Spironolactone: Difference between revisions
No edit summary |
m (Protected "Spironolactone": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (19 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | {{DrugProjectFormSinglePage | ||
|authorTag={{SS}} | |authorTag={{SS}}, {{RB}} | ||
|genericName=Spironolactone | |genericName=Spironolactone | ||
|aOrAn=an | |aOrAn=an | ||
|drugClass= | |drugClass=[[aldosterone antagonist]] | ||
|indication=Primary hyperaldosteronism,edematous conditions of [[congestive heart failure]], [[ | |indicationType=treatment | ||
|indication=[[Primary hyperaldosteronism]],[[Edema|edematous]] conditions of [[congestive heart failure]], [[Cirrhosis|Cirrhosis of the liver]] accompanied by [[edema]] and/or [[ascites]], [[nephrotic syndrome]], [[essential hypertension]] | |||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions=[[gynecomastia]], [[diarrhea]], [[nausea]] and [[vomiting]],[[somnolence]],disorder of menstruation, [[impotence]] | |adverseReactions=[[gynecomastia]], [[diarrhea]], [[nausea]] and [[vomiting]], [[somnolence]], [[Menstrual disorder|disorder of menstruation]], [[impotence]] | ||
|blackBoxWarningTitle=WARNING | |blackBoxWarningTitle=<span style="color:#FF0000;">WARNING</span> | ||
|blackBoxWarningBody=Spironolactone has been shown to be a tumorigen in chronic toxicity studies in rats | |blackBoxWarningBody=Spironolactone has been shown to be a tumorigen in chronic toxicity studies in rats. Spironolactone tablets should be used only in those conditions described under Indications and Usage. Unnecessary use of this drug should be avoided. | ||
|fdaLIADAdult======Primary hyperaldosteronism===== | |fdaLIADAdult======Primary hyperaldosteronism===== | ||
* Dosing Information | * Dosing Information | ||
:* Long test: 400 mg/day PO for 3-4 weeks | :* Long test: '''400 mg/day PO for 3-4 weeks ''' | ||
:* Short test: 400 mg/day PO for 4 days | ::* Correction of [[hypokalemia]] and of [[hypertension]] provides presumptive evidence for the diagnosis of [[primary hyperaldosteronism]]. | ||
:* Short test: '''400 mg/day PO for 4 days''' | |||
::* If serum [[potassium]] increases during spironolactone administration but drops when spironolactone tablets are discontinued, a presumptive diagnosis of [[primary hyperaldosteronism]] should be considered. | |||
:* After the diagnosis: '''100-400 mg/day'''in preparation for surgery. | |||
::*: For the patient unsuitable for surgery: spironolactone tablets may be employed for long-term maintenance therapy at the lowest effective dosage determined for the individual patient. | |||
=====Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)===== | =====Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)===== | ||
* Dosing information | * Dosing information (given as the sole agent for diuresis) | ||
:* Initial dosage: '''100 mg/day PO for at least 5 days''' either single or divided dose. | |||
:* Dosage range: '''25-200 mg/day''' | |||
* Dosing information (combination with other diuretic) | |||
:* | :* If, after five days, an adequate diuretic response to spironolactone tablets has not occurred, a second diuretic that acts more proximally in the renal tubule may be added to the regimen. | ||
:* dosage | ::* Because of the additive effect of spironolactone tablets when administered concurrently with such [[diuretics]], an enhanced [[diuresis]] usually begins on the first day of combined treatment. | ||
::* Combined therapy is indicated when more rapid [[diuresis]] is desired. The dosage of spironolactone tablets should remain unchanged when other diuretic therapy is added. | |||
=====Essential hypertension===== | =====Essential hypertension===== | ||
| Line 27: | Line 40: | ||
* Dosing information | * Dosing information | ||
:* | :* Initial dosage: '''50-100 mg/days PO''', in either single or divided doses. | ||
::* Duration: '''at least 2 weeks''' (since the maximum response may not occur before this time. Subsequently, dosage should be adjusted according to the response of the patient.) | |||
=====Hypokalemia===== | =====Hypokalemia===== | ||
| Line 33: | Line 47: | ||
* Dosing information | * Dosing information | ||
:* initial dosage: 50-100 mg/days PO | :* initial dosage: '''50-100 mg/days PO''' (when oral [[potassium]] supplements or other potassium-sparing regimens are considered inappropriate.) | ||
=====Severe heart failure in conjunction with standard therapy (NYHA class III – IV)===== | =====Severe heart failure in conjunction with standard therapy (NYHA class III – IV)===== | ||
| Line 39: | Line 53: | ||
* Dosing information | * Dosing information | ||
:* | :* Initial dosage: '''25 mg PO qd''' (serum [[potassium]] is ≤5.0 mEq/L and the patient's serum [[creatinine]] is ≤ 2.5 mg/dL) | ||
:* | :* Patient who can tolerate 25 mg once daily: '''50 mg PO qd ''' | ||
:* | :* Patient who can't tolerate 25 mg once daily: '''25 mg PO q.o.d''' | ||
|offLabelAdultGuideSupport=There is limited information about <i>Off-Label Guideline-Supported Use</i> of Spironolactone in adult patients. | |||
|offLabelAdultNoGuideSupport======Acne vulgaris===== | |offLabelAdultNoGuideSupport======Acne vulgaris===== | ||
* Dosing information | * Dosing information | ||
:* 50-200 mg PO | :* '''50-200 mg PO ''' | ||
:* | :* Optimal dosage: '''150-200 mg PO''' <ref name="pmid8112074">Vincenzi C, Trevisi P, Farina P, Stinchi C, Tosti A (1993) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=8112074 Facial contact dermatitis due to spironolactone in an anti-acne cream.] ''Contact Dermatitis'' 29 (5):277-8. PMID: [http://pubmed.gov/8112074 8112074]</ref><ref name="pmid2449021">Hatwal A, Bhatt RP, Agrawal JK, Singh G, Bajpai HS (1988) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=2449021 Spironolactone and cimetidine in treatment of acne.] ''Acta Derm Venereol'' 68 (1):84-7. PMID: [http://pubmed.gov/2449021 2449021]</ref><ref name="pmid6235834">Goodfellow A, Alaghband-Zadeh J, Carter G, Cream JJ, Holland S, Scully J et al. (1984) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=6235834 Oral spironolactone improves acne vulgaris and reduces sebum excretion.] ''Br J Dermatol'' 111 (2):209-14. PMID: [http://pubmed.gov/6235834 6235834]</ref> | ||
=====Ascites of patients in cirrhosis of liver===== | =====Ascites of patients in cirrhosis of liver===== | ||
| Line 53: | Line 68: | ||
* Dosing information | * Dosing information | ||
:* 100-400 mg/day (300-600 mg/day satisfies 50%-90% patients) | :* '''100-400 mg/day''' ('''300-600 mg/day''' satisfies 50%-90% patients) | ||
:* | :* Recommended initial dosage: '''100-200 mg PO qd ''' | ||
:* 225 mg/day <ref name="pmid9075669">Fernández-Esparrach G, Guevara M, Sort P, Pardo A, Jiménez W, Ginès P et al. (1997) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=9075669 Diuretic requirements after therapeutic paracentesis in non-azotemic patients with cirrhosis. A randomized double-blind trial of spironolactone versus placebo.] ''J Hepatol'' 26 (3):614-20. PMID: [http://pubmed.gov/9075669 9075669]</ref> | :* '''225 mg/day''' <ref name="pmid9075669">Fernández-Esparrach G, Guevara M, Sort P, Pardo A, Jiménez W, Ginès P et al. (1997) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=9075669 Diuretic requirements after therapeutic paracentesis in non-azotemic patients with cirrhosis. A randomized double-blind trial of spironolactone versus placebo.] ''J Hepatol'' 26 (3):614-20. PMID: [http://pubmed.gov/9075669 9075669]</ref> | ||
=====Proteinuria in Chronic renal failure===== | =====Proteinuria in Chronic renal failure===== | ||
| Line 61: | Line 76: | ||
* Dosing information | * Dosing information | ||
:* 25 mg/day <ref name="pmid17035949">Bianchi S, Bigazzi R, Campese VM (2006) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=17035949 Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease.] ''Kidney Int'' 70 (12):2116-23. [http://dx.doi.org/10.1038/sj.ki.5001854 DOI:10.1038/sj.ki.5001854] PMID: [http://pubmed.gov/17035949 17035949]</ref> | :* '''25 mg/day''' <ref name="pmid17035949">Bianchi S, Bigazzi R, Campese VM (2006) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=17035949 Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease.] ''Kidney Int'' 70 (12):2116-23. [http://dx.doi.org/10.1038/sj.ki.5001854 DOI:10.1038/sj.ki.5001854] PMID: [http://pubmed.gov/17035949 17035949]</ref> | ||
=====Proteinuria in diabetic nephropathy===== | =====Proteinuria in diabetic nephropathy===== | ||
| Line 67: | Line 82: | ||
* Dosing information | * Dosing information | ||
:* | :* '''25 mg''' in addition to an [[ACE inhibitor]] or [[angiotensin II]] receptor antagonist <ref name="pmid16775595">Schjoedt KJ, Rossing K, Juhl TR, Boomsma F, Tarnow L, Rossing P et al. (2006) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=16775595 Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy.] ''Kidney Int'' 70 (3):536-42. [http://dx.doi.org/10.1038/sj.ki.5001580 DOI:10.1038/sj.ki.5001580] PMID: [http://pubmed.gov/16775595 16775595]</ref> | ||
=====Hirsutism===== | =====Hirsutism===== | ||
| Line 73: | Line 88: | ||
* Dosing information | * Dosing information | ||
:* | :* Spironolactone plus [[cyproterone]]/[[ethinyl estradiol]] or [[flutamide]] alone were both significantly effective for the treatment of women with moderate to severe hirsutism in a prospective, randomized, clinical trial <ref name="pmid18389188">Karakurt F, Sahin I, Güler S, Demirbas B, Culha C, Serter R et al. (2008) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18389188 Comparison of the clinical efficacy of flutamide and spironolactone plus ethinyloestradiol/cyproterone acetate in the treatment of hirsutism: a randomised controlled study.] ''Adv Ther'' 25 (4):321-8. [http://dx.doi.org/10.1007/s12325-008-0039-5 DOI:10.1007/s12325-008-0039-5] PMID: [http://pubmed.gov/18389188 18389188]</ref> | ||
=====Idiopathic edema===== | =====Idiopathic edema===== | ||
| Line 79: | Line 94: | ||
* Dosing information | * Dosing information | ||
:* | :* '''50-200 mg every morning''' or '''[[hydrochlorothiazide]] 25 mg every morning''' <ref name="pmid3081532">Gaby AR (1986) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=3081532 Idiopathic edema: 'overlooked' causes.] ''Hosp Pract (Off Ed)'' 21 (2):21. PMID: [http://pubmed.gov/3081532 3081532]</ref><ref name="pmid3934201">Melby JC (1985) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=3934201 Idiopathic edema. A clinical conundrum.] ''Hosp Pract (Off Ed)'' 20 (12):68E-68G, 68J, 68M passim. PMID: [http://pubmed.gov/3934201 3934201]</ref> | ||
=====Myocardial infarction===== | =====Myocardial infarction===== | ||
| Line 85: | Line 100: | ||
* Dosing information | * Dosing information | ||
:* 25 mg/day <ref name="pmid12732605">Hayashi M, Tsutamoto T, Wada A, Tsutsui T, Ishii C, Ohno K et al. (2003) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=12732605 Immediate administration of mineralocorticoid receptor antagonist spironolactone prevents post-infarct left ventricular remodeling associated with suppression of a marker of myocardial collagen synthesis in patients with first anterior acute myocardial infarction.] ''Circulation'' 107 (20):2559-65. [http://dx.doi.org/10.1161/01.CIR.0000068340.96506.0F DOI:10.1161/01.CIR.0000068340.96506.0F] PMID: [http://pubmed.gov/12732605 12732605]</ref> | :* '''25 mg/day''' <ref name="pmid12732605">Hayashi M, Tsutamoto T, Wada A, Tsutsui T, Ishii C, Ohno K et al. (2003) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=12732605 Immediate administration of mineralocorticoid receptor antagonist spironolactone prevents post-infarct left ventricular remodeling associated with suppression of a marker of myocardial collagen synthesis in patients with first anterior acute myocardial infarction.] ''Circulation'' 107 (20):2559-65. [http://dx.doi.org/10.1161/01.CIR.0000068340.96506.0F DOI:10.1161/01.CIR.0000068340.96506.0F] PMID: [http://pubmed.gov/12732605 12732605]</ref> | ||
=====Prophylaxis of osteopenia; | =====Prophylaxis of osteopenia; - Polycystic ovary syndrome===== | ||
* Dosing information | * Dosing information | ||
:* 100 mg PO qd <ref name="pmid10199763">Moghetti P, Castello R, Zamberlan N, Rossini M, Gatti D, Negri C et al. (1999) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=10199763 Spironolactone, but not flutamide, administration prevents bone loss in hyperandrogenic women treated with gonadotropin-releasing hormone agonist.] ''J Clin Endocrinol Metab'' 84 (4):1250-4. [http://dx.doi.org/10.1210/jcem.84.4.5606 DOI:10.1210/jcem.84.4.5606] PMID: [http://pubmed.gov/10199763 10199763]</ref> | :* '''100 mg PO qd''' <ref name="pmid10199763">Moghetti P, Castello R, Zamberlan N, Rossini M, Gatti D, Negri C et al. (1999) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=10199763 Spironolactone, but not flutamide, administration prevents bone loss in hyperandrogenic women treated with gonadotropin-releasing hormone agonist.] ''J Clin Endocrinol Metab'' 84 (4):1250-4. [http://dx.doi.org/10.1210/jcem.84.4.5606 DOI:10.1210/jcem.84.4.5606] PMID: [http://pubmed.gov/10199763 10199763]</ref> | ||
|fdaLIADPed=Safety and effectiveness in pediatric patients have not been established. | |||
|offLabelPedGuideSupport=There is limited information about <i>Off-Label Guideline-Supported Use</i> of Spironolactone in pediatric patients. | |||
|offLabelPedNoGuideSupport======Primary aldosteronism===== | |offLabelPedNoGuideSupport======Primary aldosteronism===== | ||
* Dosing information | * Dosing information | ||
:* | :* Initial dosage: '''400 mg/day''' with gradual reduction to '''200 mg/day''' <ref name="pmid3023598">Batista MC, Mendonça BB, Kater CE, Arnhold IJ, Rocha A, Nicolau W et al. (1986) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=3023598 Spironolactone-reversible rickets associated with 11 beta-hydroxysteroid dehydrogenase deficiency syndrome.] ''J Pediatr'' 109 (6):989-93. PMID: [http://pubmed.gov/3023598 3023598]</ref> | ||
|contraindications=Spironolactone tablets are contraindicated for patients with [[anuria]], [[acute renal insufficiency]], significant impairment of renal excretory function, [[hypercalcemia]], [[hyperkalemia]], [[Addison's disease]] or other conditions associated with [[hyperkalemia]],and with concomitant use of eplerenone. | |contraindications=Spironolactone tablets are contraindicated for patients with [[anuria]], [[acute renal insufficiency]], significant impairment of renal excretory function, [[hypercalcemia]], [[hyperkalemia]], [[Addison's disease]] or other conditions associated with [[hyperkalemia]],and with concomitant use of eplerenone. | ||
