or transient ischemic attack (TIA) because these patients are at a higher risk of stroke [see Warnings and Precautions (5.4)]. History of hemiplegic or basilar migraine. Peripheral vascular disease [see Warnings and Precautions (5.5)]. Ischemic bowel disease [see Warnings and Precautions (5.5)]. Uncontrolled hypertension [see Warnings and Precautions (5.8)]. Recent (i.e., within 24 hours) use of ergotamine-containing medication, ergot-type medication (such as dihydroergotamine or methysergide), or another 5-hydroxytryptamine 1 (5-HT 1) agonist [see Drug Interactions (7.1, 7.3)]. Concurrent administration of an MAO-A inhibitor or recent (within 2 weeks) use of an MAO-A inhibitor [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)]. Known hypersensitivity to sumatriptan [see Warnings and Precautions (5.9) and Adverse Reactions (6.2)]. Severe hepatic impairment [see Clinical Pharmacology (12.3)].
Warnings
5.1 Myocardial Ischemia, Myocardial Infarction, and Prinzmetal’s Angina The use of IMITREX Injection is contraindicated in patients with ischemic or vasospastic CAD. There have been rare reports of serious cardiac adverse reactions, including acute myocardial infarction, occurring within a few hours following administration of IMITREX Injection. Some of these reactions occurred in patients without known CAD. 5-HT1 agonists, including IMITREX Injection, may cause coronary artery vasospasm (Prinzmetal’s angina), even in patients without a history of CAD.
Perform a cardiovascular evaluation in triptan-naive patients who have multiple cardiovascular risk factors (e.g., increased age, diabetes, hypertension, smoking, obesity, strong family history of CAD) prior to receiving IMITREX Injection. If there is evidence of CAD or coronary artery vasospasm, IMITREX Injection is contraindicated. For patients with multiple cardiovascular risk factors who have a negative cardiovascular evaluation, consider administering the first dose of IMITREX Injection in a medically supervised setting and performing an electrocardiogram (ECG) immediately following IMITREX Injection. For such patients, consider periodic cardiovascular evaluation in intermittent long-term users of IMITREX Injection.
Evaluate patients with signs or symptoms suggestive of angina following IMITREX Injection for the presence of CAD or Prinzmetal’s angina before receiving additional doses of IMITREX Injection.
5.2 Arrhythmias Life-threatening disturbances of cardiac rhythm, including ventricular tachycardia and ventricular fibrillation leading to death, have been reported within a few hours following the administration of 5-HT1 agonists. Discontinue IMITREX Injection if these disturbances occur. IMITREX Injection is contraindicated in patients with Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders.
5.3 Chest, Throat, Neck, and/or Jaw Pain/Tightness/Pressure As with other 5-HT1 agonists, sensations of tightness, pain, pressure, and heaviness in the precordium, throat, neck, and jaw commonly occur after treatment with IMITREX Injection and are usually non-cardiac in origin. However, perform a cardiac evaluation if these patients are at high cardiac risk. The use of IMITREX Injection is contraindicated in patients shown to have CAD and those with Prinzmetal’s variant angina.
5.4 Cerebrovascular Events Cerebral hemorrhage, subarachnoid hemorrhage, and stroke have occurred in patients treated with 5-HT1 agonists, and some have resulted in fatalities. In a number of cases, it appears possible that the cerebrovascular events were primary, the 5-HT1 agonist having been administered in the incorrect belief that the symptoms experienced were a consequence of migraine when they were not. Also, patients with migraine may be at increased risk of certain cerebrovascular events (e.g., stroke, hemorrhage, TIA). Discontinue IMITREX Injection if a cerebrovascular event occurs.
As with other acute migraine therapies, before treating headaches in patients not previously diagnosed as migraineurs, and in migraineurs who present with atypical symptoms, exclude other potentially serious neurological conditions. IMITREX Injection is contraindicated in patients with a history of stroke or TIA.
5.5 Other Vasospasm Reactions 5-HT1 agonists, including IMITREX Injection, may cause non-coronary vasospastic reactions, such as peripheral vascular ischemia, gastrointestinal vascular ischemia and infarction (presenting with abdominal pain and bloody diarrhea), splenic infarction, and Raynaud’s syndrome. Until further evaluation, IMITREX Injection is contraindicated in patients who experience symptoms or signs suggestive of non-coronary vasospasm reaction following the use of any 5-HT1 agonist.
