Stress cardiomyopathy
| Stress cardiomyopathy | |
 | |
|---|---|
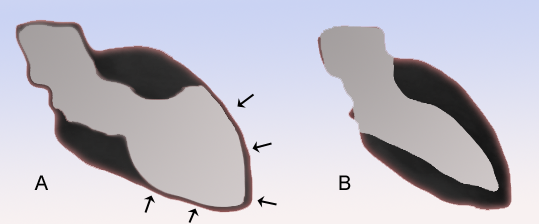
| Schematic representation of Takotsubo cardiomyopathy (A) compared to the situation in a normal person (B). | |
| ICD-9 | 429.83 |
| DiseasesDB | 33976 |
| MeSH | 054549 |
|
Stress cardiomyopathy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Unstable angina/non ST elevation myocardial infarction in Stress (Takotsubo) Cardiomyopathy |
|
Case Studies |
|
Stress cardiomyopathy On the Web |
|
American Roentgen Ray Society Images of Stress cardiomyopathy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Takotsubo cardiomyopathy; Tako-tsubo syndrome; Left Ventricular Apical Ballooning Syndrome; Ampulla-Shaped Cardiomyopathy; Broken Heart Syndrome; transient apical dysfunction
Overview
Stress cardiomyopathy is a cardiac syndrome characterized by a reversible transient apical ventricular dysfunction.
Diagnosis
History
A directed history should be obtained to evaluate if the patient has a history of emotional stress such as the death of a loved one or loss of job.
Symptoms
- The typical presentation of patients with stress cardiomyopathy includes acute onset of chest pain or shortness of breath, and is similar to an acute coronary syndrome
Physical examination
- Bulging out of the left ventricular apex with a hypercontractile base of the left ventricle is often noted.
Electrocardiogram
The EKG findings are often confused with those of an acute anterior wall myocardial infarction.[1][2] While the ECG may reveal ST-segment elevation, it may also reveal non-specific ST/T wave abnormality, usually in the precordial leads. The 12-lead ECG alone is not helpful in differentiating apical ballooning syndrome from a traditional thrombotic ST-elevation myocardial infarction. Evolutionary changes occur over 2 to 3 days that are characteristic and include resolution of the ST-segment elevation and development of diffuse and frequently deep T-wave inversion.
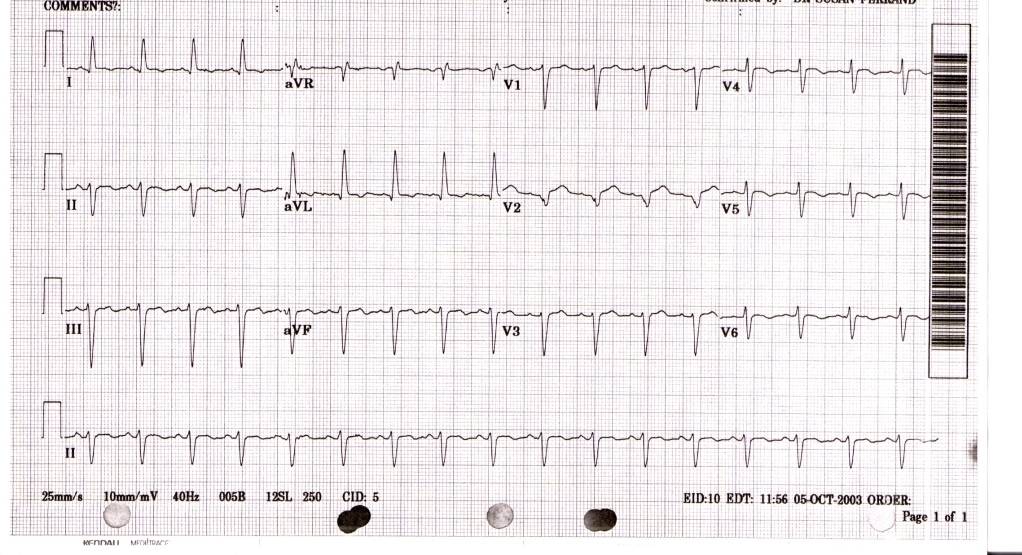
The diagnosis of takotsubo cardiomyopathy may be difficult upon presentation. The EKG findings are often confused with those found during an acute anterior wall myocardial infarction.[1][2]
Biomarker Studies
Cardiac biomarkers of myonecrosis, especially troponin, are invariably elevated.
Echocardiography
Cardiac Catheterization
Coronary angiography usually demonstrates normal coronary arteries or mild coronary atherosclerosis. The left ventriculogram usually reveals characteristic regional wall motion abnormalities which involve the mid and usually the apical segments. There is sparing of the basal systolic function, and the wall motion abnormality extends beyond the distribution of any one single coronary artery.

The diagnosis is made by the pathognomic wall motion abnormalities, in which the base of the left ventricle is contracting normally or are hyperkinetic while the remainder of the left ventricle is akinetic or dyskinetic. This is accompanied by the lack of significant coronary artery disease that would explain the wall motion abnormalities.