|warnings=Potassium supplementation, either in the form of medication or as a diet rich in potassium, should not ordinarily be given in association with | |warnings=Potassium supplementation, either in the form of medication or as a diet rich in potassium, should not ordinarily be given in association with aldactazide therapy. Excessive potassium intake may cause [[hyperkalemia]] in patients receiving [[aldactazide]]. | ||
Concomitant administration of | Concomitant administration of aldactazide with the following drugs or potassium sources may lead to severe [[hyperkalemia]]: | ||
* other potassium-sparing | * other [[potassium-sparing diuretics]] | ||
* [[ACE inhibitors]] | * [[ACE inhibitors]] | ||
* [[angiotensin II receptor antagonists]] | * [[angiotensin II receptor antagonists]] | ||
* [[aldosterone blockers]] | * [[aldosterone blockers]] | ||
* non-steroidal anti-inflammatory drugs ([[NSAIDs]]), e.g., [[indomethacin]] | * [[non-steroidal anti-inflammatory drugs]] ([[NSAIDs]]), e.g., [[indomethacin]] | ||
* [[heparin]] and [[low molecular weight heparin]] | * [[heparin]] and [[low molecular weight heparin]] | ||
* other drugs known to cause [[hyperkalemia]] | * other drugs known to cause [[hyperkalemia]] | ||
* potassium supplements | * [[potassium]] supplements | ||
* diet rich in potassium | * diet rich in [[potassium]] | ||
* salt substitutes containing potassium | * salt substitutes containing [[potassium]] | ||
Spironolactone tablets should not be administered concurrently with other potassium-sparing [[diuretics]]. Spironolactone tablets, when used with [[ACE inhibitors]] or [[indomethacin]], even in the presence of a [[diuretic]], have been associated with severe [[hyperkalemia]]. Extreme caution should be exercised when spironolactone tablets are given concomitantly with these drugs. | * Spironolactone tablets should not be administered concurrently with other potassium-sparing [[diuretics]]. Spironolactone tablets, when used with [[ACE inhibitors]] or [[indomethacin]], even in the presence of a [[diuretic]], have been associated with severe [[hyperkalemia]]. Extreme caution should be exercised when spironolactone tablets are given concomitantly with these drugs. | ||
* Hyperkalemia in patients with severe heart failure | * Hyperkalemia in patients with severe heart failure | ||
:* Hyperkalemia may be fatal. It is critical to monitor and manage serum potassium in patients with severe heart failure receiving spironolactone. Avoid using other potassium-sparing [[diuretics]]. Avoid using oral potassium supplements in patients with serum potassium > 3.5 mEq/L. RALES excluded patients with a serum creatinine > 2.5 mg/dL or a recent increase in serum creatinine > 25%. The recommended monitoring for potassium and creatinine is one week after initiation or increase in dose of spironolactone, monthly for the first 3 months, then quarterly for a year, and then every 6 months. | :* [[Hyperkalemia]] may be fatal. It is critical to monitor and manage serum [[potassium]] in patients with severe heart failure receiving spironolactone. Avoid using other potassium-sparing [[diuretics]]. Avoid using oral [[potassium]] supplements in patients with serum [[potassium]] > 3.5 mEq/L. RALES excluded patients with a serum [[creatinine]] > 2.5 mg/dL or a recent increase in serum [[creatinine]] > 25%. The recommended monitoring for [[potassium]] and [[creatinine]] is one week after initiation or increase in dose of spironolactone, monthly for the first 3 months, then quarterly for a year, and then every 6 months. | ||
:* Discontinue or interrupt treatment for serum potassium > 5 mEq/L or for serum creatinine > 4 mg/dL. | :* Discontinue or interrupt treatment for serum [[potassium]] > 5 mEq/L or for serum [[creatinine]] > 4 mg/dL. | ||
:* Spironolactone tablets should be used with caution in patients with impaired hepatic function because minor alterations of fluid and electrolyte balance may precipitate hepatic coma. | :* Spironolactone tablets should be used with caution in patients with impaired hepatic function because minor alterations of fluid and electrolyte balance may precipitate [[hepatic coma]]. | ||
:* Lithium generally should not be given with [[diuretics]] | :* [[Lithium]] generally should not be given with [[diuretics]] | ||
=====PRECAUTIONS===== | =====PRECAUTIONS===== | ||
| Line 124: | Line 141: | ||
* General | * General | ||
:* All patients receiving diuretic therapy should be observed for evidence of fluid or electrolyte imbalance, e.g., hypomagnesemia, hyponatremia, hypochloremic alkalosis, and hyperkalemia. | :* All patients receiving diuretic therapy should be observed for evidence of fluid or electrolyte imbalance, e.g., [[hypomagnesemia]], [[hyponatremia]], [[hypochloremic alkalosis]], and [[hyperkalemia]]. | ||
:* Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Warning signs or symptoms of fluid and electrolyte imbalance, irrespective of cause, include dryness of the mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, and gastrointestinal disturbances such as nausea and vomiting. Hyperkalemia may occur in patients with impaired renal function or excessive potassium intake and can cause cardiac irregularities, which may be fatal. Consequently, no potassium supplement should ordinarily be given with spironolactone tablets. | :* Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Warning signs or symptoms of fluid and electrolyte imbalance, irrespective of cause, include dryness of the mouth, thirst, [[weakness]], [[lethargy]], [[drowsiness]], [[restlessness]], [[muscle pains]] or [[cramps]], muscular fatigue, [[hypotension]], [[oliguria]], [[tachycardia]], and gastrointestinal disturbances such as [[nausea]] and [[vomiting]]. [[Hyperkalemia]] may occur in patients with impaired renal function or excessive potassium intake and can cause cardiac irregularities, which may be fatal. Consequently, no potassium supplement should ordinarily be given with spironolactone tablets. | ||
:* If hyperkalemia is suspected (warning signs include paresthesia, muscle weakness, fatigue, flaccid paralysis of the extremities, bradycardia, and shock), an electrocardiogram (ECG) should be obtained. However, it is important to monitor serum potassium levels because mild hyperkalemia may not be associated with ECG changes. | :* If [[hyperkalemia]] is suspected (warning signs include [[paresthesia]], [[muscle weakness]], [[fatigue]], [[flaccid paralysis]] of the extremities, [[bradycardia]], and [[shock]]), an [[electrocardiogram]] (ECG) should be obtained. However, it is important to monitor serum potassium levels because mild [[hyperkalemia]] may not be associated with ECG changes. | ||
If hyperkalemia is present, spironolactone tablets should be discontinued immediately. With severe hyperkalemia, the clinical situation dictates the procedures to be employed. These may include the intravenous administration of calcium chloride solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent hyperkalemia may require dialysis. | :* If [[hyperkalemia]] is present, spironolactone tablets should be discontinued immediately. With severe [[hyperkalemia]], the clinical situation dictates the procedures to be employed. These may include the intravenous administration of [[calcium chloride]] solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent [[hyperkalemia]] may require dialysis. | ||
:* Reversible hyperchloremic metabolic acidosis, usually in association with hyperkalemia, has been reported to occur in some patients with decompensated hepatic cirrhosis, even in the presence of normal renal function. | :* Reversible [[hyperchloremic metabolic acidosis]], usually in association with [[hyperkalemia]], has been reported to occur in some patients with decompensated [[hepatic cirrhosis]], even in the presence of normal renal function. | ||
:* Dilutional hyponatremia, manifested by dryness of the mouth, thirst, lethargy, and drowsiness, and confirmed by a low serum sodium level, may be caused or aggravated, especially when spironolactone tablets are administered in combination with other [[diuretics]], and dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction rather than administration of sodium, except in rare instances when the hyponatremia is life-threatening. | :* Dilutional [[hyponatremia]], manifested by [[Dry mouth|dryness of the mouth]], [[thirst]], [[lethargy]], and [[drowsiness]], and confirmed by a low serum sodium level, may be caused or aggravated, especially when spironolactone tablets are administered in combination with other [[diuretics]], and dilutional [[hyponatremia]] may occur in [[edematous]] patients in hot weather; appropriate therapy is water restriction rather than administration of sodium, except in rare instances when the [[hyponatremia]] is life-threatening. | ||
:* Spironolactone therapy may cause a transient elevation of BUN, especially in patients with pre-existing renal impairment. Spironolactone tablets may cause mild acidosis. | :* Spironolactone therapy may cause a transient elevation of [[BUN]], especially in patients with pre-existing renal impairment. Spironolactone tablets may cause mild [[acidosis]]. | ||
:* Gynecomastia may develop in association with the use of spironolactone; physicians should be alert to its possible onset. The development of gynecomastia appears to be related to both dosage level and duration of therapy and is normally reversible when spironolactone tablets are discontinued. In rare instances some breast enlargement may persist when spironolactone tablets are discontinued. | :* [[Gynecomastia]] may develop in association with the use of spironolactone; physicians should be alert to its possible onset. The development of [[gynecomastia]] appears to be related to both dosage level and duration of therapy and is normally reversible when spironolactone tablets are discontinued. In rare instances some breast enlargement may persist when spironolactone tablets are discontinued. | ||
:* Somnolence and dizziness have been reported to occur in some patients. Caution is advised when driving or operating machinery until the response to initial treatment has been determined. | :* [[Somnolence]] and [[dizziness]] have been reported to occur in some patients. Caution is advised when driving or operating machinery until the response to initial treatment has been determined. | ||
|clinicalTrials=:* Digestive: Gastric bleeding, [[ulceration]], [[gastritis]], [[diarrhea]] and [[cramping]], [[nausea]], [[vomiting]].<BR> | |clinicalTrials=:* Digestive: Gastric bleeding, [[ulceration]], [[gastritis]], [[diarrhea]] and [[cramping]], [[nausea]], [[vomiting]].<BR> | ||
:* Reproductive: [[Gynecomastia]] | :* Reproductive: [[Gynecomastia]], inability to achieve or maintain erection, irregular menses or [[amenorrhea]], [[postmenopausal bleeding]], breast pain. [[Carcinoma of the breast]] has been reported in patients taking spironolactone but a cause and effect relationship has not been established.<BR> | ||
:* Hematologic: [[Leukopenia]] (including [[agranulocytosis]]), [[thrombocytopenia]].<BR> | :* Hematologic: [[Leukopenia]] (including [[agranulocytosis]]), [[thrombocytopenia]].<BR> | ||
:* Hypersensitivity: [[Fever]], [[urticaria]], [[maculopapular]] or [[erythematous cutaneous eruptions]], <BR>[[anaphylactic reactions]], [[vasculitis]]. | :* Hypersensitivity: [[Fever]], [[urticaria]], [[maculopapular]] or [[erythematous cutaneous eruptions]], <BR>[[anaphylactic reactions]], [[vasculitis]]. | ||
:* Metabolism: [[Hyperkalemia]], electrolyte disturbances | :* Metabolism: [[Hyperkalemia]], electrolyte disturbances.<BR> | ||
:* Musculoskeletal: Leg cramps.<BR> | :* Musculoskeletal: [[Leg cramps]].<BR> | ||
:* Nervous system/psychiatric: [[Lethargy]], mental confusion, [[ataxia]], [[dizziness]], [[headache]], [[drowsiness]].<BR> | :* Nervous system/psychiatric: [[Lethargy]], [[mental confusion]], [[ataxia]], [[dizziness]], [[headache]], [[drowsiness]].<BR> | ||
:* Liver/biliary: A very few cases of mixed cholestatic/hepatocellular toxicity, with one reported fatality, have been reported with spironolactone administration.<BR> | :* Liver/biliary: A very few cases of mixed cholestatic/[[hepatocellular toxicity]], with one reported fatality, have been reported with spironolactone administration.<BR> | ||
:* Renal: [[Renal dysfunction]] (including renal failure).<BR> | :* Renal: [[Renal dysfunction]] (including [[renal failure]]).<BR> | ||
:* Skin: Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN), drug rash with [[eosinophilia]] and systemic symptoms (DRESS), [[alopecia]], [[pruritus]].<BR> | :* Skin: [[Stevens-Johnson Syndrome]] ([[SJS]]), [[toxic epidermal necrolysis]] ([[TEN]]), [[drug rash]] with [[eosinophilia]] and systemic symptoms (DRESS), [[alopecia]], [[pruritus]].<BR> | ||
|postmarketing=There is limited information about the post marketing experience. | |||
|drugInteractions=[[ACE inhibitors]], [[Angiotensin II receptor antagonists]], [[aldosterone blockers]], [[potassium supplements]], [[heparin]], [[low molecular weight heparin]], and other drugs known to cause [[hyperkalemia]]: | |drugInteractions=[[ACE inhibitors]], [[Angiotensin II receptor antagonists]], [[aldosterone blockers]], [[potassium supplements]], [[heparin]], [[low molecular weight heparin]], and other drugs known to cause [[hyperkalemia]]: | ||
:* Concomitant administration may lead to severe [[hyperkalemia]]. | :* Concomitant administration may lead to severe [[hyperkalemia]]. | ||
:* Alcohol, [[barbiturates]], or [[narcotics]]: Potentiation of orthostatic [[hypotension]] may occur. | :* [[Alcohol]], [[barbiturates]], or [[narcotics]]: Potentiation of orthostatic [[hypotension]] may occur. | ||
:* [[Antidiabetic]] drugs (e.g., oral agents, insulin): Dosage adjustment of the antidiabetic drug may be required | :* [[Antidiabetic]] drugs (e.g., oral agents, insulin): Dosage adjustment of the antidiabetic drug may be required. | ||
:* [[Corticosteroids]], [[ACTH]]: Intensified electrolyte depletion, particularly [[hypokalemia]], may occur. | :* [[Corticosteroids]], [[ACTH]]: Intensified electrolyte depletion, particularly [[hypokalemia]], may occur. | ||