Reports of transient and permanent blindness and significant partial vision loss have been reported with the use of 5-HT1 agonists. Since visual disorders may be part of a migraine attack, a causal relationship between these events and the use of 5-HT1 agonists have not been clearly established.
5.6 Medication Overuse Headache Overuse of acute migraine drugs (e.g., ergotamine, triptans, opioids, combination of drugs for 10 or more days per month) may lead to exacerbation of headache (medication overuse headache). Medication overuse headache may present as migraine-like daily headaches, or as a marked increase in frequency of migraine attacks. Detoxification of patients, including withdrawal of the overused drugs, and treatment of withdrawal symptoms (which often includes a transient worsening of headache) may be necessary.
5.7 Serotonin Syndrome Serotonin syndrome may occur with triptans, including IMITREX Injection, particularly during coadministration with selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and MAO inhibitors [see Drug Interactions (7.4)]. Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms usually occurs within minutes to hours of receiving a new or a greater dose of a serotonergic medication. Discontinue IMITREX Injection if serotonin syndrome is suspected.
5.8 Increase in Blood Pressure Significant elevation in blood pressure, including hypertensive crisis with acute impairment of organ systems, has been reported on rare occasions in patients treated with 5-HT1 agonists, including patients without a history of hypertension. Monitor blood pressure in patients treated with IMITREX. IMITREX Injection is contraindicated in patients with uncontrolled hypertension.
5.9 Anaphylactic/Anaphylactoid Reactions Anaphylactic/anaphylactoid reactions have occurred in patients receiving sumatriptan. Such reactions can be life threatening or fatal. In general, anaphylactic reactions to drugs are more likely to occur in individuals with a history of sensitivity to multiple allergens. IMITREX Injection is contraindicated in patients with prior serious anaphylactic reaction.
5.10 Seizures Seizures have been reported following administration of sumatriptan. Some have occurred in patients with either a history of seizures or concurrent conditions predisposing to seizures. There are also reports in patients where no such predisposing factors are apparent. IMITREX Injection should be used with caution in patients with a history of epilepsy or conditions associated with a lowered seizure threshold.
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Sumatriptan (injection) Clinical Trials Experience in the drug label.
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of IMITREX Tablets, IMITREX Nasal Spray, and IMITREX Injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to IMITREX or a combination of these factors.
Blood: Hemolytic anemia, pancytopenia, thrombocytopenia.
Ear, Nose, and Throat: Deafness.
Eye: Ischemic optic neuropathy, retinal artery occlusion, retinal vein thrombosis.
Neurological: Central nervous system vasculitis, cerebrovascular accident, serotonin syndrome, subarachnoid hemorrhage.
Non-Site Specific: Angioedema, cyanosis, temporal arteritis.
Skin: Exacerbation of sunburn, hypersensitivity reactions (allergic vasculitis, erythema, pruritus, rash, shortness of breath, urticaria), photosensitivity. Following subcutaneous administration of IMITREX, pain, redness, stinging, induration, swelling, contusion, subcutaneous bleeding, and, on rare occasions, lipoatrophy (depression in the skin) or lipohypertrophy (enlargement or thickening of tissue) have been reported.
Urogenital: Acute renal failure.
Drug Interactions
7.1 Ergot-Containing Drugs Ergot-containing drugs have been reported to cause prolonged vasospastic reactions. Because these effects may be additive, use of ergotamine-containing or ergot-type medications (like dihydroergotamine or methysergide) and IMITREX Injection within 24 hours of each other is contraindicated.
7.2 Monoamine Oxidase-A Inhibitors MAO-A inhibitors increase systemic exposure by 2-fold. Therefore, the use of IMITREX Injection in patients receiving MAO-A inhibitors is contraindicated [see Clinical Pharmacology (12.3)].
7.3 Other 5-HT 1 Agonists Because their vasospastic effects may be additive, coadministration of IMITREX Injection and other 5-HT1 agonists (e.g., triptans) within 24 hours of each other is contraindicated.
7.4 Selective Serotonin Reuptake Inhibitors/Serotonin Norepinephrine Reuptake Inhibitors and Serotonin Syndrome Cases of serotonin syndrome have been reported during coadministration of triptans and SSRIs, or SNRIs, TCAs, and MAO inhibitors [see Warnings and Precautions (5.7)].
