Sandbox:Christina
Wikidoc
Otosclerosis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] CSN, M.D. Christina Ninan, M.D.
Synonyms and keywords: Otospongiosis
Overview
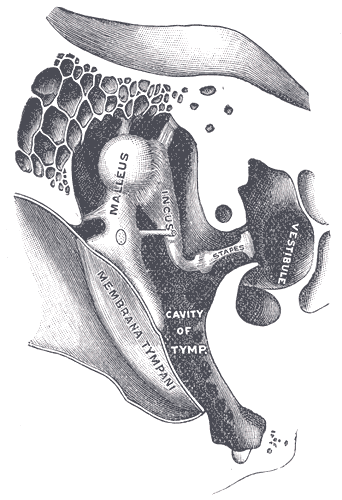
Otosclerosis is a word derived from the Greek word "sklērós" meaning hardening and oto meaning ear. Otosclerosis is an osseous dyscrasia of the otic capsule, which should be an endochondral dense bony part in the labyrinth, replaced by irregularly laid spongy bone leading to the fixation of stapes. It is one of the most common causes of conductive deafness with normal tympanic membranes. Thereby affecting sound transmission to the inner ear at the level of the oval window [1] Though majority of cases are observed at the oval window, otosclerosis can also affect the round window, cochlear apex, posterior to the oval window, posterior and anterior wall of the internal auditory canal (IAC), cochlear aqueduct, semicircular canals, and within the stapes footplate. It can be asymptomatic or in advanced cases extend into the bony labyrinth and affect cochlea which causes mixed conductive and sensorineural hearing loss depending on the position of foci. Otosclerosis is common in Caucasians and predominantly women. Hormonal fluctuations in women like during pregnancy and menopause may aggravate the disease. Many genetic factors contribute to the development of otosclerosis. And it is an autosomal dominant inheritance with incomplete penetrance. Measles was found to be one of the reasons for otosclerosis. Other factors include infammatory cytokine and cytotxic mediators secondary to inflammation.[2] (CT) scanning of the temporal bone can often demonstrate foci of demineralization in the otic capsule in cases of cochlear otosclerosis. The treatment for hearing loss is essentially stapes surgery with successful improvement of 90%-95% in the first 5 years; decreases to 63% after 30years and rarely need revision surgery. Additionally, hearing aid and cochlear implants could be used along with surgery.
Historical perspective
- 1704:Antonio Maria Valsalva identified fixation of stapes as a cause of hearing loss[3]
- 1841:Toyn bee stated, "osseous ankylosis of the stapes to the fenestra ovalis as one of the causes of deafness".[4]
- 1876:Johannes Kessel described stapes surgery as the treatment.[5]
- 1930-1950: Used Julius Lempert’s single-stage fenestration of stapes as treatment.[6]
- 1956:John Shea modernized stapedectomy.[7]
Classification
- Based on Symons/fanning grading system[8]
- Grade 1: Fenestral Otosclerosis
- Grade 2: Cochlear Otosclerosis
- Grade 2A:Basal cochlear turn Otosclerosis
- Grade 2B:Middle/Apical turn Otosclerosis
- Grade 2C:Both Basal and Middle/apical Otosclerosis
- Grade 3:Diffuse confluent cochlear involvement (with or without fenestral involvement)
Embryology
Table explains the embryological process for the development of bony labyrinth
| Gestational week | Developmental process |
|---|---|
| 4th week |
|
| 8th week |
|
| 16th week |
|
In certain cases, completion of the third stage of bone formation doesn't occur leading to cartilages between bony structures. During labyrinth bone formation, the anterior to the oval window is usually the last area to develop. This area is the most common site for otosclerosis.