:* Pressor amines (e.g., [[norepinephrine]]): Both [[spironolactone]] and [[hydrochlorothiazide]] reduce the vascular responsiveness to [[norepinephrine]]. Therefore, caution should be exercised in the management of patients subjected to regional or [[general anesthesia]] while they are being treated with | :* Pressor amines (e.g., [[norepinephrine]]): Both [[spironolactone]] and [[hydrochlorothiazide]] reduce the vascular responsiveness to [[norepinephrine]]. Therefore, caution should be exercised in the management of patients subjected to regional or [[general anesthesia]] while they are being treated with aldactazide. | ||
:* Skeletal muscle relaxants, [[nondepolarizing]] (e.g., [[tubocurarine]]): Possible increased responsiveness to the muscle relaxant may result. | :* [[Skeletal muscle relaxants]], [[nondepolarizing]] (e.g., [[tubocurarine]]): Possible increased responsiveness to the muscle relaxant may result. | ||
:* Lithium: Lithium generally should not be given with [[diuretics]]. [[Diuretic]] agents reduce the renal clearance of lithium and add a high risk of lithium toxicity. | :* Lithium: [[Lithium]] generally should not be given with [[diuretics]]. [[Diuretic]] agents reduce the renal clearance of lithium and add a high risk of [[lithium toxicity]]. | ||
:* Nonsteroidal anti-inflammatory drugs ([[NSAIDs]]): In some patients, the administration of an NSAID can reduce the [[diuretic]], [[natriuretic]], and [[antihypertensive]] effects of loop, potassium-sparing, and [[thiazide diuretics]]. Combination of NSAIDs, e.g., [[indomethacin]], with potassium-sparing [[diuretics]] has been associated with severe [[hyperkalemia]]. Therefore, when | :* Nonsteroidal anti-inflammatory drugs ([[NSAIDs]]): In some patients, the administration of an [[NSAID]] can reduce the [[diuretic]], [[natriuretic]], and [[antihypertensive]] effects of loop, potassium-sparing, and [[thiazide diuretics]]. Combination of [[NSAIDs]], e.g., [[indomethacin]], with potassium-sparing [[diuretics]] has been associated with severe [[hyperkalemia]]. Therefore, when [[aldactazide]] and [[NSAIDs]] are used concomitantly, the patient should be observed closely to determine if the desired effect of the [[diuretic]] is obtained. | ||
:* [[Digoxin]]: [[Spironolactone]] has been shown to increase the half-life of [[digoxin]]. This may result in increased serum [[digoxin]] levels and subsequent digitalis toxicity. Monitor serum [[digoxin]] levels and adjust dose accordingly. Thiazide-induced electrolyte disturbances, i.e. [[hypokalemia]], [[hypomagnesemia]], increase the risk of [[digoxin]] toxicity, which may lead to fatal arrhythmic events | :* [[Digoxin]]: [[Spironolactone]] has been shown to increase the half-life of [[digoxin]]. This may result in increased serum [[digoxin]] levels and subsequent digitalis toxicity. Monitor serum [[digoxin]] levels and adjust dose accordingly. Thiazide-induced electrolyte disturbances, i.e. [[hypokalemia]], [[hypomagnesemia]], increase the risk of [[digoxin]] toxicity, which may lead to fatal arrhythmic events . | ||
:* [[Cholestyramine]]: Hyperkalemic metabolic acidosis has been reported in patients given [[spironolactone]] concurrently with [[cholestyramine]]. | :* [[Cholestyramine]]: [[Hyperkalemic metabolic acidosis]] has been reported in patients given [[spironolactone]] concurrently with [[cholestyramine]]. | ||
=====Drug/Laboratory test interactions===== | =====Drug/Laboratory test interactions===== | ||
:* [[Thiazides]] should be discontinued before carrying out tests for parathyroid function | :* [[Thiazides]] should be discontinued before carrying out tests for parathyroid function. [[Thiazides]] may also decrease serum PBI levels without evidence of alteration of thyroid function. | ||
:* Several reports of possible interference with [[digoxin]] [[radioimmunoassays]] by [[spironolactone]] or its metabolites have appeared in the literature. Neither the extent nor the potential clinical significance of its interference (which may be assay specific) has been fully established. | :* Several reports of possible interference with [[digoxin]] [[radioimmunoassays]] by [[spironolactone]] or its metabolites have appeared in the literature. Neither the extent nor the potential clinical significance of its interference (which may be assay specific) has been fully established. | ||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA=Teratology studies with [[spironolactone]] have been carried out in mice and rabbits at doses of up to 20 mg/kg/day. On a body surface area basis, this dose in the mouse is substantially below the maximum recommended human dose and, in the rabbit, approximates the maximum recommended human dose. No teratogenic or other embryotoxic effects were observed in mice, but the 20 mg/kg dose caused an increased rate of resorption and a lower number of live fetuses in rabbits. Because of its antiandrogenic activity and the requirement of testosterone for male morphogenesis, [[spironolactone]] may have the potential for adversely affecting sex differentiation of the male during embryogenesis. When administered to rats at 200 mg/kg/day between gestation days 13 and 21 (late embryogenesis and fetal development), feminization of male fetuses was observed. Offspring exposed during late pregnancy to 50 and 100 mg/kg/day doses of [[spironolactone]] exhibited changes in the reproductive tract including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction, that persisted into adulthood. There are no adequate and well-controlled studies with [[spironolactone]] and [[hydrochlorothiazide]] tablets in pregnant women. Spironolactone has known endocrine effects in animals including [[progestational]] and antiandrogenic effects. The antiandrogenic effects can result in apparent [[estrogenic]] side effects in humans, such as [[gynecomastia]]. Therefore, the use of [[spironolactone]] and [[hydrochlorothiazide]] tablets in pregnant women requires that the anticipated benefit be weighed against the possible hazards to the fetus. | |useInPregnancyFDA=Teratology studies with [[spironolactone]] have been carried out in mice and rabbits at doses of up to 20 mg/kg/day. On a body surface area basis, this dose in the mouse is substantially below the maximum recommended human dose and, in the rabbit, approximates the maximum recommended human dose. No teratogenic or other embryotoxic effects were observed in mice, but the 20 mg/kg dose caused an increased rate of resorption and a lower number of live fetuses in rabbits. Because of its antiandrogenic activity and the requirement of testosterone for male morphogenesis, [[spironolactone]] may have the potential for adversely affecting sex differentiation of the male during embryogenesis. When administered to rats at 200 mg/kg/day between gestation days 13 and 21 (late embryogenesis and fetal development), feminization of male fetuses was observed. Offspring exposed during late pregnancy to 50 and 100 mg/kg/day doses of [[spironolactone]] exhibited changes in the reproductive tract including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction, that persisted into adulthood. There are no adequate and well-controlled studies with [[spironolactone]] and [[hydrochlorothiazide]] tablets in pregnant women. Spironolactone has known endocrine effects in animals including [[progestational]] and antiandrogenic effects. The antiandrogenic effects can result in apparent [[estrogenic]] side effects in humans, such as [[gynecomastia]]. Therefore, the use of [[spironolactone]] and [[hydrochlorothiazide]] tablets in pregnant women requires that the anticipated benefit be weighed against the possible hazards to the fetus. | ||
|useInNursing=Canrenone, a major (and active) metabolite of spironolactone, appears in human breast milk. Because spironolactone has been found to be tumorigenic in rats, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother. If use of the drug is deemed essential, an alternative method of infant feeding should be instituted. | |useInNursing=* Canrenone, a major (and active) metabolite of spironolactone, appears in human breast milk. Because spironolactone has been found to be tumorigenic in rats, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother. If use of the drug is deemed essential, an alternative method of infant feeding should be instituted. | ||
|useInPed=Safety and effectiveness in pediatric patients have not been established. | |useInPed=Safety and effectiveness in pediatric patients have not been established. | ||
|administration======Primary | |administration======Primary hyperaldosteronism===== | ||
Spironolactone tablets may be employed as an initial diagnostic measure to provide presumptive evidence of primary [[hyperaldosteronism]] while patients are on normal diets. | * Spironolactone tablets may be employed as an initial diagnostic measure to provide presumptive evidence of primary [[hyperaldosteronism]] while patients are on normal diets. | ||
======Long test====== | ======Long test====== | ||
Spironolactone tablets are administered at a daily dosage of 400 mg for three to four weeks. Correction of [[hypokalemia]]and of hypertension provides presumptive evidence for the diagnosis of primary [[hyperaldosteronism]]. | * Spironolactone tablets are administered at a daily dosage of 400 mg for three to four weeks. Correction of [[hypokalemia]]and of hypertension provides presumptive evidence for the diagnosis of primary [[hyperaldosteronism]]. | ||
======Short test====== | ======Short test====== | ||
Spironolactone tablets are administered at a daily dosage of 400 mg for four days. If serum potassium increases during spironolactone administration but drops when spironolactone tablets are discontinued, a presumptive diagnosis of primary [[hyperaldosteronism]] should be considered. | * Spironolactone tablets are administered at a daily dosage of 400 mg for four days. If serum potassium increases during spironolactone administration but drops when spironolactone tablets are discontinued, a presumptive diagnosis of primary [[hyperaldosteronism]] should be considered. | ||
After the diagnosis of [[hyperaldosteronism]] has been established by more definitive testing procedures, spironolactone tablets may be administered in doses of 100 to 400 mg daily in preparation for surgery. For patients who are considered unsuitable for surgery, spironolactone tablets may be employed for long-term maintenance therapy at the lowest effective dosage determined for the individual patient. | After the diagnosis of [[hyperaldosteronism]] has been established by more definitive testing procedures, spironolactone tablets may be administered in doses of 100 to 400 mg daily in preparation for surgery. For patients who are considered unsuitable for surgery, spironolactone tablets may be employed for long-term maintenance therapy at the lowest effective dosage determined for the individual patient. | ||
=====Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)===== | =====Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)===== | ||
An initial daily dosage of 100 mg of spironolactone tablets administered in either single or divided doses is recommended, but may range from 25 to 200 mg daily. When given as the sole agent for [[diuresis]], spironolactone tablets should be continued for at least five days at the initial dosage level, after which it may be adjusted to the optimal therapeutic or maintenance level administered in either single or divided daily doses. If, after five days, an adequate [[diuretic]] response to spironolactone tablets has not occurred, a second [[diuretic]] that acts more proximally in the renal tubule may be added to the regimen. Because of the additive effect of spironolactone tablets when administered concurrently with such [[diuretics]], an enhanced [[diuresis]] usually begins on the first day of combined treatment; combined therapy is indicated when more rapid [[diuresis]] is desired. The dosage of spironolactone tablets should remain unchanged when other [[diuretic]] therapy is added. | * An initial daily dosage of 100 mg of spironolactone tablets administered in either single or divided doses is recommended, but may range from 25 to 200 mg daily. When given as the sole agent for [[diuresis]], spironolactone tablets should be continued for at least five days at the initial dosage level, after which it may be adjusted to the optimal therapeutic or maintenance level administered in either single or divided daily doses. If, after five days, an adequate [[diuretic]] response to spironolactone tablets has not occurred, a second [[diuretic]] that acts more proximally in the renal tubule may be added to the regimen. Because of the additive effect of spironolactone tablets when administered concurrently with such [[diuretics]], an enhanced [[diuresis]] usually begins on the first day of combined treatment; combined therapy is indicated when more rapid [[diuresis]] is desired. The dosage of spironolactone tablets should remain unchanged when other [[diuretic]] therapy is added. | ||
=====Essential hypertension===== | =====Essential hypertension===== | ||
For adults, an initial daily dosage of 50 to 100 mg of spironolactone tablets administered in either single or divided doses is recommended. Spironolactone tablets may also be given with [[diuretics]] that act more proximally in the renal tubule or with other antihypertensive agents. Treatment with spironolactone tablets should be continued for at least two weeks, since the maximum response may not occur before this time. Subsequently, dosage should be adjusted according to the response of the patient. | * For adults, an initial daily dosage of 50 to 100 mg of spironolactone tablets administered in either single or divided doses is recommended. Spironolactone tablets may also be given with [[diuretics]] that act more proximally in the renal tubule or with other antihypertensive agents. Treatment with spironolactone tablets should be continued for at least two weeks, since the maximum response may not occur before this time. Subsequently, dosage should be adjusted according to the response of the patient. | ||
=====Hypokalemia===== | =====Hypokalemia===== | ||
Spironolactone tablets in a dosage ranging from 25 mg to 100 mg daily are useful in treating a diuretic-induced [[hypokalemia]], when oral potassium supplements or other potassium-sparing regimens are considered inappropriate. | * Spironolactone tablets in a dosage ranging from 25 mg to 100 mg daily are useful in treating a diuretic-induced [[hypokalemia]], when oral potassium supplements or other potassium-sparing regimens are considered inappropriate. | ||
=====Severe heart failure in conjunction with standard therapy (NYHA class III – IV)===== | =====Severe heart failure in conjunction with standard therapy (NYHA class III – IV)===== | ||