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C There are no adequate and well-controlled trials of IMITREX Injection in pregnant women. IMITREX Injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
When sumatriptan was administered intravenously to pregnant rabbits daily throughout the period of organogenesis, embryolethality was observed at doses at or close to those producing maternal toxicity. These doses were less than the maximum recommended human dose (MRHD) of 12 mg/day on a mg/m2 basis. Oral administration of sumatriptan to rabbits during organogenesis was associated with increased incidences of fetal vascular and skeletal abnormalities. The highest no-effect dose for these effects was 15 mg/kg/day. The intravenous administration of sumatriptan to pregnant rats throughout organogenesis at doses that are approximately 10 times the MRHD on a mg/m2 basis, did not produce evidence of embryolethality. The subcutaneous administration of sumatriptan to pregnant rats prior to and throughout pregnancy did not produce evidence of embryolethality or teratogenicity.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sumatriptan (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Sumatriptan (injection) during labor and delivery.
Nursing Mothers
It is not known whether sumatriptan is excreted in human breast milk following subcutaneous administration. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from IMITREX, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness of IMITREX Injection in pediatric patients under 18 years of age have not been established; therefore, IMITREX Injection is not recommended for use in patients under 18 years of age.
Two controlled clinical trials evaluated IMITREX Nasal Spray (5 to 20 mg) in 1,248 adolescent migraineurs aged 12 to 17 years who treated a single attack. The trials did not establish the efficacy of IMITREX Nasal Spray compared with placebo in the treatment of migraine in adolescents. Adverse reactions observed in these clinical trials were similar in nature to those reported in clinical trials in adults.
Five controlled clinical trials (2 single-attack trials, 3 multiple-attack trials) evaluating oral IMITREX (25 to 100 mg) in pediatric subjects aged 12 to 17 years enrolled a total of 701 adolescent migraineurs. These trials did not establish the efficacy of oral IMITREX compared with placebo in the treatment of migraine in adolescents. Adverse reactions observed in these clinical trials were similar in nature to those reported in clinical trials in adults. The frequency of all adverse reactions in these subjects appeared to be both dose- and age-dependent, with younger subjects reporting reactions more commonly than older adolescents.
Postmarketing experience documents that serious adverse reactions have occurred in the pediatric population after use of subcutaneous, oral, and/or intranasal IMITREX. These reports include reactions similar in nature to those reported rarely in adults, including stroke, visual loss, and death. A myocardial infarction has been reported in a 14-year-old male following the use of oral IMITREX; clinical signs occurred within 1 day of drug administration. Since clinical data to determine the frequency of serious adverse reactions in pediatric patients who might receive subcutaneous, oral, or intranasal IMITREX are not presently available, the use of IMITREX in patients under 18 years of age is not recommended.
Geriatic Use
Clinical trials of IMITREX Injection did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
A cardiovascular evaluation is recommended for geriatric patients who have other cardiovascular risk factors (e.g., diabetes, hypertension, smoking, obesity, strong family history of CAD) prior to receiving IMITREX Injection [see Warnings and Precautions (5.1)].
Gender
There is no FDA guidance on the use of Sumatriptan (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Sumatriptan (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Sumatriptan (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Sumatriptan (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Sumatriptan (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Sumatriptan (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Sumatriptan (injection) Administration in the drug label.
Monitoring
There is limited information regarding Sumatriptan (injection) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Sumatriptan (injection) and IV administrations.
Overdosage
No gross overdoses in clinical practice have been reported. Coronary vasospasm was observed after intravenous administration of IMITREX Injection [see Contraindications (4)]. Overdoses would be expected from animal data (dogs at 0.1 g/kg, rats at 2 g/kg) to possibly cause convulsions, tremor, inactivity, erythema of the extremities, reduced respiratory rate, cyanosis, ataxia, mydriasis, injection site reactions (desquamation, hair loss, and scab formation), and paralysis.
The elimination half-life of sumatriptan is about 2 hours [see Clinical Pharmacology (12.3)], and therefore monitoring of patients after overdose with IMITREX Injection should continue for at least 10 hours or while symptoms or signs persist.
It is unknown what effect hemodialysis or peritoneal dialysis has on the serum concentrations of sumatriptan.
