Sideroblastic anemia pathophysiology: Difference between revisions
Nazia Fuad (talk | contribs) |
Nazia Fuad (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Sideroblastic anemia}} | {{Sideroblastic anemia}} | ||
{{CMG}} {{AE}} | {{CMG}} {{AE}} {{N.F}} | ||
==Overview== | ==Overview== | ||
Revision as of 17:35, 6 August 2018
|
Sideroblastic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sideroblastic anemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Sideroblastic anemia pathophysiology |
|
Risk calculators and risk factors for Sideroblastic anemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Nazia Fuad M.D.
Overview
| Sideroblastic anemia pathophysiology | |
 | |
|---|---|
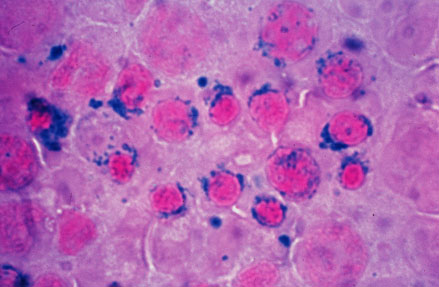
| Sideroblastic (microcytic) anemia |
Pathophysiology[1][2]
Physiology
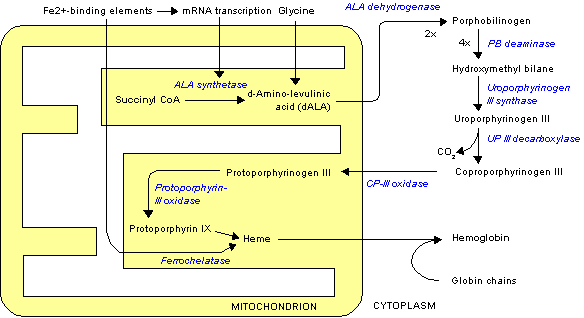
Heme is porphyrin containing compound, with an Fe iron ion in the centre,surrounded by heterocyclic organic ring of porphyrin.
The normal physiology of heme synthesis can be understood as follows:
- Mitochondria in the developing erythroid cells are the cellular site of heme production and iron utilization.
- Glycine combines with succinylcoA to form aminolenolinic acid(ALA)
- This reaction is catalyzed by ALA sunthetase enzyme (ALAS2) in mitochondria
- ALA synthetase requires vit B-6 as a cofactor
- Two molecules of aminolenolinic acid condense in cytosol to form porphobilinogen(PBG)
- This reaction is catalyzed by zinc containing enzyme called ALA dehydratase.
- Multiple enzymatic transformations in cytoplasm produce coproporphyrinogen III (CPG).
- Coproporphyrinogen III (CPG) enters the mitochondrion.
- Additional modifications of CPG in mitochondrion produces protoporphyrin IX.
- The final step is the insertion of iron into the protoporphyrin IX ring producing HEME.
- This final reaction is catalyzed by enzyme ferrochelatase.

Pathogenesis
- The exact pathogenesis of [disease name] is not completely understood.
OR
- It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics[edit | edit source]
[Disease name] is transmitted in [mode of genetic transmission] pattern.
OR
Genes involved in the pathogenesis of [disease name] include:
- [Gene1]
- [Gene2]
- [Gene3]
OR
The development of [disease name] is the result of multiple genetic mutations such as:
References
- ↑ Fujiwara T, Harigae H (December 2013). "Pathophysiology and genetic mutations in congenital sideroblastic anemia". Pediatr Int. 55 (6): 675–9. doi:10.1111/ped.12217. PMID 24003969.
- ↑ Fleming MD (2011). "Congenital sideroblastic anemias: iron and heme lost in mitochondrial translation". Hematology Am Soc Hematol Educ Program. 2011: 525–31. doi:10.1182/asheducation-2011.1.525. PMID 22160084.