Treatment should be initiated with spironolactone 25 mg once daily if the patient's serum potassium is ≤5.0 mEq/L and the patient's serum creatinine is ≤ 2.5 mg/dL. Patients who tolerate 25 mg once daily may have their dosage increased to 50 mg once daily as clinically indicated. Patients who do not tolerate 25 mg once-daily dose may have their dosage reduced to 25 mg every other day. | * Treatment should be initiated with spironolactone 25 mg once daily if the patient's serum [[potassium]] is ≤5.0 mEq/L and the patient's serum [[creatinine]] is ≤ 2.5 mg/dL. Patients who tolerate 25 mg once daily may have their dosage increased to 50 mg once daily as clinically indicated. Patients who do not tolerate 25 mg once-daily dose may have their dosage reduced to 25 mg every other day. [[Hyperkalemia]] in patients with severe [[heart failure]][[Spironolactone]] for advice on monitoring serum [[potassium]] and serum [[creatinine]]. | ||
|overdose=The oral LD50 of spironolactone is greater than 1,000 mg/kg in mice, rats, and rabbits. | |monitoring=* It is critical to monitor and manage serum potassium in patients with severe [[heart failure]] receiving spironolactone | ||
Acute overdosage of spironolactone may be manifested by [[drowsiness]], mental confusion, [[maculopapular]] or [[erythematous rash]], [[nausea]], [[vomiting]], [[dizziness]], or [[diarrhea]]. Rarely, instances of [[hyponatremia]], [[hyperkalemia]], or [[hepatic coma]] may occur in patients with severe liver disease, but these are unlikely due to acute overdosage. [[Hyperkalemia]] may occur, especially in patients with impaired renal function. | * The recommended monitoring for [[potassium]] and [[creatinine]] is one week after initiation or increase in dose of spironolactone, monthly for the first 3 months, then quarterly for a year, and then every 6 months. | ||
* Monitoring serum [[potassium]] and serum [[creatinine]] for patients with [[hyperkalemia]] and [[heart failure]]. | |||
|IVCompat=There is limited information about the IV Compatibility. | |||
|overdose=* The oral LD50 of spironolactone is greater than 1,000 mg/kg in mice, rats, and rabbits. | |||
* Acute overdosage of spironolactone may be manifested by [[drowsiness]], [[mental confusion]], [[maculopapular]] or [[erythematous rash]], [[nausea]], [[vomiting]], [[dizziness]], or [[diarrhea]]. Rarely, instances of [[hyponatremia]], [[hyperkalemia]], or [[hepatic coma]] may occur in patients with severe liver disease, but these are unlikely due to acute overdosage. [[Hyperkalemia]] may occur, especially in patients with impaired renal function. | |||
=====Treatment===== | =====Treatment===== | ||
Induce vomiting or evacuate the stomach by lavage. There is no specific [[antidote]]. Treatment is supportive to maintain [[hydration]], electrolyte balance, and vital functions. | * Induce vomiting or evacuate the stomach by lavage. There is no specific [[antidote]]. Treatment is supportive to maintain [[hydration]], electrolyte balance, and vital functions. | ||
Patients who have renal impairment may develop spironolactone-induced [[hyperkalemia]]. In such cases, spironolactone tablets should be discontinued immediately. With severe [[hyperkalemia]], the clinical situation dictates the procedures to be employed. These may include the intravenous administration of calcium chloride solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent [[hyperkalemia]] may require dialysis. | * Patients who have renal impairment may develop spironolactone-induced [[hyperkalemia]]. In such cases, spironolactone tablets should be discontinued immediately. With severe [[hyperkalemia]], the clinical situation dictates the procedures to be employed. These may include the intravenous administration of calcium chloride solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent [[hyperkalemia]] may require [[dialysis]]. | ||
|mechAction=Spironolactone is a specific pharmacologic antagonist of [[aldosterone]], acting primarily through competitive binding of receptors at the [[aldosterone]]-dependent sodium-potassium exchange site in the distal convoluted renal tubule. Spironolactone causes increased amounts of sodium and water to be excreted, while potassium is retained. Spironolactone acts both as a [[diuretic]] and as an antihypertensive drug by this mechanism. It may be given alone or with other [[diuretic]] agents that act more proximally in the renal tubule. | |drugBox={{Drugbox2 | ||
| Watchedfields = changed | |||
| verifiedrevid = 470470172 | |||
| IUPAC_name = 7α-acetylthio-3-oxo-17α-pregn-4-ene-21,17-carbolactone<br />or<br />17-hydroxy-7α-mercapto-3-oxo-17α-pregn-4-ene-21-carboxylic acid, γ-lactone acetate | |||
| image = Spironolactone drugbox 01.png | |||
<!--Clinical data--> | |||
| tradename = Aldactone | |||
| Drugs.com = {{drugs.com|monograph|spironolactone}} | |||
| MedlinePlus = a682627 | |||
| pregnancy_AU = B3 | |||
| pregnancy_US = C | |||
| legal_UK = POM | |||
| legal_US = Rx-only | |||
| routes_of_administration = [[Mouth|Oral]] | |||
<!--Pharmacokinetic data--> | |||
| bioavailability = | |||
| protein_bound = 90%+<ref name="Brittain2002">{{cite book | author = Harry G. Brittain | title = Analytical Profiles of Drug Substances and Excipients | url = http://books.google.com/books?id=RMN5zMW64ZEC&pg=PA309 | accessdate = 27 May 2012 | date = 26 November 2002 | publisher = Academic Press | isbn = 978-0-12-260829-2 | page = 309}}</ref> | |||
| metabolism = [[Liver|Hepatic]] [[CYP450]] | |||
| elimination_half-life = 1.3-2 hours | |||
| excretion = [[Urine]], [[bile]] | |||
<!--Identifiers--> | |||
| CASNo_Ref = {{cascite|correct|CAS}} | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 52-01-7 | |||
| ATC_prefix = C03 | |||
| ATC_suffix = DA01 | |||
| ATC_supplemental = | |||
| PubChem = 5833 | |||
| IUPHAR_ligand = 2875 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00421 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 5628 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = 27O7W4T232 | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D00443 | |||
| ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| ChEBI = 9241 | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 1393 | |||
<!--Chemical data--> | |||
| C = 24 | H = 32 | O = 4 | S = 1 | |||
| molecular_weight = 416.574 g/mol | |||
| smiles = O=C5O[C@@]4([C@@]3([C@H]([C@@H]2[C@H](SC(=O)C)C/C1=C/C(=O)CC[C@]1(C)[C@H]2CC3)CC4)C)CC5 | |||
| InChI = 1/C24H32O4S/c1-14(25)29-19-13-15-12-16(26)4-8-22(15,2)17-5-9-23(3)18(21(17)19)6-10-24(23)11-7-20(27)28-24/h12,17-19,21H,4-11,13H2,1-3H3/t17-,18-,19+,21+,22-,23-,24+/m0/s1 | |||
| InChIKey = LXMSZDCAJNLERA-ZHYRCANABW | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C24H32O4S/c1-14(25)29-19-13-15-12-16(26)4-8-22(15,2)17-5-9-23(3)18(21(17)19)6-10-24(23)11-7-20(27)28-24/h12,17-19,21H,4-11,13H2,1-3H3/t17-,18-,19+,21+,22-,23-,24+/m0/s1 | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = LXMSZDCAJNLERA-ZHYRCANASA-N | |||
}} | |||
|mechAction=* Spironolactone is a specific pharmacologic antagonist of [[aldosterone]], acting primarily through competitive binding of receptors at the [[aldosterone]]-dependent sodium-potassium exchange site in the distal convoluted renal tubule. Spironolactone causes increased amounts of sodium and water to be excreted, while potassium is retained. Spironolactone acts both as a [[diuretic]] and as an antihypertensive drug by this mechanism. It may be given alone or with other [[diuretic]] agents that act more proximally in the renal tubule. | |||
=====Aldosterone antagonist activity===== | =====Aldosterone antagonist activity===== | ||
Increased levels of the [[mineralocorticoid]], [[aldosterone]], are present in primary and secondary [[hyperaldosteronism]]. [[Edematous]] states in which secondary [[aldosteronism]] is usually involved include [[congestive heart failure]], [[hepatic cirrhosis]], and [[nephrotic syndrome]]. By competing with [[aldosterone]] for receptor sites, spironolactone tablets provide effective therapy for the [[edema]] and [[ascites]] in those conditions. Spironolactone tablets counteract secondary [[aldosteronism]] induced by the volume depletion and associated sodium loss caused by active [[diuretic]] therapy. | * Increased levels of the [[mineralocorticoid]], [[aldosterone]], are present in primary and secondary [[hyperaldosteronism]]. [[Edematous]] states in which secondary [[aldosteronism]] is usually involved include [[congestive heart failure]], [[hepatic cirrhosis]], and [[nephrotic syndrome]]. By competing with [[aldosterone]] for receptor sites, spironolactone tablets provide effective therapy for the [[edema]] and [[ascites]] in those conditions. Spironolactone tablets counteract secondary [[aldosteronism]] induced by the volume depletion and associated sodium loss caused by active [[diuretic]] therapy. | ||
Spironolactone tablets are effective in lowering the systolic and diastolic blood pressure in patients with primary [[hyperaldosteronism]]. It is also effective in most cases of essential [[hypertension]], despite the fact that aldosterone secretion may be within normal limits in benign essential [[hypertension]]. | * Spironolactone tablets are effective in lowering the systolic and [[diastolic blood pressure]] in patients with primary [[hyperaldosteronism]]. It is also effective in most cases of essential [[hypertension]], despite the fact that [[aldosterone]] secretion may be within normal limits in benign essential [[hypertension]]. | ||
Through its action in antagonizing the effect of [[aldosterone]], spironolactone tablets inhibit the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss. | * Through its action in antagonizing the effect of [[aldosterone]], spironolactone tablets inhibit the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss. | ||
Spironolactone tablets have not been demonstrated to elevate serum uric acid, to precipitate gout, or to alter carbohydrate metabolism. | * Spironolactone tablets have not been demonstrated to elevate serum [[uric acid]], to precipitate [[gout]], or to alter carbohydrate metabolism. | ||
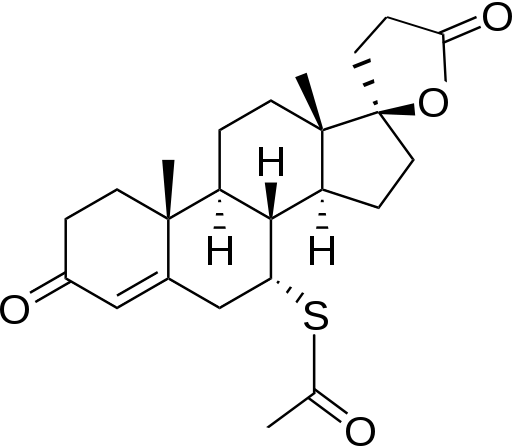
|structure=Spironolactone oral tablets contain 25 mg, 50 mg, or 100 mg of the aldosterone antagonist spironolactone, 17-hydroxy-7α-mercapto-3-oxo-17α-pregn-4-ene-21-carboxylic acid γ-lactone acetate, which has the following structural formula: | |structure=* Spironolactone oral tablets contain 25 mg, 50 mg, or 100 mg of the [[aldosterone antagonist]] spironolactone, 17-hydroxy-7α-mercapto-3-oxo-17α-pregn-4-ene-21-carboxylic acid γ-lactone acetate, which has the following structural formula: | ||
[[File:Spironolactone description table 01.jpg|thumb|none| | [[File:Spironolactone description table 01.jpg|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
Spironolactone is practically insoluble in water, soluble in alcohol, and freely soluble in benzene and in chloroform. | * Spironolactone is practically insoluble in water, soluble in alcohol, and freely soluble in benzene and in chloroform. | ||
Inactive ingredients include calcium sulfate, corn starch, flavor, hypromellose, iron oxide, magnesium stearate, polyethylene glycol, povidone, and titanium dioxide. | Inactive ingredients include calcium sulfate, corn starch, flavor, hypromellose, iron oxide, magnesium stearate, polyethylene glycol, povidone, and titanium dioxide. | ||
|PK=Spironolactone is rapidly and extensively metabolized. Sulfur-containing products are the predominant metabolites and are thought to be primarily responsible, together with spironolactone, for the therapeutic effects of the drug. The following pharmacokinetic data were obtained from 12 healthy volunteers following the administration of 100 mg of spironolactone (ALDACTONE film-coated tablets) daily for 15 days. On the 15th day, spironolactone was given immediately after a lowfat breakfast and blood was drawn thereafter. | |PK=* Spironolactone is rapidly and extensively metabolized. Sulfur-containing products are the predominant metabolites and are thought to be primarily responsible, together with spironolactone, for the therapeutic effects of the drug. The following pharmacokinetic data were obtained from 12 healthy volunteers following the administration of 100 mg of spironolactone (ALDACTONE film-coated tablets) daily for 15 days. On the 15th day, spironolactone was given immediately after a lowfat breakfast and blood was drawn thereafter. | ||
[[File:Spironolactone pharmacology table 01.jpg|thumb|none| | [[File:Spironolactone pharmacology table 01.jpg|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
The pharmacological activity of spironolactone metabolites in man is not known. However, in the [[adrenalectomized]] rat the antimineralocorticoid activities of the metabolites C, TMS, and HTMS, relative to spironolactone, were 1.10, 1.28, and 0.32, respectively. Relative to spironolactone, their binding affinities to the [[aldosterone]] receptors in rat kidney slices were 0.19, 0.86, and 0.06, respectively. | * The pharmacological activity of spironolactone metabolites in man is not known. However, in the [[adrenalectomized]] rat the antimineralocorticoid activities of the metabolites C, TMS, and HTMS, relative to spironolactone, were 1.10, 1.28, and 0.32, respectively. Relative to spironolactone, their binding affinities to the [[aldosterone]] receptors in rat kidney slices were 0.19, 0.86, and 0.06, respectively. | ||
In humans, the potencies of TMS and 7-α-thiospirolactone in reversing the effects of the synthetic [[mineralocorticoid]], [[fludrocortisone]], on urinary electrolyte composition were 0.33 and 0.26, respectively, relative to spironolactone. However, since the serum concentrations of these steroids were not determined, their incomplete absorption and/or first-pass metabolism could not be ruled out as a reason for their reduced in vivo activities. | * In humans, the potencies of TMS and 7-α-thiospirolactone in reversing the effects of the synthetic [[mineralocorticoid]], [[fludrocortisone]], on urinary electrolyte composition were 0.33 and 0.26, respectively, relative to spironolactone. However, since the serum concentrations of these steroids were not determined, their incomplete absorption and/or first-pass metabolism could not be ruled out as a reason for their reduced in vivo activities. | ||
spironolactone and its metabolites are more than 90% bound to plasma proteins. The metabolites are excreted primarily in the urine and secondarily in bile. | spironolactone and its metabolites are more than 90% bound to plasma proteins. The metabolites are excreted primarily in the urine and secondarily in bile. | ||