Pharmacology
Mechanism of Action
Sumatriptan binds with high affinity to human cloned 5-HT1B/1D receptors. IMITREX presumably exerts its therapeutic effects in the treatment of migraine headache by binding to 5-HT1B/1D receptors located on intracranial blood vessels and sensory nerves of the trigeminal system.
Current theories proposed to explain the etiology of migraine headache suggest that symptoms are due to local cranial vasodilatation and/or to the release of sensory neuropeptides (including substance P and calcitonin gene-related peptide) through nerve endings in the trigeminal system. The therapeutic activity of IMITREX for the treatment of migraine and cluster headaches is thought to be due to the agonist effects at the 5-HT1B/1D receptors on intracranial blood vessels (including the arterio-venous anastomoses) and sensory nerves of the trigeminal system, which result in cranial vessel constriction and inhibition of pro-inflammatory neuropeptide release.
Structure
IMITREX Injection contains sumatriptan succinate, a selective 5-HT1B/1D receptor agonist. Sumatriptan succinate is chemically designated as 3-[2-(dimethylamino)ethyl]-N-methyl-indole-5-methanesulfonamide succinate (1:1), and it has the following structure:
The empirical formula is C14H21N3O2S•C4H6O4, representing a molecular weight of 413.5. Sumatriptan succinate is a white to off-white powder that is readily soluble in water and in saline.
IMITREX Injection is a clear, colorless to pale yellow, sterile, nonpyrogenic solution for subcutaneous injection. Each 0.5 mL of IMITREX Injection 8 mg/mL solution contains 4 mg of sumatriptan (base) as the succinate salt and 3.8 mg of sodium chloride, USP in Water for Injection, USP. Each 0.5 mL of IMITREX Injection 12 mg/mL solution contains 6 mg of sumatriptan (base) as the succinate salt and 3.5 mg of sodium chloride, USP in Water for Injection, USP. The pH range of both solutions is approximately 4.2 to 5.3. The osmolality of both injections is 291 mOsmol.
Pharmacodynamics
Blood Pressure: Significant elevation in blood pressure, including hypertensive crisis, has been reported in patients with and without a history of hypertension [see Warnings and Precautions (5.8)].
Peripheral (Small) Arteries: In healthy volunteers (N = 18), a trial evaluating the effects of sumatriptan on peripheral (small vessel) arterial reactivity failed to detect a clinically significant increase in peripheral resistance.
Heart Rate: Transient increases in blood pressure observed in some subjects in clinical trials carried out during sumatriptan’s development as a treatment for migraine were not accompanied by any clinically significant changes in heart rate.
Pharmacokinetics
Absorption and Bioavailability: The bioavailability of sumatriptan via subcutaneous site injection to 18 healthy male subjects was 97% ± 16% of that obtained following intravenous injection.
After a single 6-mg subcutaneous manual injection into the deltoid area of the arm in 18 healthy males (age: 24 ± 6 years, weight: 70 kg), the maximum serum concentration (Cmax) of sumatriptan was (mean ± standard deviation) 74 ± 15 ng/mL and the time to peak concentration (Tmax) was 12 minutes after injection (range: 5 to 20 minutes). In this trial, the same dose injected subcutaneously in the thigh gave a Cmax of 61 ± 15 ng/mL by manual injection versus 52 ± 15 ng/mL by autoinjector techniques. The Tmax or amount absorbed was not significantly altered by either the site or technique of injection.
Distribution: Protein binding, determined by equilibrium dialysis over the concentration range of 10 to 1,000 ng/mL, is low, approximately 14% to 21%. The effect of sumatriptan on the protein binding of other drugs has not been evaluated.
Following a 6-mg subcutaneous injection into the deltoid area of the arm in 9 males (mean age: 33 years, mean weight: 77 kg) the volume of distribution central compartment of sumatriptan was 50 ± 8 liters and the distribution half‑life was 15 ± 2 minutes.
Metabolism: In vitro studies with human microsomes suggest that sumatriptan is metabolized by MAO, predominantly the A isoenzyme. Most of a radiolabeled dose of sumatriptan excreted in the urine is the major metabolite indole acetic acid (IAA) or the IAA glucuronide, both of which are inactive.
Elimination: After a single 6-mg subcutaneous dose, 22% ± 4% was excreted in the urine as unchanged sumatriptan and 38% ± 7% as the IAA metabolite.
