Scoliosis surgery
|
Scoliosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Scoliosis surgery On the Web |
|
American Roentgen Ray Society Images of Scoliosis surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Surgery is usually indicated for curves that have a high likelihood of progression, curves that cause a significant amount of pain with some regularity, curves that would be cosmetically unacceptable as an adult, curves in patients with spina bifida and cerebral palsy that interfere with sitting and care, and curves that affect physiological functions such as breathing.
Surgery for scoliosis is usually done by an orthopaedic surgeon who specializes in spine surgery. For various reasons it is usually impossible to completely straighten a scoliotic spine, but in most cases very good corrections are achieved.
Surgery
Spinal fusion with instrumentation
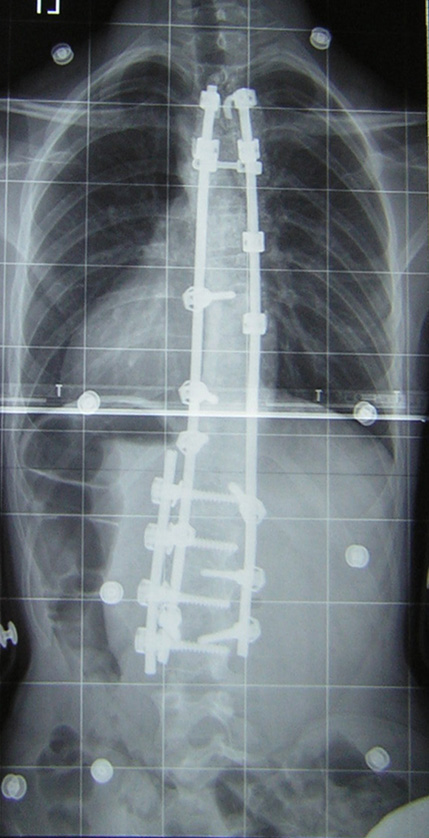
Spinal fusion is the most widely performed surgery for scoliosis. In this procedure, bone (either harvested from elsewhere in the body (autograft), or donor bone (allograft) is grafted to the vertebrae so that when it heals, they will form one solid bone mass and the vertebral column becomes rigid. This prevents worsening of the curve at the expense of spinal movement. This can be performed from the anterior (front) aspect of the spine by entering the thoracic or abdominal cavity, or performed from the back (posterior). A combination of both is used in more severe cases.
Originally, spinal fusions were done without metal implants. A cast was applied after the surgery, usually under traction to pull the curve as straight as possible and then hold it there while fusion took place. Unfortunately, there was a relatively high risk of pseudarthrosis (fusion failure) at one or more levels and significant correction could not always be achieved. In 1962, Paul Harrington introduced a metal spinal system of instrumentation which assisted with straightening the spine, as well as holding it rigid while fusion took place. The original, now obsolete Harrington rod operated on a ratchet system, attached by hooks to the spine at the top and bottom of the curvature that when cranked would distract, or straighten, the curve. A major shortcoming of the Harrington method was that it failed to produce a posture where the skull would be in proper alignment with the pelvis and it didn't address rotational deformity. As a result, unfused parts of the spine would try to compensate for this in the effort to "stand up straight". As the person aged, there would be increased "wear and tear", early onset arthritis, disc degeneration, muscular stiffness and pain with eventual reliance on painkillers, further surgery, inability to work full-time and disability. "Flatback" became the medical name for a related complication, especially for those who had lumbar scoliosis. Modern spinal systems are attempting to address sagittal imbalance and rotational defects unresolved by the Harrington rod system. They involve a combination of rods, screws, hooks and wires fixing the spine and can apply stronger, safer forces to the spine than the Harrington rod. Spinal fusion is rarely performed without this instrumentation.
Modern spinal fusions generally have good outcomes with high degrees of correction and low rates of failure and infection. Patients with fused spines and permanent implants tend to have normal lives with unrestricted activities when they are younger, it remains to be seen whether those that have been treated with the newer surgical techniques will develop problems as they age. They are able to participate in recreational athletics, have natural childbirth and are generally satisfied with their treatment. The most notable limitation of spinal fusions is that patients who have undergone surgery for scoliosis are ineligible for military service in the United States.
In cases where scoliosis has caused a significant deformity resulting in a rib hump, it is often possible to perform a surgery called a "costoplasty" (also called "thorocoplasty") in order to achieve a more pleasing cosmetic result. This procedure may be performed at any time after a fusion surgery, whether as part of the same operation or several years afterwards. As stated before, it is usually impossible to completely straighten and untwist a scoliotic spine, and it should be noted that the level of cosmetic success will depend on the extent to which the fused spine still rotates out into the ribcage. A rib hump is evidence that there is still some rotational deformity to the spine. Specific weight training techniques can be used to influence this rotational deformity in the unfused parts of the spine. This leads to a marked decrease in pain and to some improvement in organ function depending on the person's particular case and is to be recommended over any cosmetic surgical procedure.
Alternatives
Recently, new implants have been developed that aim to delay spinal fusion and to allow more spinal growth in young children. These include rods that are extendible and allow growth while still applying corrective forces and vertebral stapling which is a method of retarding normal growth on the convex side of a curve, allowing the concave side to 'catch up.' For the youngest patients, whose thoracic insufficiency compromises their ability to breathe and applies significant cardiac pressure, ribcage implants that push the ribs apart on the concave side of the curve may be especially useful. These Vertical Expandable Prosthetic Titanium Ribs (VEPTR) provide the benefit of expanding the thoracic cavity and straightening the spine in all three dimensions while allowing the spine to grow. Although these methods are novel and promising, these treatments are only suitable for growing patients. Spinal fusion remains the 'gold-standard' of surgical treatment for scoliosis. There are now non-surgical ways to help treat scoliosis, as mentioned above in the management section.