The effect of food on spironolactone absorption (two 100 mg ALDACTONE tablets) was assessed in a single dose study of 9 healthy, drug-free volunteers. Food increased the bioavailability of unmetabolized spironolactone by almost 100%. The clinical importance of this finding is not known. | The effect of food on spironolactone absorption (two 100 mg ALDACTONE tablets) was assessed in a single dose study of 9 healthy, drug-free volunteers. Food increased the bioavailability of unmetabolized spironolactone by almost 100%. The clinical importance of this finding is not known. | ||
|nonClinToxic=Orally administered spironolactone has been shown to be a tumorigen in dietary administration studies performed in rats, with its proliferative effects manifested on endocrine organs and the liver. In an 18-month study using doses of about 50, 150, and 500 mg/kg/day, there were statistically significant increases in benign [[adenomas]] of the thyroid and testes and, in male rats, a dose-related increase in proliferative changes in the liver (including hepatocytomegaly and [[hyperplastic nodules]]). In a 24-month study in which the same strain of rat was administered doses of about 10, 30 and 100 mg spironolactone/kg/day, the range of proliferative effects included significant increases in hepatocellular adenomas and testicular interstitial cell tumors in males, and significant increases in thyroid follicular cell adenomas and carcinomas in both sexes. There was also a statistically significant, but not dose-related, increase in benign uterine endometrial stromal polyps in females. | |nonClinToxic=* Orally administered spironolactone has been shown to be a tumorigen in dietary administration studies performed in rats, with its proliferative effects manifested on endocrine organs and the [[liver]]. In an 18-month study using doses of about 50, 150, and 500 mg/kg/day, there were statistically significant increases in benign [[adenomas]] of the thyroid and testes and, in male rats, a dose-related increase in proliferative changes in the liver (including hepatocytomegaly and [[hyperplastic nodules]]). In a 24-month study in which the same strain of rat was administered doses of about 10, 30 and 100 mg spironolactone/kg/day, the range of proliferative effects included significant increases in [[hepatocellular adenomas]] and testicular interstitial cell tumors in males, and significant increases in thyroid follicular cell adenomas and carcinomas in both sexes. There was also a statistically significant, but not dose-related, increase in benign uterine endometrial stromal polyps in females.<BR> | ||
A dose-related (above 30 mg/kg/day) incidence of [[myelocytic leukemia]] was observed in rats fed daily doses of potassium [[canrenoate]] (a compound chemically similar to spironolactone and whose primary metabolite, [[canrenone]], is also a major product of spironolactone in man) for a period of one year. In two year studies in the rat, oral administration of potassium [[canrenoate]] was associated with [[myelocytic leukemia]] and hepatic, thyroid, testicular, and mammary tumors. | * A dose-related (above 30 mg/kg/day) incidence of [[myelocytic leukemia]] was observed in rats fed daily doses of potassium [[canrenoate]] (a compound chemically similar to spironolactone and whose primary metabolite, [[canrenone]], is also a major product of spironolactone in man) for a period of one year. In two year studies in the rat, oral administration of potassium [[canrenoate]] was associated with [[myelocytic leukemia]] and hepatic, thyroid, testicular, and mammary tumors.<BR> | ||
Neither spironolactone nor potassium canrenoate produced mutagenic effects in tests using bacteria or yeast. In the absence of metabolic activation, neither spironolactone nor potassium canrenoate has been shown to be mutagenic in mammalian tests in vitro. In the presence of metabolic activation, spironolactone has been reported to be negative in some mammalian mutagenicity tests in vitro and inconclusive (but slightly positive) for mutagenicity in other mammalian tests in vitro. In the presence of metabolic activation, potassium [[canrenoate]] has been reported to test positive for mutagenicity in some mammalian tests in vitro, inconclusive in others, and negative in still others. | * Neither spironolactone nor potassium canrenoate produced mutagenic effects in tests using bacteria or yeast. In the absence of metabolic activation, neither spironolactone nor potassium canrenoate has been shown to be mutagenic in mammalian tests in vitro. In the presence of metabolic activation, spironolactone has been reported to be negative in some mammalian mutagenicity tests in vitro and inconclusive (but slightly positive) for mutagenicity in other mammalian tests in vitro. In the presence of metabolic activation, potassium [[canrenoate]] has been reported to test positive for mutagenicity in some mammalian tests in vitro, inconclusive in others, and negative in still others.<BR> | ||
In a three-litter reproduction study in which female rats received dietary doses of 15 and 500 mg spironolactone/kg/day, there were no effects on mating and fertility, but there was a small increase in incidence of stillborn pups at 500 mg/kg/day. When injected into female rats (100 mg/kg/day for 7 days, i.p.), spironolactone was found to increase the length of the estrous cycle by prolonging [[diestrus]] during treatment and inducing constant [[diestrus]] during a two week posttreatment observation period. These effects were associated with retarded ovarian follicle development and a reduction in circulating estrogen levels, which would be expected to impair mating, fertility, and fecundity. spironolactone (100 mg/kg/day), administered i.p. to female mice during a two week cohabitation period with untreated males, decreased the number of mated mice that conceived (effect shown to be caused by an inhibition of ovulation) and decreased the number of implanted embryos in those that became pregnant (effect shown to be caused by an inhibition of implantation), and at 200 mg/kg, also increased the latency period to mating. | * In a three-litter reproduction study in which female rats received dietary doses of 15 and 500 mg spironolactone/kg/day, there were no effects on mating and fertility, but there was a small increase in incidence of stillborn pups at 500 mg/kg/day. When injected into female rats (100 mg/kg/day for 7 days, i.p.), spironolactone was found to increase the length of the estrous cycle by prolonging [[diestrus]] during treatment and inducing constant [[diestrus]] during a two week posttreatment observation period. These effects were associated with retarded ovarian follicle development and a reduction in circulating estrogen levels, which would be expected to impair mating, fertility, and fecundity. spironolactone (100 mg/kg/day), administered i.p. to female mice during a two week cohabitation period with untreated males, decreased the number of mated mice that conceived (effect shown to be caused by an inhibition of ovulation) and decreased the number of implanted embryos in those that became pregnant (effect shown to be caused by an inhibition of implantation), and at 200 mg/kg, also increased the latency period to mating. | ||
|clinicalStudies======Severe heart failure===== | |clinicalStudies======Severe heart failure===== | ||
The Randomized Aldactone Evaluation Study (RALES) was a multinational, double-blind study in patients with an ejection fraction of ≤ 35%, a history of New York Heart Association (NYHA) class IV heart failure within 6 months, and class III–IV heart failure at the time of randomization. All patients were required to be taking a loop [[diuretic]] and, if tolerated, an [[ACE inhibitor]]. Patients with a baseline serum creatinine of >2.5 mg/dL or a recent increase of 25% or with a baseline serum potassium of >5.0 mEq/L were excluded. | * The Randomized Aldactone Evaluation Study (RALES) was a multinational, double-blind study in patients with an ejection fraction of ≤ 35%, a history of New York Heart Association (NYHA) class IV heart failure within 6 months, and class III–IV heart failure at the time of randomization. All patients were required to be taking a loop [[diuretic]] and, if tolerated, an [[ACE inhibitor]]. Patients with a baseline serum [[creatinine]] of >2.5 mg/dL or a recent increase of 25% or with a baseline serum potassium of >5.0 mEq/L were excluded. | ||
Patients were randomized 1:1 to spironolactone 25 mg orally once daily or matching placebo. Follow-up visits and laboratory measurements (including serum potassium and creatinine) were performed every four weeks for the first 12 weeks, then every 3 months for the first year, and then every 6 months thereafter. Dosing could be withheld for serious [[hyperkalemia]] or if the serum creatinine increased to >4.0 mg/dL. Patients who were intolerant of the initial dosage regimen had their dose decreased to one tablet every other day at one to four weeks. Patients who were tolerant of one tablet daily at 8 weeks may have had their dose increased to two tablets daily at the discretion of the investigator. | * Patients were randomized 1:1 to spironolactone 25 mg orally once daily or matching placebo. Follow-up visits and laboratory measurements (including serum [[potassium]] and [[creatinine]]) were performed every four weeks for the first 12 weeks, then every 3 months for the first year, and then every 6 months thereafter. Dosing could be withheld for serious [[hyperkalemia]] or if the serum [[creatinine]] increased to >4.0 mg/dL. Patients who were intolerant of the initial dosage regimen had their dose decreased to one tablet every other day at one to four weeks. Patients who were tolerant of one tablet daily at 8 weeks may have had their dose increased to two tablets daily at the discretion of the investigator. | ||
RALES enrolled 1663 patients (3% U.S.) at 195 centers in 15 countries between March 24, 1995 and December 31, 1996. The study population was primarily white (87%, with 7% black, 2% Asian, and 4% other), male (73%), and elderly (median age 67). The median ejection fraction was 0.26. Seventy percent were NYHA class III and 29% class IV. The presumed etiology of [[heart failure]] was [[ischemic]] in 55%, and non-ischemic in 45%. There was a history of [[myocardial infarction]] in 28%, of [[hypertension]] in 24%, and of [[diabetes]] in 22%. The median baseline serum creatinine was 1.2 mg/dL and the median baseline creatinine clearance was 57 mL/min. The mean daily dose at study end for the patients randomized to spironolactone was 26 mg. | * RALES enrolled 1663 patients (3% U.S.) at 195 centers in 15 countries between March 24, 1995 and December 31, 1996. The study population was primarily white (87%, with 7% black, 2% Asian, and 4% other), male (73%), and elderly (median age 67). The median ejection fraction was 0.26. Seventy percent were NYHA class III and 29% class IV. The presumed etiology of [[heart failure]] was [[ischemic]] in 55%, and non-ischemic in 45%. There was a history of [[myocardial infarction]] in 28%, of [[hypertension]] in 24%, and of [[diabetes]] in 22%. The median baseline serum [[creatinine]] was 1.2 mg/dL and the median baseline [[creatinine clearance]] was 57 mL/min. The mean daily dose at study end for the patients randomized to spironolactone was 26 mg. | ||
Concomitant medications included a [[loop diuretic]] in 100% of patients and an [[ACE inhibitor]] in 97%. Other medications used at any time during the study included [[digoxin]] (78%), [[anticoagulants]] (58%), [[aspirin]] (43%), and [[beta-blockers]] (15%). | * Concomitant medications included a [[loop diuretic]] in 100% of patients and an [[ACE inhibitor]] in 97%. Other medications used at any time during the study included [[digoxin]] (78%), [[anticoagulants]] (58%), [[aspirin]] (43%), and [[beta-blockers]] (15%). | ||
The primary endpoint for RALES was time to all-cause mortality. RALES was terminated early, after a mean follow-up of 24 months, because of significant mortality benefit detected on a planned interim analysis. The survival curves by treatment group are shown in Figure 1. | The primary endpoint for RALES was time to all-cause mortality. RALES was terminated early, after a mean follow-up of 24 months, because of significant mortality benefit detected on a planned interim analysis. The survival curves by treatment group are shown in Figure 1. | ||
Figure 1. Survival by Treatment Group in RALES | Figure 1. Survival by Treatment Group in RALES | ||
[[File:Spironolactone clinical studies table 01.jpg|thumb|none|400px]] | [[File:Spironolactone clinical studies table 01.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Spironolactone reduced the risk of death by 30% compared to placebo (p<0.001; 95% confidence interval 18% to 40%). Spironolactone reduced the risk of cardiac death, primarily sudden death and death from progressive [[heart failure]] by 31% compared to placebo (p <0.001; 95% confidence interval 18% to 42%). | * Spironolactone reduced the risk of death by 30% compared to placebo (p<0.001; 95% confidence interval 18% to 40%). Spironolactone reduced the risk of cardiac death, primarily sudden death and death from progressive [[heart failure]] by 31% compared to placebo (p <0.001; 95% confidence interval 18% to 42%). | ||
Spironolactone also reduced the risk of hospitalization for cardiac causes (defined as worsening [[heart failure]], [[angina]], [[ventricular arrhythmias]], or [[myocardial infarction]]) by 30% (p <0.001 95% confidence interval 18% to 41%). Changes in NYHA class were more favorable with spironolactone: In the spironolactone group, NYHA class at the end of the study improved in 41% of patients and worsened in 38% compared to improved in 33% and worsened in 48% in the placebo group (p <0.001). | Spironolactone also reduced the risk of hospitalization for cardiac causes (defined as worsening [[heart failure]], [[angina]], [[ventricular arrhythmias]], or [[myocardial infarction]]) by 30% (p <0.001 95% confidence interval 18% to 41%). Changes in NYHA class were more favorable with spironolactone: In the spironolactone group, NYHA class at the end of the study improved in 41% of patients and worsened in 38% compared to improved in 33% and worsened in 48% in the placebo group (p <0.001). | ||
