Streptococcus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 64: | Line 64: | ||
''[[Streptococcus agalactiae|S. agalactiae]]'', or ''GBS'', causes [[pneumonia]] and [[meningitis]] in [[neonate]]s and the [[elderly]], with occasional systemic [[bacteremia]]. They can also colonize the intestines and the female reproductive tract, increasing the risk for premature rupture of membranes and transmission to the infant. | ''[[Streptococcus agalactiae|S. agalactiae]]'', or ''GBS'', causes [[pneumonia]] and [[meningitis]] in [[neonate]]s and the [[elderly]], with occasional systemic [[bacteremia]]. They can also colonize the intestines and the female reproductive tract, increasing the risk for premature rupture of membranes and transmission to the infant. | ||
The American College of Obstetricians and Gynecologists, American Academy of Pediatrics and the [[Centers for Disease Control]] recommend all pregnant women between 35 and 37 weeks gestation should be tested for GBS. Women who test positive should be given prophylactic antibiotics during labor, which will usually prevent transmission to the infant.<ref name=Schrag_2002>{{cite journal |author=Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A |title=Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC |journal=MMWR Recomm Rep |volume=51 |issue=RR-11 |pages=1-22 |year=2002 |pmid=12211284}}</ref> In the UK, clinicians have been slow to implement the same standards as the US, Australia and Canada. In the UK, only 1% of maternity units test for the presence of Group B Strep.<ref name=RCOG_2003>{{cite paper | author = Hughes, RG, et al. | title = Prevention of Early Onset Neonatal Group B Streptococcal Disease | publisher = Royal College of Obstetricians and Gynaecologists | url = http://www.rcog.org.uk/index.asp?PageID=520 | format = | The American College of Obstetricians and Gynecologists, American Academy of Pediatrics and the [[Centers for Disease Control]] recommend all pregnant women between 35 and 37 weeks gestation should be tested for GBS. Women who test positive should be given prophylactic antibiotics during labor, which will usually prevent transmission to the infant.<ref name=Schrag_2002>{{cite journal |author=Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A |title=Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC |journal=MMWR Recomm Rep |volume=51 |issue=RR-11 |pages=1-22 |year=2002 |pmid=12211284}}</ref> In the UK, clinicians have been slow to implement the same standards as the US, Australia and Canada. In the UK, only 1% of maternity units test for the presence of Group B Strep.<ref name=RCOG_2003>{{cite paper | author = Hughes, RG, et al. | title = Prevention of Early Onset Neonatal Group B Streptococcal Disease | publisher = Royal College of Obstetricians and Gynaecologists | url = http://www.rcog.org.uk/index.asp?PageID=520 | format = HTML}}</ref> | ||
Although The Royal College of Obstetricians and Gynaecologists issued risk-based guidelines in 2003 (due for review 2006), the implentation of these guidelines has been patchy. Some groups feel that as a result over 75 infants in the UK die each year of GBS related disease and another 600 or so suffer serious infection, most of which could be prevented <ref name=GBSS_2007>{{cite web | title = Group B Strep Support Home Page | publisher = Group B Strep Support | date = 2007-01-09 | url = http://www.gbss.org.uk/ | format = | Although The Royal College of Obstetricians and Gynaecologists issued risk-based guidelines in 2003 (due for review 2006), the implentation of these guidelines has been patchy. Some groups feel that as a result over 75 infants in the UK die each year of GBS related disease and another 600 or so suffer serious infection, most of which could be prevented <ref name=GBSS_2007>{{cite web | title = Group B Strep Support Home Page | publisher = Group B Strep Support | date = 2007-01-09 | url = http://www.gbss.org.uk/ | format = HTML}}</ref> however this is yet to be substantiated by RCT in the UK setting and, given the evidence for the efficacy of testing and treating from other countries, it may be that the large-scale trial necessary would receive neither funding nor ethics approval.<ref name=Arjb1_2007>{{cite web | title = RCOG: Preventing group B streptococcus infection in new born babies | publisher = RCOG | date = 2006-02 | url = http://www.rcog.org.uk/index.asp?PageID=1400#national | format = HTML}}</ref> | ||