Pathophysiology
Accumulation of bone deposits because of increased bone remodeling which is bone resorption followed by bone deposition in the otic capsule result in otosclerosis. Audiological findings are directly proportionate to the extent of bone remodeling.[9] Bone remodeling happens in 3 phases:
| Phase | Mechanism of action |
|---|---|
| Otospongiosis | Increase in both osteoclast activity and microvascularity |
| Transitional phase | begins with deposits of spongy bone by osteoblasts in areas of previous bone reabsorption |
| Otosclerotic phase | characterized by spongy bone deposits developing into dense bone that narrows the microcirculation previously developed in the otospongiosis phase |
The lesions occur mostly in the anterior to the oval window by calcifying of annular ligament or by involving stapes footplate (80%). While 30% of cases have the lesion at the round window,21% have it at pericochlear region, and 19% at the anterior segment of the internal auditory canal.[10]
Etiology
Though the exact cause of otosclerosis is unknown and multiple research studies are still ongoing, several etiologies are the following:
- Embryological Cause
- During the maturation of the otic capsule of the labyrinth, certain places skip the complete conversion to endochondral, leading to irregularly laid spongy bone. This most commonly is seen at fissula ante fenestram.[2]
- Genetic Cause
- Studies have been conducted and found Type 1 collagen gene(COL1A1), a component essential for bone metabolism plays a role in otosclerosis. TGF-beta 1(BMP 2 and BMP 4 gene and Angiotensin II (AGT M235T and ACE I/D genes) are also found associated with otosclerosis. Other genetic causes for otosclerosis include sex hormones, autoimmune reaction, human leucocyte antigen, inflammatory and regulatory cytokines, parathyroid hormone, and expression of parathyroid hormone-related peptides receptors, and oxidative stress[11][12][13][14]
- Gender
- Women are more likely to have otosclerosis than men , suggesting the role of sex hormones.[15]
- Ethinicity
- Otosclerosis is more common in Caucasians and Japanese compared to African populations.[16]
- Age
- Even though otosclerosis could be seen in patients at their twenties and thirties, it usually causes hearing loss only in or after their forties.
- Pregnancy
- There is no strong evidence why pregnancy worsens hearing loss in some patients with otosclerosis.However 33% women with otosclerosis are found to deteriote in hering after one pregnancy.[17]
- Measles
- RNA of measles virus was detected at the footplate of stapes in otosclerotic patients , suggesting its role in casuing it, while incidence has reduced significantly in vaccinated populations.[18]
Trauma and Major surgeries also cause otosclerosis.
- Autoimmune
- Though research on this is in the initial stages, inflammatory cytokine like TNF-alpha and cytotoxic mediators were found at the otosclerotic bone suggesting its role in the pathology.[2]
Differentiating otosclerosis from other diseases
| Conditions mimicking Otosclerosis |
|---|
|
Epidemiology and demographics
- Though a variable pattern of inheritance is observed, 60% of patients report a family with a history of otosclerosis. Thus researchers conclude this condition as an autosomal dominant with incomplete penetrance.
- Greater preponderance in women compared to men in a ratio of 2:1.[19]
- Even though the disease begins in the second and third decade of life, it doesn't result in hearing loss until the fourth decade.[20]
- Clinical prevalence of otosclerosis is found to be higher in Caucasians by 0.04%-1% while the histological incidence of otosclerosis increases to 10% in the same.[21].The incidence of histological otosclerosis is 1% and 5% in African and Asian population respectively.[22]
Risk Factors
- Genetic factor
- Otosclerosis is an autosomal dominant disease with incomplete penetrance. When 60% of patients were found with family history, 40-50% of patients have it with variable patterns of inheritance. But hearing loss in otosclerosis is found only with family history of the same.[2]
- Hormonal conditions
- Puberty, pregnancy, and menopause increase the occurrence of hearing loss in pre-existing otosclerosis.[23]
- Measles
- Persistent measles virus infection of stapes footplate results in activated osteoclast and inflammatory pathways by TNF-alpha mRNA. The protective function of osteoprotegerin at the otic capsule is inhibited by TNF-alpha and its action on RANK production[14]
Screening
Even though otosclerosis appears to be genetic deafness, early prevention can help in combating the disorder and its prevention.[24]
- Systematic Impedance-audiometry screening: The purpose of this screening is to detect a possible diphasic impedance change (on-off effect) by eliciting stapedius reflex. It is done in school going-children and helps in the early detection of stapedial fixation.
- Systematic Bone-conducted audiometry screening: It is done in young children with a family history of otosclerosis.
Natural History, complications and Prognosis
Clinical presentaion
Patients present with the following:
- Most cases are asymptomatic and diagnosed as an incidental finding in temporal autopsies.