Mortality hazard ratios for some subgroups are shown in Figure 2. The favorable effect of spironolactone on mortality appeared similar for both genders and all age groups except patients younger than 55; there were too few non-whites in RALES to draw any conclusions about differential effects by race. Spironolactone's benefit appeared greater in patients with low baseline serum potassium levels and less in patients with ejection fractions <0.2. These subgroup analyses must be interpreted cautiously. | * Mortality hazard ratios for some subgroups are shown in Figure 2. The favorable effect of spironolactone on mortality appeared similar for both genders and all age groups except patients younger than 55; there were too few non-whites in RALES to draw any conclusions about differential effects by race. Spironolactone's benefit appeared greater in patients with low baseline serum potassium levels and less in patients with ejection fractions <0.2. These subgroup analyses must be interpreted cautiously. | ||
Figure 2. Hazard Ratios of All-Cause Mortality by Subgroup in RALES | Figure 2. Hazard Ratios of All-Cause Mortality by Subgroup in RALES | ||
[[File:Spironolactone clinical studies table 02.jpg|thumb|none|400px]] | [[File:Spironolactone clinical studies table 02.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Figure 2: The size of each box is proportional to the sample size as well as the event rate. [[LVEF]] denotes [[left ventricular ejection fraction]], Ser Creatinine denotes serum creatinine, Cr Clearance denotes creatinine clearance, and [[ACEI]] denotes [[angiotensin-converting enzyme inhibitor]]. | Figure 2: The size of each box is proportional to the sample size as well as the event rate. [[LVEF]] denotes [[left ventricular ejection fraction]], Ser Creatinine denotes serum creatinine, Cr Clearance denotes creatinine clearance, and [[ACEI]] denotes [[angiotensin-converting enzyme inhibitor]]. | ||
|howSupplied=Spironolactone tablets 25 mg are round, light yellow, film-coated, with G debossed on one side and 5011 on the other side, supplied as: | |howSupplied=* Spironolactone tablets 25 mg are round, light yellow, film-coated, with G debossed on one side and 5011 on the other side, supplied as: | ||
[[File:Spironolactone how supplied table 01.jpg|thumb|none|400px]] | [[File:Spironolactone how supplied table 01.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Spironolactone tablets 50 mg are oval, light orange, scored, film-coated, with 5012 debossed on the scored side and G on the other side, supplied as: | * Spironolactone tablets 50 mg are oval, light orange, scored, film-coated, with 5012 debossed on the scored side and G on the other side, supplied as: | ||
[[File:Spironolactone how supplied table 02.jpg|thumb|none|400px]] | [[File:Spironolactone how supplied table 02.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Spironolactone tablets 100 mg are round, peach-colored, scored, film-coated, with 5013 debossed on the scored side and G on the other side, supplied as: | * Spironolactone tablets 100 mg are round, peach-colored, scored, film-coated, with 5013 debossed on the scored side and G on the other side, supplied as: | ||
[[File:Spironolactone how supplied table 03.jpg|thumb|none|400px]] | [[File:Spironolactone how supplied table 03.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
|storage=Store below 77°F (25°C). | |storage=Store below 77°F (25°C). | ||
|fdaPatientInfo=Patients who receive spironolactone tablets should be advised to avoid potassium supplements and foods containing high levels of potassium, including salt substitutes | |fdaPatientInfo=* Patients who receive spironolactone tablets should be advised to avoid potassium supplements and foods containing high levels of potassium, including salt substitutes. | ||
|alcohol=Concomitant with alcohol, [[barbiturates]], or [[narcotics]] may lead to potentiation of [[orthostatic hypotension]]. | |alcohol=Concomitant with alcohol, [[barbiturates]], or [[narcotics]] may lead to potentiation of [[orthostatic hypotension]]. | ||
|nlmPatientInfo=* For patient information about spironolactone from NLM, click [[spironolactone (patient information)|here]]. | |||
}} | }} | ||
{{PillImage}} | |||
{{LabelImage | {{LabelImage | ||
|fileName=Spironolactone label table 01.jpg | |fileName=Spironolactone label table 01.jpg | ||
| Line 284: | Line 363: | ||
|fileName=Spironolactone panel 04.png | |fileName=Spironolactone panel 04.png | ||
}} | }} | ||
[[Category:Diuretics]] | |||
[[Category:Cardiovascular Drugs]] | |||
[[Category:Drug]] | |||
[[Category:Aldosterone antagonists]] | |||
Latest revision as of 17:10, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2], Rabin Bista, M.B.B.S. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
Spironolactone has been shown to be a tumorigen in chronic toxicity studies in rats. Spironolactone tablets should be used only in those conditions described under Indications and Usage. Unnecessary use of this drug should be avoided.
|
Overview
Spironolactone is an aldosterone antagonist that is FDA approved for the treatment of Primary hyperaldosteronism,edematous conditions of congestive heart failure, Cirrhosis of the liver accompanied by edema and/or ascites, nephrotic syndrome, essential hypertension. There is a Black Box Warning for this drug as shown here. Common adverse reactions include gynecomastia, diarrhea, nausea and vomiting, somnolence, disorder of menstruation, impotence.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Primary hyperaldosteronism
- Dosing Information
- Long test: 400 mg/day PO for 3-4 weeks
- Correction of hypokalemia and of hypertension provides presumptive evidence for the diagnosis of primary hyperaldosteronism.
- Short test: 400 mg/day PO for 4 days
- If serum potassium increases during spironolactone administration but drops when spironolactone tablets are discontinued, a presumptive diagnosis of primary hyperaldosteronism should be considered.
- After the diagnosis: 100-400 mg/dayin preparation for surgery.
- For the patient unsuitable for surgery: spironolactone tablets may be employed for long-term maintenance therapy at the lowest effective dosage determined for the individual patient.
Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)
- Dosing information (given as the sole agent for diuresis)
- Initial dosage: 100 mg/day PO for at least 5 days either single or divided dose.
- Dosage range: 25-200 mg/day
- Dosing information (combination with other diuretic)
- If, after five days, an adequate diuretic response to spironolactone tablets has not occurred, a second diuretic that acts more proximally in the renal tubule may be added to the regimen.
- Because of the additive effect of spironolactone tablets when administered concurrently with such diuretics, an enhanced diuresis usually begins on the first day of combined treatment.
- Combined therapy is indicated when more rapid diuresis is desired. The dosage of spironolactone tablets should remain unchanged when other diuretic therapy is added.
Essential hypertension
- Dosing information
- Initial dosage: 50-100 mg/days PO, in either single or divided doses.
- Duration: at least 2 weeks (since the maximum response may not occur before this time. Subsequently, dosage should be adjusted according to the response of the patient.)
Hypokalemia
- Dosing information
- initial dosage: 50-100 mg/days PO (when oral potassium supplements or other potassium-sparing regimens are considered inappropriate.)
Severe heart failure in conjunction with standard therapy (NYHA class III – IV)
- Dosing information
- Initial dosage: 25 mg PO qd (serum potassium is ≤5.0 mEq/L and the patient's serum creatinine is ≤ 2.5 mg/dL)
- Patient who can tolerate 25 mg once daily: 50 mg PO qd
- Patient who can't tolerate 25 mg once daily: 25 mg PO q.o.d
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Spironolactone in adult patients.
Non–Guideline-Supported Use
Acne vulgaris
- Dosing information
Ascites of patients in cirrhosis of liver
- Dosing information
- 100-400 mg/day (300-600 mg/day satisfies 50%-90% patients)
- Recommended initial dosage: 100-200 mg PO qd
- 225 mg/day [4]
Proteinuria in Chronic renal failure
- Dosing information
- 25 mg/day [5]
Proteinuria in diabetic nephropathy
- Dosing information
- 25 mg in addition to an ACE inhibitor or angiotensin II receptor antagonist [6]
Hirsutism
- Dosing information
- Spironolactone plus cyproterone/ethinyl estradiol or flutamide alone were both significantly effective for the treatment of women with moderate to severe hirsutism in a prospective, randomized, clinical trial [7]
Idiopathic edema
- Dosing information
- 50-200 mg every morning or hydrochlorothiazide 25 mg every morning [8][9]
Myocardial infarction
- Dosing information
- 25 mg/day [10]
Prophylaxis of osteopenia; - Polycystic ovary syndrome
- Dosing information
- 100 mg PO qd [11]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Spironolactone in pediatric patients.
Non–Guideline-Supported Use
Primary aldosteronism
- Dosing information
- Initial dosage: 400 mg/day with gradual reduction to 200 mg/day [12]
Contraindications
Spironolactone tablets are contraindicated for patients with anuria, acute renal insufficiency, significant impairment of renal excretory function, hypercalcemia, hyperkalemia, Addison's disease or other conditions associated with hyperkalemia,and with concomitant use of eplerenone.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
Spironolactone has been shown to be a tumorigen in chronic toxicity studies in rats. Spironolactone tablets should be used only in those conditions described under Indications and Usage. Unnecessary use of this drug should be avoided.
|
Potassium supplementation, either in the form of medication or as a diet rich in potassium, should not ordinarily be given in association with aldactazide therapy. Excessive potassium intake may cause hyperkalemia in patients receiving aldactazide.
Concomitant administration of aldactazide with the following drugs or potassium sources may lead to severe hyperkalemia:
- other potassium-sparing diuretics
- ACE inhibitors
- angiotensin II receptor antagonists
- aldosterone blockers
- non-steroidal anti-inflammatory drugs (NSAIDs), e.g., indomethacin
- heparin and low molecular weight heparin
- other drugs known to cause hyperkalemia
- potassium supplements
- diet rich in potassium
- salt substitutes containing potassium
- Spironolactone tablets should not be administered concurrently with other potassium-sparing diuretics. Spironolactone tablets, when used with ACE inhibitors or indomethacin, even in the presence of a diuretic, have been associated with severe hyperkalemia. Extreme caution should be exercised when spironolactone tablets are given concomitantly with these drugs.
- Hyperkalemia in patients with severe heart failure
- Hyperkalemia may be fatal. It is critical to monitor and manage serum potassium in patients with severe heart failure receiving spironolactone. Avoid using other potassium-sparing diuretics. Avoid using oral potassium supplements in patients with serum potassium > 3.5 mEq/L. RALES excluded patients with a serum creatinine > 2.5 mg/dL or a recent increase in serum creatinine > 25%. The recommended monitoring for potassium and creatinine is one week after initiation or increase in dose of spironolactone, monthly for the first 3 months, then quarterly for a year, and then every 6 months.
- Discontinue or interrupt treatment for serum potassium > 5 mEq/L or for serum creatinine > 4 mg/dL.
- Spironolactone tablets should be used with caution in patients with impaired hepatic function because minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
- Lithium generally should not be given with diuretics
PRECAUTIONS
- General
- All patients receiving diuretic therapy should be observed for evidence of fluid or electrolyte imbalance, e.g., hypomagnesemia, hyponatremia, hypochloremic alkalosis, and hyperkalemia.
- Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Warning signs or symptoms of fluid and electrolyte imbalance, irrespective of cause, include dryness of the mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, and gastrointestinal disturbances such as nausea and vomiting. Hyperkalemia may occur in patients with impaired renal function or excessive potassium intake and can cause cardiac irregularities, which may be fatal. Consequently, no potassium supplement should ordinarily be given with spironolactone tablets.
- If hyperkalemia is suspected (warning signs include paresthesia, muscle weakness, fatigue, flaccid paralysis of the extremities, bradycardia, and shock), an electrocardiogram (ECG) should be obtained. However, it is important to monitor serum potassium levels because mild hyperkalemia may not be associated with ECG changes.
- If hyperkalemia is present, spironolactone tablets should be discontinued immediately. With severe hyperkalemia, the clinical situation dictates the procedures to be employed. These may include the intravenous administration of calcium chloride solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent hyperkalemia may require dialysis.
- Reversible hyperchloremic metabolic acidosis, usually in association with hyperkalemia, has been reported to occur in some patients with decompensated hepatic cirrhosis, even in the presence of normal renal function.
- Dilutional hyponatremia, manifested by dryness of the mouth, thirst, lethargy, and drowsiness, and confirmed by a low serum sodium level, may be caused or aggravated, especially when spironolactone tablets are administered in combination with other diuretics, and dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction rather than administration of sodium, except in rare instances when the hyponatremia is life-threatening.
- Spironolactone therapy may cause a transient elevation of BUN, especially in patients with pre-existing renal impairment. Spironolactone tablets may cause mild acidosis.
- Gynecomastia may develop in association with the use of spironolactone; physicians should be alert to its possible onset. The development of gynecomastia appears to be related to both dosage level and duration of therapy and is normally reversible when spironolactone tablets are discontinued. In rare instances some breast enlargement may persist when spironolactone tablets are discontinued.
- Somnolence and dizziness have been reported to occur in some patients. Caution is advised when driving or operating machinery until the response to initial treatment has been determined.