====Group C ==== | ====Group C ==== | ||
Revision as of 22:08, 20 January 2009
| Streptococcus | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | ||||||||||||
| Scientific classification | ||||||||||||
| ||||||||||||
| Species | ||||||||||||
|
S. agalactiae |
|
WikiDoc Resources for Streptococcus |
|
Articles |
|---|
|
Most recent articles on Streptococcus Most cited articles on Streptococcus |
|
Media |
|
Powerpoint slides on Streptococcus |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Streptococcus at Clinical Trials.gov Trial results on Streptococcus Clinical Trials on Streptococcus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Streptococcus NICE Guidance on Streptococcus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Streptococcus Discussion groups on Streptococcus Patient Handouts on Streptococcus Directions to Hospitals Treating Streptococcus Risk calculators and risk factors for Streptococcus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Streptococcus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
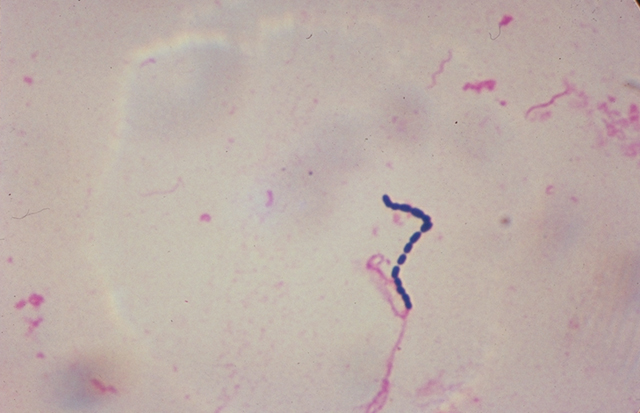
Streptococcus is a genus of spherical Gram-positive bacteria, belonging to the phylum Firmicutes[1] and the lactic acid bacteria group. Cellular division occurs along a single axis in these bacteria, and thus they grow in chains or pairs, hence the name — from Greek streptos, meaning easily bent or twisted, like a chain. Contrast this with staphylococci, which divide along multiple axes and generate grape-like clusters of cells.
Streptococci are oxidase– and catalase–negative.
Pathogenesis
In addition to strep throat, certain Streptococcus species are responsible for many cases of meningitis, bacterial pneumonia, endocarditis, erysipelas and necrotizing fasciitis (the 'flesh-eating' bacterial infections). However, many streptococcal species are non-pathogenic. Streptococci are also part of the normal commensal flora of the mouth, skin, intestine, and upper respiratory tract of humans.
As a rule, individual species of Streptococcus are classified based on their hemolytic properties (breakdown of red blood cells in a laboratory).[2] Alpha hemolysis is caused by a reduction of iron in hemoglobin, giving it a greenish color on blood agar. Beta-only hemolysis is complete rupture of red blood cells, giving distinct, wide, clear areas around bacterial colonies on blood agar. Other streptococci are labeled as gamma hemolytic, actually a misnomer, as no hemolysis takes place.
Beta-hemolytic streptococci are further characterised via the Lancefield serotyping - based on specific carbohydrates in the bacterial cell wall.[3] These are named Lancefield groups A to T, although some species, such as S. pneumoniae, do not express Lancefield antigens. See the related article on Rebecca Lancefield. In the medical setting, the most important groups are the alpha-hemolytic streptococci, S. pneumoniae and Streptococcus Viridans-group, and the beta-hemolytic streptococci of Lancefield groups A and B (also known as “Group A Strep” and “Group B Strep”).
Alpha-Hemolytic Streptococcus
Pneumococci
- S. pneumoniae, a leading cause of bacterial pneumonia, otitis media and meningitis.
Viridans and Others
- S. mutans, a contributor to dental caries
- S. viridans, a cause of endocarditis and dental abscesses
- S. thermophilus, used in the manufacture of some cheeses and yogurts
- S. constellatus, occasional human pathogen, notable as colonies grown on blood agar smell strongly of caramel
Beta-Hemolytic Streptococci
Group A
S. pyogenes (also known as GAS) is the causative agent in Group A streptococcal infections, (GAS) including strep throat, acute rheumatic fever, scarlet fever, acute glomerulonephritis and necrotizing fasciitis. If strep throat is not treated, it can develop into rheumatic fever, a disease that affects the joints and heart valves. Other Streptococcus species may also possess the Group A antigen, but human infections by non-S. pyogenes GAS strains (some S. dysgalactiae subsp. equisimilis and S. anginosus Group strains) appear to be uncommon.