- Bilateral(80%) or unilateral involvement earlier in the disease.[25]
- Progressive hearing loss, which might worsen with lower tone and frequencies like male voices and vowels.
- vertigo(10%) [26]
- tinnitis (50%)[26]
- Schwartz sign or flemingo's pink sign(not necessary for diagnosis): redness along the promontory of tymphanic membrane on otoscopic examination[27]
Diagnosis
Tuning fork[28]
- Pros of using a tuning fork for diagnosis:
- Negative Rinne test
- Weber test lateralizes to the ear with severe conductive loss.
- Cons of using tuning fork for diagnosis
- Rinne test cannot differentiate between sensorineural hearing loss and normal hearing loss.
- Weber test's inability to differentiate a bilateral hearing loss.
Whisper test[28]
Audiometry and tympanometry
- Caharts notch: Bone conduction depression in threshold at 2000Hz. After stapedectomy caharts notch diappears.
- Tympanometry normal at early disease. In severe cases, flattening and stiffening of curve representing low complaince of ossicular chain and tympanic membrane. Good test to differentiate between otosclerosis and pathologies with low resonance.
CT Imaging
- High resolution computed tomography (CT) of the temporal bones is the imaging technique of choice in the diagnosis of otosclerosis. [29]
- However, preoperative CT has little to add in establishing otosclerosis diagnosis and may not even be necessary to confirm diagnosis. [30]
- CT is recommended to be reserved for those patients with presumed additional abnormalities, for specific preoperative planning, or for legal necessity.[30]
- CT Finding: increased bony radiolucency in the otic capsule around the anterior footplate, thickening of the stapes, and widening of the oval window.[29]
- Early sign on CT: halo sign; demineralized area outlining the cochlea.
Treatment
- Medical Management
- Hearing aid:It is used alone or in combination with other treatments.
- Surgical Management:Stapedotomy or Stapedectomy along with placement of a prosthesis, has shown a good prognosis with improved hearing ability. Only rare cases have shown no benefit. Revision surgery is controversial but proposed for patients with no improvement of hearing loss, facial nerve damage, or persistent vertigo.Most common cause of stapedectomy failure is prosthesis displacement with or without incus erosion. Revision surgery is also recommended post surgery for patients with footplate fixation, perilymph fistula, otosclerotic regrowth. Post surgery, some are still encouraged to use a hearing aid.[33][34][35].
References
- ↑ Rajput MSA, Arain AA, Rajput AA, Adeel M, Suahil A, Awan MS (2020). "Otosclerosis: Experience With Stapes Surgery". Cureus. 12 (5): e7927. doi:10.7759/cureus.7927. PMC 7265776 Check
|pmc=value (help). PMID 32499972 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 2.3 Rudic M, Keogh I, Wagner R, Wilkinson E, Kiros N, Ferrary E; et al. (2015). "The pathophysiology of otosclerosis: Review of current research". Hear Res. 330 (Pt A): 51–6. doi:10.1016/j.heares.2015.07.014. PMID 26276418.
- ↑ Makarem AO, Hoang TA, Lo WW, Linthicum FH, Fayad JN (2010). "Cavitating otosclerosis: clinical, radiologic, and histopathologic correlations". Otol Neurotol. 31 (3): 381–4. doi:10.1097/MAO.0b013e3181d275e8. PMC 2880664. PMID 20195188.
- ↑ Nazarian R, McElveen JT, Eshraghi AA (2018). "History of Otosclerosis and Stapes Surgery". Otolaryngol Clin North Am. 51 (2): 275–290. doi:10.1016/j.otc.2017.11.003. PMID 29502722.
- ↑ Wielgosz R, Mroczkowski E (2008). "[History of endaural surgery]". Otolaryngol Pol. 62 (3): 348–50. doi:10.1016/S0030-6657(08)70269-5. PMID 18652164.
- ↑ Pietruski J (1998). "[Juliusz Lempert (1890-1959): the author of the fenestration technique]". Otolaryngol Pol. 52 (3): 341–6. PMID 9760779.
