Sandbox:Javaria
Methods of Pacing
Cardiac pacemakers consist of two parts: a pulse generator or simply generator which is the source of electric pulse, and a variable number of leads that convey the electric signal from the generator to the myocardium. Newer leadless pacemakers have been introduced reducing the risk of complications. There is no formal classification system for the pacemaker. Based upon their duration of use they can be divided into temporary pacing or emergency use pacing and permanent pacing.
Temporary pacing
Temporary pacing is indicated if permanent pacing is not instantly available, not required, or contraindicated. Unlike a permanent pacemaker, the generator is placed outside the body and not implanted in the subcutaneous tissue. Different types of temporary pacing techniques (based upon the method used to consign the leads to the heart chambers) have been described in the table below.
| Types of temporary pacing | |||
|---|---|---|---|
| Type | Procedure | Use | Limitation/ Complication |
| Transvenous pacing | Under sterile conditions, a pacemaker wire guided by fluoroscopy or echocardiography is placed into a vein. Internal jugular vein or subclavian vein are the most common access sites.[1] It is then passed into either the right atrium or right ventricle. The pacing wire is then connected to an external pacemaker outside the body and appropriate mode is selected. | 1. Alternative to transcutaneous pacing and a bridge to permanent pacing. 2. Post-op injury/ trauma or temporary damage to conduction system or SA node. |
1. Infection 2. Thrombosis 3. Pneumothorax, hemothorax 4. Pericardial tamponade[2] |
| Transcutaneous pacing/ External pacing | The procedure described in: External pacing should not be relied upon for an extended period of time. | 1.Emergencies: Hemodynamically significant bradycardias, asystole, third-degree AV block[3] 2. bridge to transvenous pacing |
1. Patient discomfort 2. Risk of skin burns 3. Musculoskeletal stimulation |
| Epicardial Pacing | Temporary epicardial pacing is used during open-heart surgery should the surgical procedure create atrioventricular block. The electrodes are placed in contact with the outer wall of the ventricle to maintain satisfactory cardiac output until a temporary transvenous electrode has been inserted. | ||
| Transesophageal pacing | Two types of leads are available; pill electrode with flexible wire that can be swallowed and a flexible catheter that is introduced via nares under local anesthesia. Transesophageal pacing requires special pacing devices. Being programed for burst pacing only, esophageal stimulators are intrinsically developed as triggering systems. The addition of a programmable stimulator is required to deliver extrastilumi. | 1. Evaluation of SA node, supraventricular tachycardias and palpitations. 2. Treatment: Atrial fibrillation[4] 3. Replacement of invasive atrial pacing (Atrial proximity and safer technique) |
1. No ventricular pacing 2. Heartburn 3. Phrenic nerve stimulation[5] |
| Transthoracic pacing | |||
| Transthoracic mechanical pacing | An old procedure, also known as percussive pacing involves the use of the closed fist, usually on the left lower edge of the sternum over the right ventricle. According to the British Journal of Anesthesia Striking from a distance of 20 - 30 cm to raise the ventricular pressure 10 - 15mmHg will induce electrical activity and hence ventricular beat.[6] It is a life-saving mean until an electrical pacemaker is available. | 1.Bradyarrhythmias with hemodynamic instability or asystole[7] 2. Complete heart block with ventricular asystole |
Potential for injury due to mechanical nature and availability of better techniques limit the use. |
| Transmediastinal pacing | Also available for permanent pacing, the technique is usually used for temporary pacing. | ||
Permanent Pacing
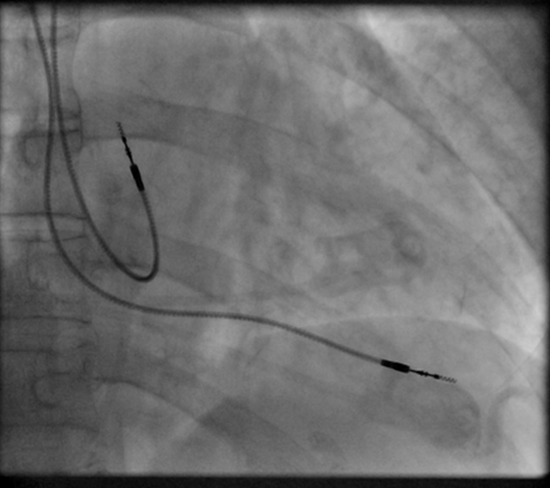
Permanent pacing with an implantable pacemaker involves the transvenous placement of one or more pacing electrodes within a chamber, or chambers, of the heart. The procedure is performed by the incision of a suitable vein into which the electrode lead is inserted and passed along the vein, through the valve of the heart, until positioned in the chamber. The procedure is facilitated by fluoroscopy which enables the physician or cardiologist to view the passage of the electrode lead. After satisfactory lodgment of the electrode is confirmed the opposite end of the electrode lead is connected to the pacemaker generator.
The pacemaker generator is a hermetically sealed device containing a power source, usually a lithium battery, a sensing amplifier which processes the electrical manifestation of naturally occurring heartbeats as sensed by the heart electrodes, the computer logic for the pacemaker and the output circuitry which delivers the pacing impulse to the electrodes.
Most commonly, the generator is placed below the subcutaneous fat of the chest wall, above the muscles and bones of the chest. However, the placement may vary on a case by case basis.
The outer casing of pacemakers is so designed that it will rarely be rejected by the body's immune system. It is usually made of titanium, which is inert in the body.
- ↑ McCann P (January 2007). "A review of temporary cardiac pacing wires". Indian Pacing Electrophysiol J. 7 (1): 40–9. PMC 1764908. PMID 17235372.
- ↑ Metkus, Thomas S.; Schulman, Steven P.; Marine, Joseph E.; Eid, Shaker M. (2019). "Complications and Outcomes of Temporary Transvenous Pacing". Chest. 155 (4): 749–757. doi:10.1016/j.chest.2018.11.026. ISSN 0012-3692.
- ↑ Doukky R, Bargout R, Kelly RF, Calvin JE (May 2003). "Using transcutaneous cardiac pacing to best advantage: How to ensure successful capture and avoid complications". J Crit Illn. 18 (5): 219–225. PMC 6376978. PMID 30774278.
- ↑ Verbeet T, Castro J, Decoodt P (October 2003). "Transesophageal pacing: a versatile diagnostic and therapeutic tool". Indian Pacing Electrophysiol J. 3 (4): 202–9. PMC 1502053. PMID 16943920.
- ↑ Roth JV (September 1996). "Phrenic nerve stimulation during transesophageal atrial pacing may cause apnea in spontaneously breathing patients". Anesth. Analg. 83 (3): 661. doi:10.1097/00000539-199609000-00054. PMID 8780310.
- ↑ (Cite_Journal)Percussion pacing in a three-year-old girl with complete heart block during cardiac catheterization. C Eich, A Bleckmann and T. Paul, retrieved from http://bja.oxfordjournals.org/cgi/content/full/95/4/465
- ↑ Eich, C.; Bleckmann, A.; Schwarz, S.K.W. (2007). "Percussion pacing—an almost forgotten procedure for haemodynamically unstable bradycardias? A report of three case studies and review of the literature". British Journal of Anaesthesia. 98 (4): 429–433. doi:10.1093/bja/aem007. ISSN 0007-0912.