Group A Strep infection is generally diagnosed with a Rapid Strep Test or by culture.
Group B
S. agalactiae, or GBS, causes pneumonia and meningitis in neonates and the elderly, with occasional systemic bacteremia. They can also colonize the intestines and the female reproductive tract, increasing the risk for premature rupture of membranes and transmission to the infant.
The American College of Obstetricians and Gynecologists, American Academy of Pediatrics and the Centers for Disease Control recommend all pregnant women between 35 and 37 weeks gestation should be tested for GBS. Women who test positive should be given prophylactic antibiotics during labor, which will usually prevent transmission to the infant.[4] In the UK, clinicians have been slow to implement the same standards as the US, Australia and Canada. In the UK, only 1% of maternity units test for the presence of Group B Strep.[5]
Although The Royal College of Obstetricians and Gynaecologists issued risk-based guidelines in 2003 (due for review 2006), the implentation of these guidelines has been patchy. Some groups feel that as a result over 75 infants in the UK die each year of GBS related disease and another 600 or so suffer serious infection, most of which could be prevented [6] however this is yet to be substantiated by RCT in the UK setting and, given the evidence for the efficacy of testing and treating from other countries, it may be that the large-scale trial necessary would receive neither funding nor ethics approval.[7]
Group C
Includes S. equi, which causes strangles in horses,[8] and S. zooepidemicus, which causes infections in several species of mammals including cattle and horses. This can also cause death in chickens and moose. Many mountaineers from Canada have found corpses of moose lying in the middle of the road; post-mortem tests have found group c streptococcus in their blood.
Group D (Enterococci) *variable in hemolysis
Many former Group D streptococci have been reclassified and placed in the genus Enterococcus (includes S. faecalis, S. faciem, S. durans, and S. avium).[9] For example, Streptococcus faecalis is now Enterococcus faecalis.
The remaining non-enterococcal Group D strains include Streptococcus bovis and Streptococcus equinus.
Non-Hemolytic Streptococci
Non-hemolytic streptococci rarely cause disease. However, weakly hemolytic group D beta-hemolytic streptococci and Listeria monocytogenes should not be confused with non-hemolytic streptococci.
References
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ↑ Patterson MJ (1996). Streptococcus. In: Baron's Medical Microbiology (Baron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. (via NCBI Bookshelf) ISBN 0-9631172-1-1.
- ↑ Facklam R (2002). "What happened to the streptococci: overview of taxonomic and nomenclature changes". Clin Microbiol Rev. 15 (4): 613–30. PMID 12364372.
- ↑ Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A (2002). "Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC". MMWR Recomm Rep. 51 (RR-11): 1–22. PMID 12211284.
- ↑ Template:Cite paper
- ↑ "Group B Strep Support Home Page" (HTML). Group B Strep Support. 2007-01-09.
- ↑ "RCOG: Preventing group B streptococcus infection in new born babies" (HTML). RCOG. 2006-02. Check date values in:
|date=(help) - ↑ Harrington D, Sutcliffe I, Chanter N (2002). "The molecular basis of Streptococcus equi infection and disease". Microbes Infect. 4 (4): 501–10. PMID 11932201.
- ↑ Ruoff KL (1990). "Recent taxonomic changes in the genus Enterococcus". Eur J Clin Microbiol Infect Dis. 9 (2): 75–9. PMID 2108030.
External links
- Prevention of Perinatal Group B Streptococcal Disease August 16, 2002 MMWR 2000;49:228-232.
- The Canadian Strep B Foundation
- The UK Group B Strep Support charity
ca:Estreptococ da:Streptokok de:Streptokokken is:Streptókokkar it:Streptococco he:Streptococcus lt:Streptokokai nl:Streptokokken no:Streptokokker sr:Стрептококе fi:Streptococcus sv:Streptokocker uk:Стрептокок