- ↑ Cheng HCS, Agrawal SK, Parnes LS (2018). "Stapedectomy Versus Stapedotomy". Otolaryngol Clin North Am. 51 (2): 375–392. doi:10.1016/j.otc.2017.11.008. PMID 29397948.
- ↑ Lee TC, Aviv RI, Chen JM, Nedzelski JM, Fox AJ, Symons SP (2009). "CT grading of otosclerosis". AJNR Am J Neuroradiol. 30 (7): 1435–9. doi:10.3174/ajnr.A1558. PMC 7051554 Check
|pmc=value (help). PMID 19321627. - ↑ Wiatr A, Składzień J, Świeży K, Wiatr M (2019). "A Biochemical Analysis of the Stapes". Med Sci Monit. 25: 2679–2686. doi:10.12659/MSM.913635. PMC 6475125. PMID 30975972.
- ↑ Arnold W (2007). "Some remarks on the histopathology of otosclerosis". Adv Otorhinolaryngol. 65: 25–30. doi:10.1159/000098665. PMID 17245019.
- ↑ Bittermann AJ, Wegner I, Noordman BJ, Vincent R, van der Heijden GJ, Grolman W (2014). "An introduction of genetics in otosclerosis: a systematic review". Otolaryngol Head Neck Surg. 150 (1): 34–9. doi:10.1177/0194599813509951. PMID 24170657.
- ↑ Van Den Bogaert K, Govaerts PJ, Schatteman I, Brown MR, Caethoven G, Offeciers FE; et al. (2001). "A second gene for otosclerosis, OTSC2, maps to chromosome 7q34-36". Am J Hum Genet. 68 (2): 495–500. doi:10.1086/318185. PMC 1235283. PMID 11170898.
- ↑ Thys M, Van Den Bogaert K, Iliadou V, Vanderstraeten K, Dieltjens N, Schrauwen I; et al. (2007). "A seventh locus for otosclerosis, OTSC7, maps to chromosome 6q13-16.1". Eur J Hum Genet. 15 (3): 362–8. doi:10.1038/sj.ejhg.5201761. PMID 17213839.
- ↑ 14.0 14.1 Karosi T, Jókay I, Kónya J, Szabó LZ, Pytel J, Jóri J; et al. (2006). "Detection of osteoprotegerin and TNF-alpha mRNA in ankylotic Stapes footplates in connection with measles virus positivity". Laryngoscope. 116 (8): 1427–33. doi:10.1097/01.mlg.0000225928.35838.e5. PMID 16885748.
- ↑ Ben Arab S, Besbes G, Hachicha S (2001). "[Otosclerosis in populations living in northern Tunisia: epidemiology and etiology]". Ann Otolaryngol Chir Cervicofac. 118 (1): 19–25. PMID 11240433.
- ↑ JOSEPH RB, FRAZER JP (1964). "OTOSCLEROSIS INCIDENCE IN CAUCASIANS AND JAPANESE". Arch Otolaryngol. 80: 256–62. doi:10.1001/archotol.1964.00750040266004. PMID 14172803.
- ↑ Gristwood RE, Venables WN (1983). "Pregnancy and otosclerosis". Clin Otolaryngol Allied Sci. 8 (3): 205–10. doi:10.1111/j.1365-2273.1983.tb01428.x. PMID 6883784.
- ↑ Niedermeyer HP, Arnold W (2008). "Otosclerosis and measles virus - association or causation?". ORL J Otorhinolaryngol Relat Spec. 70 (1): 63–9, discussion 69-70. doi:10.1159/000111049. PMID 18235207.
- ↑ Crompton M, Cadge BA, Ziff JL, Mowat AJ, Nash R, Lavy JA; et al. (2019). "The Epidemiology of Otosclerosis in a British Cohort". Otol Neurotol. 40 (1): 22–30. doi:10.1097/MAO.0000000000002047. PMC 6314447. PMID 30540696.
- ↑ Fitzgerald DC (1985). "The aging ear". Am Fam Physician. 31 (2): 225–32. PMID 3883726.
- ↑ Declau F, Spaendonck MV, Timmermans JP, Michaels L, Liang J, Qiu JP; et al. (2007). "Prevalence of histologic otosclerosis: an unbiased temporal bone study in Caucasians". Adv Otorhinolaryngol. 65: 6–16. doi:10.1159/000098663. PMID 17245017.