Adverse Reactions
Clinical Trials Experience
- Digestive: Gastric bleeding, ulceration, gastritis, diarrhea and cramping, nausea, vomiting.
- Reproductive: Gynecomastia, inability to achieve or maintain erection, irregular menses or amenorrhea, postmenopausal bleeding, breast pain. Carcinoma of the breast has been reported in patients taking spironolactone but a cause and effect relationship has not been established.
- Hematologic: Leukopenia (including agranulocytosis), thrombocytopenia.
- Hypersensitivity: Fever, urticaria, maculopapular or erythematous cutaneous eruptions,
anaphylactic reactions, vasculitis. - Metabolism: Hyperkalemia, electrolyte disturbances.
- Musculoskeletal: Leg cramps.
- Nervous system/psychiatric: Lethargy, mental confusion, ataxia, dizziness, headache, drowsiness.
- Liver/biliary: A very few cases of mixed cholestatic/hepatocellular toxicity, with one reported fatality, have been reported with spironolactone administration.
- Renal: Renal dysfunction (including renal failure).
- Skin: Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN), drug rash with eosinophilia and systemic symptoms (DRESS), alopecia, pruritus.
- Digestive: Gastric bleeding, ulceration, gastritis, diarrhea and cramping, nausea, vomiting.
Postmarketing Experience
There is limited information about the post marketing experience.
Drug Interactions
ACE inhibitors, Angiotensin II receptor antagonists, aldosterone blockers, potassium supplements, heparin, low molecular weight heparin, and other drugs known to cause hyperkalemia:
- Concomitant administration may lead to severe hyperkalemia.
- Alcohol, barbiturates, or narcotics: Potentiation of orthostatic hypotension may occur.
- Antidiabetic drugs (e.g., oral agents, insulin): Dosage adjustment of the antidiabetic drug may be required.
- Corticosteroids, ACTH: Intensified electrolyte depletion, particularly hypokalemia, may occur.
- Pressor amines (e.g., norepinephrine): Both spironolactone and hydrochlorothiazide reduce the vascular responsiveness to norepinephrine. Therefore, caution should be exercised in the management of patients subjected to regional or general anesthesia while they are being treated with aldactazide.
- Skeletal muscle relaxants, nondepolarizing (e.g., tubocurarine): Possible increased responsiveness to the muscle relaxant may result.
- Lithium: Lithium generally should not be given with diuretics. Diuretic agents reduce the renal clearance of lithium and add a high risk of lithium toxicity.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): In some patients, the administration of an NSAID can reduce the diuretic, natriuretic, and antihypertensive effects of loop, potassium-sparing, and thiazide diuretics. Combination of NSAIDs, e.g., indomethacin, with potassium-sparing diuretics has been associated with severe hyperkalemia. Therefore, when aldactazide and NSAIDs are used concomitantly, the patient should be observed closely to determine if the desired effect of the diuretic is obtained.
- Digoxin: Spironolactone has been shown to increase the half-life of digoxin. This may result in increased serum digoxin levels and subsequent digitalis toxicity. Monitor serum digoxin levels and adjust dose accordingly. Thiazide-induced electrolyte disturbances, i.e. hypokalemia, hypomagnesemia, increase the risk of digoxin toxicity, which may lead to fatal arrhythmic events .
- Cholestyramine: Hyperkalemic metabolic acidosis has been reported in patients given spironolactone concurrently with cholestyramine.
Drug/Laboratory test interactions
- Thiazides should be discontinued before carrying out tests for parathyroid function. Thiazides may also decrease serum PBI levels without evidence of alteration of thyroid function.
- Several reports of possible interference with digoxin radioimmunoassays by spironolactone or its metabolites have appeared in the literature. Neither the extent nor the potential clinical significance of its interference (which may be assay specific) has been fully established.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Teratology studies with spironolactone have been carried out in mice and rabbits at doses of up to 20 mg/kg/day. On a body surface area basis, this dose in the mouse is substantially below the maximum recommended human dose and, in the rabbit, approximates the maximum recommended human dose. No teratogenic or other embryotoxic effects were observed in mice, but the 20 mg/kg dose caused an increased rate of resorption and a lower number of live fetuses in rabbits. Because of its antiandrogenic activity and the requirement of testosterone for male morphogenesis, spironolactone may have the potential for adversely affecting sex differentiation of the male during embryogenesis. When administered to rats at 200 mg/kg/day between gestation days 13 and 21 (late embryogenesis and fetal development), feminization of male fetuses was observed. Offspring exposed during late pregnancy to 50 and 100 mg/kg/day doses of spironolactone exhibited changes in the reproductive tract including dose-dependent decreases in weights of the ventral prostate and seminal vesicle in males, ovaries and uteri that were enlarged in females, and other indications of endocrine dysfunction, that persisted into adulthood. There are no adequate and well-controlled studies with spironolactone and hydrochlorothiazide tablets in pregnant women. Spironolactone has known endocrine effects in animals including progestational and antiandrogenic effects. The antiandrogenic effects can result in apparent estrogenic side effects in humans, such as gynecomastia. Therefore, the use of spironolactone and hydrochlorothiazide tablets in pregnant women requires that the anticipated benefit be weighed against the possible hazards to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Spironolactone in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Spironolactone during labor and delivery.
Nursing Mothers
- Canrenone, a major (and active) metabolite of spironolactone, appears in human breast milk. Because spironolactone has been found to be tumorigenic in rats, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother. If use of the drug is deemed essential, an alternative method of infant feeding should be instituted.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
There is no FDA guidance on the use of Spironolactone in geriatric settings.
Gender
There is no FDA guidance on the use of Spironolactone with respect to specific gender populations.
Race
There is no FDA guidance on the use of Spironolactone with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Spironolactone in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Spironolactone in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Spironolactone in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Spironolactone in patients who are immunocompromised.
Administration and Monitoring
Administration
Primary hyperaldosteronism
- Spironolactone tablets may be employed as an initial diagnostic measure to provide presumptive evidence of primary hyperaldosteronism while patients are on normal diets.
Long test
- Spironolactone tablets are administered at a daily dosage of 400 mg for three to four weeks. Correction of hypokalemiaand of hypertension provides presumptive evidence for the diagnosis of primary hyperaldosteronism.
Short test
- Spironolactone tablets are administered at a daily dosage of 400 mg for four days. If serum potassium increases during spironolactone administration but drops when spironolactone tablets are discontinued, a presumptive diagnosis of primary hyperaldosteronism should be considered.
After the diagnosis of hyperaldosteronism has been established by more definitive testing procedures, spironolactone tablets may be administered in doses of 100 to 400 mg daily in preparation for surgery. For patients who are considered unsuitable for surgery, spironolactone tablets may be employed for long-term maintenance therapy at the lowest effective dosage determined for the individual patient.
Edema in adults (congestive heart failure, hepatic cirrhosis, or nephrotic syndrome)
- An initial daily dosage of 100 mg of spironolactone tablets administered in either single or divided doses is recommended, but may range from 25 to 200 mg daily. When given as the sole agent for diuresis, spironolactone tablets should be continued for at least five days at the initial dosage level, after which it may be adjusted to the optimal therapeutic or maintenance level administered in either single or divided daily doses. If, after five days, an adequate diuretic response to spironolactone tablets has not occurred, a second diuretic that acts more proximally in the renal tubule may be added to the regimen. Because of the additive effect of spironolactone tablets when administered concurrently with such diuretics, an enhanced diuresis usually begins on the first day of combined treatment; combined therapy is indicated when more rapid diuresis is desired. The dosage of spironolactone tablets should remain unchanged when other diuretic therapy is added.
Essential hypertension
- For adults, an initial daily dosage of 50 to 100 mg of spironolactone tablets administered in either single or divided doses is recommended. Spironolactone tablets may also be given with diuretics that act more proximally in the renal tubule or with other antihypertensive agents. Treatment with spironolactone tablets should be continued for at least two weeks, since the maximum response may not occur before this time. Subsequently, dosage should be adjusted according to the response of the patient.
Hypokalemia
- Spironolactone tablets in a dosage ranging from 25 mg to 100 mg daily are useful in treating a diuretic-induced hypokalemia, when oral potassium supplements or other potassium-sparing regimens are considered inappropriate.
Severe heart failure in conjunction with standard therapy (NYHA class III – IV)
- Treatment should be initiated with spironolactone 25 mg once daily if the patient's serum potassium is ≤5.0 mEq/L and the patient's serum creatinine is ≤ 2.5 mg/dL. Patients who tolerate 25 mg once daily may have their dosage increased to 50 mg once daily as clinically indicated. Patients who do not tolerate 25 mg once-daily dose may have their dosage reduced to 25 mg every other day. Hyperkalemia in patients with severe heart failureSpironolactone for advice on monitoring serum potassium and serum creatinine.
Monitoring
- It is critical to monitor and manage serum potassium in patients with severe heart failure receiving spironolactone
- The recommended monitoring for potassium and creatinine is one week after initiation or increase in dose of spironolactone, monthly for the first 3 months, then quarterly for a year, and then every 6 months.
- Monitoring serum potassium and serum creatinine for patients with hyperkalemia and heart failure.
IV Compatibility
There is limited information about the IV Compatibility.
Overdosage
- The oral LD50 of spironolactone is greater than 1,000 mg/kg in mice, rats, and rabbits.
- Acute overdosage of spironolactone may be manifested by drowsiness, mental confusion, maculopapular or erythematous rash, nausea, vomiting, dizziness, or diarrhea. Rarely, instances of hyponatremia, hyperkalemia, or hepatic coma may occur in patients with severe liver disease, but these are unlikely due to acute overdosage. Hyperkalemia may occur, especially in patients with impaired renal function.
Treatment
- Induce vomiting or evacuate the stomach by lavage. There is no specific antidote. Treatment is supportive to maintain hydration, electrolyte balance, and vital functions.
- Patients who have renal impairment may develop spironolactone-induced hyperkalemia. In such cases, spironolactone tablets should be discontinued immediately. With severe hyperkalemia, the clinical situation dictates the procedures to be employed. These may include the intravenous administration of calcium chloride solution, sodium bicarbonate solution and/or the oral or parenteral administration of glucose with a rapid-acting insulin preparation. These are temporary measures to be repeated as required. Cationic exchange resins such as sodium polystyrene sulfonate may be orally or rectally administered. Persistent hyperkalemia may require dialysis.
Pharmacology
Mechanism of Action
- Spironolactone is a specific pharmacologic antagonist of aldosterone, acting primarily through competitive binding of receptors at the aldosterone-dependent sodium-potassium exchange site in the distal convoluted renal tubule. Spironolactone causes increased amounts of sodium and water to be excreted, while potassium is retained. Spironolactone acts both as a diuretic and as an antihypertensive drug by this mechanism. It may be given alone or with other diuretic agents that act more proximally in the renal tubule.
Aldosterone antagonist activity
- Increased levels of the mineralocorticoid, aldosterone, are present in primary and secondary hyperaldosteronism. Edematous states in which secondary aldosteronism is usually involved include congestive heart failure, hepatic cirrhosis, and nephrotic syndrome. By competing with aldosterone for receptor sites, spironolactone tablets provide effective therapy for the edema and ascites in those conditions. Spironolactone tablets counteract secondary aldosteronism induced by the volume depletion and associated sodium loss caused by active diuretic therapy.
- Spironolactone tablets are effective in lowering the systolic and diastolic blood pressure in patients with primary hyperaldosteronism. It is also effective in most cases of essential hypertension, despite the fact that aldosterone secretion may be within normal limits in benign essential hypertension.
- Through its action in antagonizing the effect of aldosterone, spironolactone tablets inhibit the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
- Spironolactone tablets have not been demonstrated to elevate serum uric acid, to precipitate gout, or to alter carbohydrate metabolism.
Structure
- Spironolactone oral tablets contain 25 mg, 50 mg, or 100 mg of the aldosterone antagonist spironolactone, 17-hydroxy-7α-mercapto-3-oxo-17α-pregn-4-ene-21-carboxylic acid γ-lactone acetate, which has the following structural formula:
- Spironolactone is practically insoluble in water, soluble in alcohol, and freely soluble in benzene and in chloroform.
Inactive ingredients include calcium sulfate, corn starch, flavor, hypromellose, iron oxide, magnesium stearate, polyethylene glycol, povidone, and titanium dioxide.
Pharmacodynamics
There is limited information regarding Spironolactone Pharmacodynamics in the drug label.
Pharmacokinetics
- Spironolactone is rapidly and extensively metabolized. Sulfur-containing products are the predominant metabolites and are thought to be primarily responsible, together with spironolactone, for the therapeutic effects of the drug. The following pharmacokinetic data were obtained from 12 healthy volunteers following the administration of 100 mg of spironolactone (ALDACTONE film-coated tablets) daily for 15 days. On the 15th day, spironolactone was given immediately after a lowfat breakfast and blood was drawn thereafter.
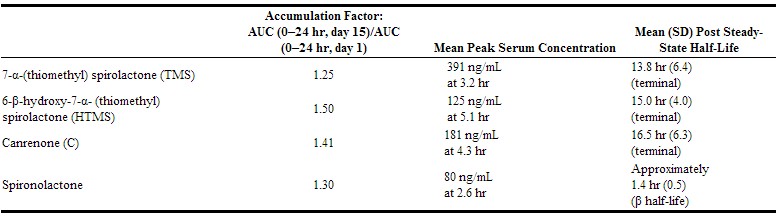
- The pharmacological activity of spironolactone metabolites in man is not known. However, in the adrenalectomized rat the antimineralocorticoid activities of the metabolites C, TMS, and HTMS, relative to spironolactone, were 1.10, 1.28, and 0.32, respectively. Relative to spironolactone, their binding affinities to the aldosterone receptors in rat kidney slices were 0.19, 0.86, and 0.06, respectively.