Magnetic Resonance Imaging
The use of MRIs as a valuable diagnostic tool in differentiating cardiomyopathy from acute myocardial infarction and myocarditis cases. Cardiac magnetic resonance imaging is helpful in excluding a myocardial infarction due to the absence of delayed gadolinium hyperenhancement.
The Eitel study is the largest (n=256), (multi-center) cardiovascular MRI imaging series of stress cardiomyopathy [3]. Stress cardiomyopathy can be accurately diagnosed by identifying a typical pattern of LV dysfunction, myocardial edema, absence of significant necrosis/fibrosis, and markers of myocardial inflammation. There are four distinct patterns of regional ventricular ballooning: apical (82%), biventricular (34%), midventricular (17%), and basal (1%). Because patients with RV involvement tended to be older, hospitalized for longer, and have markers of heart failure, biventricular ballooning on MRI “may portend a longer and more severe course of disease compared with patients with isolated (LV) involvement.” Dysfunctions in the right ventricle are important to identify due to its effects on morbidity, treatment, and outcome. During follow up MRIs, patients exhibited normalization of LVEF (66%) and inflammatory markers in the absence of significant fibrosis in all patients.
MRI Examples
The MRIs below show a patients heart with apical ballooning and then later after resolution of the apical ballooning.
MRI during apical balllooning: <youtube v=23w6f71zTXI/> ____
MRI following resolution of apical ballooning: <youtube v=qE0YrlQ5d1o/>
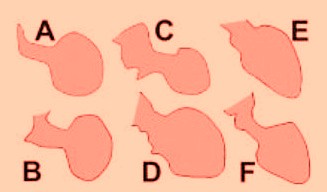
The Various Patterns of Wall Motion Abnormalities
It should be that the wall motion abnormalities are not always anteroapical.
A, [4]; B, [5]; C, [6]; D, [7]; E, [8]; and F, [9]. There is wide heterogeneity among the different patterns, varying from a relatively small akinetic apical area in C to a wide global akinesia in D and E. [10]
Mayo Criteria
Mayo Clinic Criteria for Apical Ballooning Syndrome. All 4 must be present [11]:
- Transient hypokinesis, akinesis or dyskinesis of the left ventricular mid-segments with or without apical involvement. The regional wall motion abnormalities extend beyond a single epicardial vascular distribution. A stressful trigger is often, but not always present
- Absence of obstructive coronary disease or angiographic evidence of acute plaque rupture.
- New electrocardiographic abnormalities (either ST-segment elevation and/or T- wave inversion) or modest elevation in cardiac troponin.
- Absence of pheochromocytoma and myocarditis
Treatment
The treatment of stress cardiomyopathy is supportive as the condition is reversible. Initial treatment should be similar to that of an acute coronary syndrome with therapy directed at relieving myocardial ischemia with administration of aspirin, intravenous heparin and beta blockers. Once a diagnosis of stress cardiomyopathy has been confirmed and an acute coronary syndrome excluded, consideration should be given to continuing beta-blocker therapy empirically since catecholamines are suspected of contributing to the syndrome. Diuretics are effective for the treatment of congestive heart failure. Angiotensin converting enzyme inhibitors may be used if the diagnosis is uncertain, until there is complete recovery of systolic function. Insofar as the left ventricular function and apical wall motion return to normal within days or weeks, long-term anti-coagulation does not appear to be necessary.
References
- ↑ 1.0 1.1
- ↑ 2.0 2.1 Bybee KA, Motiei A, Syed IS, Kara T, Prasad A, Lennon RJ, Murphy JG, Hammill SC, Rihal CS, Wright RS (2006). "Electrocardiography cannot reliably differentiate transient left ventricular apical ballooning syndrome from anterior ST-segment elevation myocardial infarction". J Electrocardiol. PMID 17067626.
- ↑ Eitel I, von Knobelsdorff-Brekenhoff F, Bernhardt P, et al. Clinical characteristics and CV magnetic resonance findings in stress (Takotsubo) cardiomyopathy. JAMA 2011; 306:277-286.
- ↑ Abe Y, Kondo M, Matsuoka R, Araki M, Dohyama K, Tanio H. Assessment of clinical features in transient left ventricular apical ballooning. J Am Coll Cardiol. 2003;41:737-742.
- ↑ San Roman Sanchez D, Medina O, Jimenez F, Rodriguez JC, Nieto V. Dynamic intraventricular obstruction in acute myocardial infarction. Echocardiography. 2001;18:515-518.
- ↑ Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539-548.
- ↑ Rivera JM, Locketz AJ, Fritz KD, et al. “Broken heart syndrome” after separation (from OxyContin). Mayo Clin Proc. 2006;81:825-828.
- ↑ Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart. 2003;89:1027-1031.
- ↑ Reyburn AM, Vaglio JC Jr. Transient left ventricular apical ballooning syndrome. Mayo Clin Proc. 2006;81:824.
- ↑ Ibanez B. Takotsubo Syndrome: A Bayesian Approach to Interpreting Its Pathogenesis Mayo Clin Proc. 2006; 81: 732-735
- ↑ Prasad A (2007). "Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction". Circulation. 115 (5): e56–9. doi:10.1161/CIRCULATIONAHA.106.669341. PMID 17283269.