- ↑ Tato JM, Tato JM (1967). "Otosclerosis and races". Ann Otol Rhinol Laryngol. 76 (5): 1018–25. doi:10.1177/000348946707600512. PMID 6074235.
- ↑ Imauchi Y, Lainé P, Sterkers O, Ferrary E, Bozorg Grayeli A (2004). "Effect of 17 beta-estradiol on diastrophic dysplasia sulfate transporter activity in otosclerotic bone cell cultures and SaOS-2 cells". Acta Otolaryngol. 124 (8): 890–5. doi:10.1080/00016480310017081. PMID 15513522.
- ↑ Causse JR, Causse JB (1983). "Early detection of otosclerosis by impedance-audiometry screening". Scand Audiol Suppl. 17: 47–54. PMID 6577559.
- ↑ Thomas JP, Minovi A, Dazert S (2011). "Current aspects of etiology, diagnosis and therapy of otosclerosis". Otolaryngol Pol. 65 (3): 162–70. doi:10.1016/S0030-6657(11)70670-9. PMID 21916215.
- ↑ 26.0 26.1 Ealy M, Smith RJH (2011). "Otosclerosis". Adv Otorhinolaryngol. 70: 122–129. doi:10.1159/000322488. PMID 21358194.
- ↑ Sellari-Franceschini S, Ravecca F, De Vito A, Berrettini S (1998). "[Progressive sensorineural hearing loss in cochlear otosclerosis]". Acta Otorhinolaryngol Ital. 18 (4 Suppl 59): 59–65. PMID 10205935.
- ↑ 28.0 28.1 Bagai A, Thavendiranathan P, Detsky AS (2006). "Does this patient have hearing impairment?". JAMA. 295 (4): 416–28. doi:10.1001/jama.295.4.416. PMID 16434632. Review in: Evid Based Nurs. 2006 Oct;9(4):120 Review in: Evid Based Med. 2006 Aug;11(4):116
- ↑ 29.0 29.1 Virk JS, Singh A, Lingam RK (2013). "The role of imaging in the diagnosis and management of otosclerosis". Otol Neurotol. 34 (7): e55–60. doi:10.1097/MAO.0b013e318298ac96. PMID 23921926.
- ↑ 30.0 30.1 Wegner I, van Waes AM, Bittermann AJ, Buitinck SH, Dekker CF, Kurk SA; et al. (2016). "A Systematic Review of the Diagnostic Value of CT Imaging in Diagnosing Otosclerosis". Otol Neurotol. 37 (1): 9–15. doi:10.1097/MAO.0000000000000924. PMID 26649602.
- ↑ Uppal S, Bajaj Y, Coatesworth AP (2010). "Otosclerosis 2: the medical management of otosclerosis". Int J Clin Pract. 64 (2): 256–65. doi:10.1111/j.1742-1241.2009.02046.x. PMID 20089010.
- ↑ Quesnel AM, Seton M, Merchant SN, Halpin C, McKenna MJ (2012). "Third-generation bisphosphonates for treatment of sensorineural hearing loss in otosclerosis". Otol Neurotol. 33 (8): 1308–14. doi:10.1097/MAO.0b013e318268d1b3. PMC 3442123. PMID 22935809.
- ↑ Redfors YD, Hellgren J, Möller C (2013). "Hearing-aid use and benefit: a long-term follow-up in patients undergoing surgery for otosclerosis". Int J Audiol. 52 (3): 194–9. doi:10.3109/14992027.2012.754957. PMID 23336672.
- ↑ Bajaj Y, Uppal S, Bhatti I, Coatesworth AP (2010). "Otosclerosis 3: the surgical management of otosclerosis". Int J Clin Pract. 64 (4): 505–10. doi:10.1111/j.1742-1241.2009.02047.x. PMID 20456195.
- ↑ McElveen JT, Kutz JW (2018). "Controversies in the Evaluation and Management of Otosclerosis". Otolaryngol Clin North Am. 51 (2): 487–499. doi:10.1016/j.otc.2017.11.017. PMID 29502731.