- In humans, the potencies of TMS and 7-α-thiospirolactone in reversing the effects of the synthetic mineralocorticoid, fludrocortisone, on urinary electrolyte composition were 0.33 and 0.26, respectively, relative to spironolactone. However, since the serum concentrations of these steroids were not determined, their incomplete absorption and/or first-pass metabolism could not be ruled out as a reason for their reduced in vivo activities.
spironolactone and its metabolites are more than 90% bound to plasma proteins. The metabolites are excreted primarily in the urine and secondarily in bile. The effect of food on spironolactone absorption (two 100 mg ALDACTONE tablets) was assessed in a single dose study of 9 healthy, drug-free volunteers. Food increased the bioavailability of unmetabolized spironolactone by almost 100%. The clinical importance of this finding is not known.
Nonclinical Toxicology
- Orally administered spironolactone has been shown to be a tumorigen in dietary administration studies performed in rats, with its proliferative effects manifested on endocrine organs and the liver. In an 18-month study using doses of about 50, 150, and 500 mg/kg/day, there were statistically significant increases in benign adenomas of the thyroid and testes and, in male rats, a dose-related increase in proliferative changes in the liver (including hepatocytomegaly and hyperplastic nodules). In a 24-month study in which the same strain of rat was administered doses of about 10, 30 and 100 mg spironolactone/kg/day, the range of proliferative effects included significant increases in hepatocellular adenomas and testicular interstitial cell tumors in males, and significant increases in thyroid follicular cell adenomas and carcinomas in both sexes. There was also a statistically significant, but not dose-related, increase in benign uterine endometrial stromal polyps in females.
- A dose-related (above 30 mg/kg/day) incidence of myelocytic leukemia was observed in rats fed daily doses of potassium canrenoate (a compound chemically similar to spironolactone and whose primary metabolite, canrenone, is also a major product of spironolactone in man) for a period of one year. In two year studies in the rat, oral administration of potassium canrenoate was associated with myelocytic leukemia and hepatic, thyroid, testicular, and mammary tumors.
- Neither spironolactone nor potassium canrenoate produced mutagenic effects in tests using bacteria or yeast. In the absence of metabolic activation, neither spironolactone nor potassium canrenoate has been shown to be mutagenic in mammalian tests in vitro. In the presence of metabolic activation, spironolactone has been reported to be negative in some mammalian mutagenicity tests in vitro and inconclusive (but slightly positive) for mutagenicity in other mammalian tests in vitro. In the presence of metabolic activation, potassium canrenoate has been reported to test positive for mutagenicity in some mammalian tests in vitro, inconclusive in others, and negative in still others.
- In a three-litter reproduction study in which female rats received dietary doses of 15 and 500 mg spironolactone/kg/day, there were no effects on mating and fertility, but there was a small increase in incidence of stillborn pups at 500 mg/kg/day. When injected into female rats (100 mg/kg/day for 7 days, i.p.), spironolactone was found to increase the length of the estrous cycle by prolonging diestrus during treatment and inducing constant diestrus during a two week posttreatment observation period. These effects were associated with retarded ovarian follicle development and a reduction in circulating estrogen levels, which would be expected to impair mating, fertility, and fecundity. spironolactone (100 mg/kg/day), administered i.p. to female mice during a two week cohabitation period with untreated males, decreased the number of mated mice that conceived (effect shown to be caused by an inhibition of ovulation) and decreased the number of implanted embryos in those that became pregnant (effect shown to be caused by an inhibition of implantation), and at 200 mg/kg, also increased the latency period to mating.
Clinical Studies
Severe heart failure
- The Randomized Aldactone Evaluation Study (RALES) was a multinational, double-blind study in patients with an ejection fraction of ≤ 35%, a history of New York Heart Association (NYHA) class IV heart failure within 6 months, and class III–IV heart failure at the time of randomization. All patients were required to be taking a loop diuretic and, if tolerated, an ACE inhibitor. Patients with a baseline serum creatinine of >2.5 mg/dL or a recent increase of 25% or with a baseline serum potassium of >5.0 mEq/L were excluded.
- Patients were randomized 1:1 to spironolactone 25 mg orally once daily or matching placebo. Follow-up visits and laboratory measurements (including serum potassium and creatinine) were performed every four weeks for the first 12 weeks, then every 3 months for the first year, and then every 6 months thereafter. Dosing could be withheld for serious hyperkalemia or if the serum creatinine increased to >4.0 mg/dL. Patients who were intolerant of the initial dosage regimen had their dose decreased to one tablet every other day at one to four weeks. Patients who were tolerant of one tablet daily at 8 weeks may have had their dose increased to two tablets daily at the discretion of the investigator.
- RALES enrolled 1663 patients (3% U.S.) at 195 centers in 15 countries between March 24, 1995 and December 31, 1996. The study population was primarily white (87%, with 7% black, 2% Asian, and 4% other), male (73%), and elderly (median age 67). The median ejection fraction was 0.26. Seventy percent were NYHA class III and 29% class IV. The presumed etiology of heart failure was ischemic in 55%, and non-ischemic in 45%. There was a history of myocardial infarction in 28%, of hypertension in 24%, and of diabetes in 22%. The median baseline serum creatinine was 1.2 mg/dL and the median baseline creatinine clearance was 57 mL/min. The mean daily dose at study end for the patients randomized to spironolactone was 26 mg.
- Concomitant medications included a loop diuretic in 100% of patients and an ACE inhibitor in 97%. Other medications used at any time during the study included digoxin (78%), anticoagulants (58%), aspirin (43%), and beta-blockers (15%).
The primary endpoint for RALES was time to all-cause mortality. RALES was terminated early, after a mean follow-up of 24 months, because of significant mortality benefit detected on a planned interim analysis. The survival curves by treatment group are shown in Figure 1. Figure 1. Survival by Treatment Group in RALES
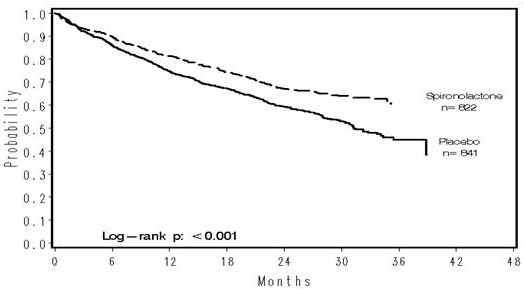
- Spironolactone reduced the risk of death by 30% compared to placebo (p<0.001; 95% confidence interval 18% to 40%). Spironolactone reduced the risk of cardiac death, primarily sudden death and death from progressive heart failure by 31% compared to placebo (p <0.001; 95% confidence interval 18% to 42%).
Spironolactone also reduced the risk of hospitalization for cardiac causes (defined as worsening heart failure, angina, ventricular arrhythmias, or myocardial infarction) by 30% (p <0.001 95% confidence interval 18% to 41%). Changes in NYHA class were more favorable with spironolactone: In the spironolactone group, NYHA class at the end of the study improved in 41% of patients and worsened in 38% compared to improved in 33% and worsened in 48% in the placebo group (p <0.001).
- Mortality hazard ratios for some subgroups are shown in Figure 2. The favorable effect of spironolactone on mortality appeared similar for both genders and all age groups except patients younger than 55; there were too few non-whites in RALES to draw any conclusions about differential effects by race. Spironolactone's benefit appeared greater in patients with low baseline serum potassium levels and less in patients with ejection fractions <0.2. These subgroup analyses must be interpreted cautiously.
Figure 2. Hazard Ratios of All-Cause Mortality by Subgroup in RALES
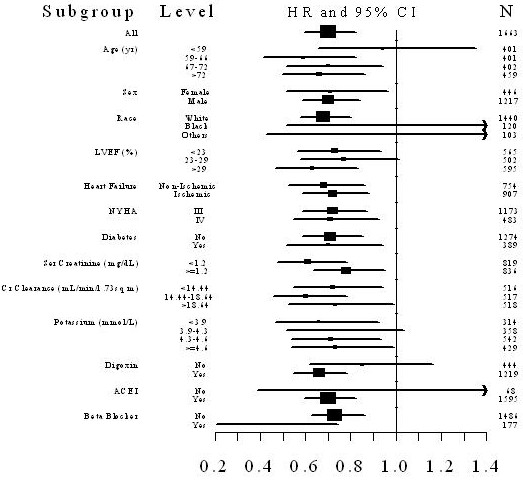
Figure 2: The size of each box is proportional to the sample size as well as the event rate. LVEF denotes left ventricular ejection fraction, Ser Creatinine denotes serum creatinine, Cr Clearance denotes creatinine clearance, and ACEI denotes angiotensin-converting enzyme inhibitor.
How Supplied
- Spironolactone tablets 25 mg are round, light yellow, film-coated, with G debossed on one side and 5011 on the other side, supplied as:
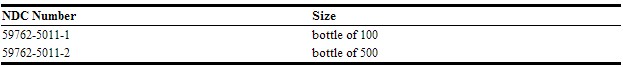
- Spironolactone tablets 50 mg are oval, light orange, scored, film-coated, with 5012 debossed on the scored side and G on the other side, supplied as:
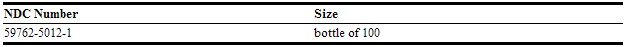
- Spironolactone tablets 100 mg are round, peach-colored, scored, film-coated, with 5013 debossed on the scored side and G on the other side, supplied as:
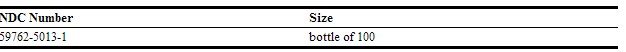
Storage
Store below 77°F (25°C).
Images
Drug Images
{{#ask: Page Name::Spironolactone |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Spironolactone |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Patients who receive spironolactone tablets should be advised to avoid potassium supplements and foods containing high levels of potassium, including salt substitutes.
Precautions with Alcohol
Concomitant with alcohol, barbiturates, or narcotics may lead to potentiation of orthostatic hypotension.
Brand Names
There is limited information regarding Spironolactone Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Spironolactone Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Vincenzi C, Trevisi P, Farina P, Stinchi C, Tosti A (1993) Facial contact dermatitis due to spironolactone in an anti-acne cream. Contact Dermatitis 29 (5):277-8. PMID: 8112074
- ↑ Hatwal A, Bhatt RP, Agrawal JK, Singh G, Bajpai HS (1988) Spironolactone and cimetidine in treatment of acne. Acta Derm Venereol 68 (1):84-7. PMID: 2449021
- ↑ Goodfellow A, Alaghband-Zadeh J, Carter G, Cream JJ, Holland S, Scully J et al. (1984) Oral spironolactone improves acne vulgaris and reduces sebum excretion. Br J Dermatol 111 (2):209-14. PMID: 6235834
- ↑ Fernández-Esparrach G, Guevara M, Sort P, Pardo A, Jiménez W, Ginès P et al. (1997) Diuretic requirements after therapeutic paracentesis in non-azotemic patients with cirrhosis. A randomized double-blind trial of spironolactone versus placebo. J Hepatol 26 (3):614-20. PMID: 9075669
- ↑ Bianchi S, Bigazzi R, Campese VM (2006) Long-term effects of spironolactone on proteinuria and kidney function in patients with chronic kidney disease. Kidney Int 70 (12):2116-23. DOI:10.1038/sj.ki.5001854 PMID: 17035949
- ↑ Schjoedt KJ, Rossing K, Juhl TR, Boomsma F, Tarnow L, Rossing P et al. (2006) Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy. Kidney Int 70 (3):536-42. DOI:10.1038/sj.ki.5001580 PMID: 16775595
- ↑ Karakurt F, Sahin I, Güler S, Demirbas B, Culha C, Serter R et al. (2008) Comparison of the clinical efficacy of flutamide and spironolactone plus ethinyloestradiol/cyproterone acetate in the treatment of hirsutism: a randomised controlled study. Adv Ther 25 (4):321-8. DOI:10.1007/s12325-008-0039-5 PMID: 18389188
- ↑ Gaby AR (1986) Idiopathic edema: 'overlooked' causes. Hosp Pract (Off Ed) 21 (2):21. PMID: 3081532
- ↑ Melby JC (1985) Idiopathic edema. A clinical conundrum. Hosp Pract (Off Ed) 20 (12):68E-68G, 68J, 68M passim. PMID: 3934201
- ↑ Hayashi M, Tsutamoto T, Wada A, Tsutsui T, Ishii C, Ohno K et al. (2003) Immediate administration of mineralocorticoid receptor antagonist spironolactone prevents post-infarct left ventricular remodeling associated with suppression of a marker of myocardial collagen synthesis in patients with first anterior acute myocardial infarction. Circulation 107 (20):2559-65. DOI:10.1161/01.CIR.0000068340.96506.0F PMID: 12732605
- ↑ Moghetti P, Castello R, Zamberlan N, Rossini M, Gatti D, Negri C et al. (1999) Spironolactone, but not flutamide, administration prevents bone loss in hyperandrogenic women treated with gonadotropin-releasing hormone agonist. J Clin Endocrinol Metab 84 (4):1250-4. DOI:10.1210/jcem.84.4.5606 PMID: 10199763
- ↑ Batista MC, Mendonça BB, Kater CE, Arnhold IJ, Rocha A, Nicolau W et al. (1986) Spironolactone-reversible rickets associated with 11 beta-hydroxysteroid dehydrogenase deficiency syndrome. J Pediatr 109 (6):989-93. PMID: 3023598
- ↑ Harry G. Brittain (26 November 2002). Analytical Profiles of Drug Substances and Excipients. Academic Press. p. 309. ISBN 978-0-12-260829-2. Retrieved 27 May 2012.
{{#subobject:
|Page Name=Spironolactone
|Pill Name=
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone label table 01.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone label table 02.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone label table 03.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone panel 01.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone panel 02.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone panel 03.jpg
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone panel 04.png
}}
{{#subobject:
|Label Page=Spironolactone |Label Name=Spironolactone panel 04.png
}}