Following a 6-mg subcutaneous injection into the deltoid area of the arm, the systemic clearance of sumatriptan was 1,194 ± 149 mL/min and the terminal half-life was 115 ± 19 minutes.
Special Populations:Age: The pharmacokinetics of sumatriptan in the elderly (mean age: 72 years, 2 males and 4 females) and in subjects with migraine (mean age: 38 years, 25 males and 155 females) were similar to that in healthy male subjects (mean age: 30 years).
Renal Impairment: The effect of renal impairment on the pharmacokinetics of sumatriptan has not been examined.
Hepatic Impairment: The effect of mild to moderate hepatic disease on the pharmacokinetics of subcutaneously administered sumatriptan has been evaluated. There were no significant differences in the pharmacokinetics of subcutaneously administered sumatriptan in moderately hepatically impaired subjects compared with healthy controls. The pharmacokinetics of subcutaneously administered sumatriptan in patients with severe hepatic impairment has not been studied. The use of IMITREX Injection in this population is contraindicated [see Contraindications (4)].
Race: The systemic clearance and Cmax of sumatriptan were similar in black (n = 34) and Caucasian (n = 38) healthy male subjects.
Drug Interaction Studies: Monoamine Oxidase-A Inhibitors:In a trial of 14 healthy females, pretreatment with an MAO-A inhibitor decreased the clearance of sumatriptan, resulting in a 2-fold increase in the area under the sumatriptan plasma concentration-time curve (AUC), corresponding to a 40% increase in elimination half-life.
Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis: In carcinogenicity studies, rats and mice were given sumatriptan by oral gavage. Mice were dosed for 78 weeks and rats were dosed for 104 weeks. Average exposures achieved in mice receiving the highest dose were approximately 110 times the exposure attained in humans after the maximum recommended single dose of 6 mg. The highest dose to rats was approximately 260 times the maximum single dose of 6 mg on a mg/m2 basis. There was no evidence of an increase in tumors in either species related to sumatriptan administration.
Mutagenesis: Sumatriptan was not mutagenic in the presence or absence of metabolic activation when tested in 2 gene mutation assays (the Ames test and the in vitro mammalian Chinese hamster V79/HGPRT assay). It was not clastogenic in 2 cytogenetics assays (the in vitro human lymphocyte assay and the in vivo rat micronucleus assay).
Impairment of Fertility: A fertility study (Segment I) by the subcutaneous route, during which male and female rats were dosed daily with sumatriptan prior to and throughout the mating period, has shown no evidence of impaired fertility at doses equivalent to approximately 100 times the maximum recommended single human dose of 6 mg on a mg/m2 basis. However, following oral administration, a treatment-related decrease in fertility, secondary to a decrease in mating, was seen for rats treated with 50 and 500 mg/kg/day. The no-effect dose for this finding was approximately 8 times the maximum recommended single human dose of 6 mg on a mg/m2 basis. It is not clear whether the problem is associated with the treatment of males or females or both.
13.2 Animal Toxicology and/or Pharmacology Corneal Opacities: Dogs receiving oral sumatriptan developed corneal opacities and defects in the corneal epithelium. Corneal opacities were seen at the lowest dosage tested, 2 mg/kg/day, and were present after 1 month of treatment. Defects in the corneal epithelium were noted in a 60-week study. Earlier examinations for these toxicities were not conducted and no-effect doses were not established; however, the relative exposure at the lowest dose tested was approximately 5 times the human exposure after a 100-mg oral dose or 3 times the human exposure after a 6-mg subcutaneous dose.
Melanin Binding: In rats with a single subcutaneous dose (0.5 mg/kg) of radiolabeled sumatriptan, the elimination half-life of radioactivity from the eye was 15 days, suggesting that sumatriptan and its metabolites bind to the melanin of the eye. The clinical significance of this binding is unknown.
Clinical Studies
There is limited information regarding Sumatriptan (injection) Clinical Studies in the drug label.
How Supplied
There is limited information regarding Sumatriptan (injection) How Supplied in the drug label.
Storage
There is limited information regarding Sumatriptan (injection) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Sumatriptan (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Sumatriptan (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Sumatriptan (injection) Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Sumatriptan (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Sumatriptan (injection) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Sumatriptan (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.